Keywords
Pulmonary vein thromboses;ncRNA;64-MDCT;Dabigatran;SLC5A7
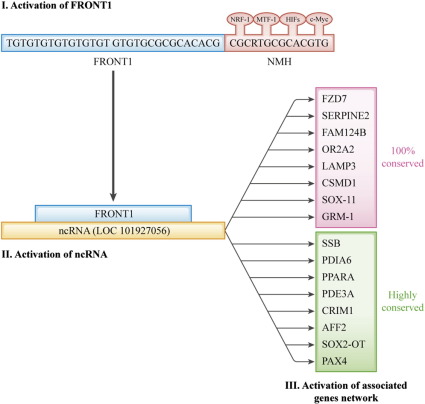
Pulmonary vein thromboses (PVTs) are believed to be rare; however, using 64-slice multidetector CT (64-MDCT), I have reported a number of cases of PVT in elderly patients with chest pains since 2012 [1]; [2]; [3]; [4]; [5]; [6]; [7]; [8]; [9] ; [10]. In 2014, I reported that 61% (35 patients) of 57 elderly patients with chest pain had PVTs [5], which suggests that PVTs are common in elderly patients with chest pain. PVTs can release microclots that can occlude the microarteries of all organs, which inhibits the supply of oxygen and nutrients by inhibiting the arterial flow. Such conditions can cause and promote heart failure and activate nuclear respiratory factor-1 (NRF-1; CGCRTGCGCR), metal responsive transcription factor-1 (MTF-1; TGCRCNC) and hypoxia inducible factors (HIFs; RCGTG). These transcription factors and c-Myc (CACGTG) might bind and co-function on CGCGTGCGCACGTG sequences, which are termed NMHs. SLC5A7 (a choline transporter) is known to be associated with heart rate variability. SLC5A7 has an NMH that is 481 Kb from the ATG start codon that contains the sequence TGTGTGTGTGTGTGT GTGTGCGCGCACACG (termed FRONT1) before the NMH. A 29-nt FRONT1 is included in the ncRNA (LOC 101927056), and a 30-nt FRONT1 is included in the near regions of genes such as FZD7 (cardiac differentiation), SERPINE2, FAM124B, OR2A2, LAMP3, CSMD1, SOX-11 and GRM1. Additionally, FRONT1 is highly conserved in Sjogren syndrome antigen B (SSB), which is associated with cardiovascular disease, PDIA6, PPARA (acute myocardial infarction), PDE3A (cardiac remodeling), CRIM1 (chronic heart failure), AFF2, SOX2-OT and PAX4 (transcriptional modulator) (Fig. 1). Some of these genes are associated with cardiovascular disease.
|
|
|
Fig. 1. Schematic overview of possible function of ncRNA (101927056) in the regulation of several gene expression levels. |
Initially, FRONT1 + NMH might be activated, and ncRNA might subsequently be activated by FRONT1. The FRONT1 of LOC 101927056 has no NMH at all. Finally, ncRNA might activate many other genes, and these genes might form a network that changes the characteristics of to survive under new hypoxic and undernourished conditions. Cardiovascular agents cannot reach the pathologic parts of the heart through occluded microvessels. I have reported some PVT cases in which warfarin [1] and dabigatran [3]; [4]; [5] ; [10] dissolved the PVTs. Warfarin and dabigatran might ameliorate cardiovascular disease by increasing microarterial blood flow. FRONT1 might be useful as a novel prognostic factor and a new target for the development of drugs for cardiovascular disease. Microclots released from PVTs might occlude small coronary arteries and cause slow flow syndrome of the coronary arteries. To clarify these relationships, additional studies are needed. It is important to use 64-MDCT to demonstrate PVTs when we estimate the effects of anticoagulants on PVTs.
Conflict of interest
The author reports no relationships that could be construed as a conflict of interest.
Acknowledgements
None.
References
- [1] H. Takeuchi; A thrombus of the right upper pulmonary vein: detection by the use of a 64-MDCT; BMJ Case Rep (Sep 14 2012) https://doi.org/10.1136/bcr.12.2011.5446 [Published online:]
- [2] H. Takeuchi; 64-MDCT showed the thrombus in the pulmonary vein of the patient with angina pectoris; BMJ Case Rep (Oct 13 2012) https://doi.org/10.1136/bcr.02.2012.5839 [Published online:]
- [3] H. Takeuchi; Floating thrombus in the left upper pulmonary vein dissolved by dabigatran; BMJ Case Rep (Oct 9 2013) https://doi.org/10.1136/bcr-2013-200836 [Published online:]
- [4] H. Takeuchi; Chest pain caused by pulmonary vein thrombi could be curable by dabigatran; BMJ Case Rep (March 13 2014) https://doi.org/10.1126/bcr-2013-203186 [Published online:]
- [5] H. Takeuchi; High prevalence of pulmonary vein thrombi in elderly patients with chest pain, which has relationships with aging associated diseases; IJC Heart Vessels, 4 (JUN-6-2014), pp. 129–134 https://doi.org/10.1016/j.ijchv.2014.05.006 [Published online:]
- [6] H. Takeuchi; Pulmonary vein thrombi in a patient with paroxysmal atrial fibrillation; IJC Heart Vasc, 5 (2014), pp. 63–64 https://doi.org/10.1016/j.ijcha.2014.10.006
- [7] H. Takeuchi; A network of pulmonary vein thrombi is a risk factor for ischemic stroke, especially after cardiac surgery: a case report and mini review; IJC Heart Vasc (2014) https://doi.org/10.1016/j.ijcha.2014.11.004
- [8] H. Takeuchi; A jumping left atrial thrombus connected to a pulmonary vein thrombus using transthoracic echocardiography and 64-slice multi-detector computed tomography; IJC Heart Vasc (2014) https://doi.org/10.1016/j.ijcha.2014.12.002
- [9] H. Takeuchi; A long and narrow pulmonary vein thrombus attached to the wall of pulmonary vein; IJC Heart Vasc (2015) https://doi.org/10.1016/j.ijcha.2015.02.011
- [10] H. Takeuchi; 64-Slice multidetector computed tomography may assess resistance of antiplatelet drugs; Int J Cardiol (2015) https://doi.org/10.1016/j.ijcme.2015.03.001
Document information
Published on 19/05/17
Submitted on 19/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?