Abstract
Background
Despite substantive growth in utilization of positron emission tomography (PET) myocardial perfusion imaging (MPI), evidence on its prognostic value is limited. We aimed to comprehensively evaluate the prognostic literature of PET perfusion measures according to the most recent American Heart Association recommendations for assessment of novel cardiovascular biomarkers.
Methods
We searched the literature for studies reporting associations of PET MPI measures and outcomes in patients with known or suspected coronary artery disease. We documented hazard ratios (HR) and 95% confidence intervals (CI) of association effects and quantitatively synthesized them with random-effects meta-analyses. Discrimination, calibration and risk reclassification after addition of PET MPI measures to standard prognostic models were documented.
Results
We identified 20 eligible studies with median n = 551 patients. In meta-analyses, the extents of ischemic and scarred myocardium were significantly associated with cardiac death. Meta-analyses of multivariate estimates for abnormal summed stress score ≥ 4 and myocardial perfusion reserve < 2 revealed significant associations with major adverse cardiovascular events [HR (95% CI) 2.30 (1.53–3.44) and 2.11 (1.33–3.36), respectively]. Changes in model discrimination, calibration or risk reclassification were reported in 5 studies (8 prognostic evaluations). There were marginal improvements in discrimination based on C index and no improvements in model calibration. Net reclassification index ranged from 9.8% to 14.2% and risk classification was significantly improved in 4/5 prognostic evaluations.
Conclusions
PET MPI measures were strongly associated with adverse patient outcomes. Risk classification was more consistently improved than discrimination and calibration after addition of PET MPI measures, but reporting of such metrics was overall limited.
Keywords
Positron emission tomography;Myocardial perfusion imaging;Prognosis;Discrimination;Calibration;Risk reclassification
1. Introduction
Positron emission tomography (PET) myocardial perfusion imaging (MPI) has emerged as an important tool in the evaluation of coronary artery disease (CAD). PET MPI offers an accurate assessment of myocardial perfusion with favorable diagnostic characteristics and is increasingly utilized. In a recent meta-analysis of 166 articles of different MPI methods, PET achieved the highest diagnostic performance, over both single-photon emission tomography (SPECT) and cardiac magnetic resonance imaging, with a pooled sensitivity of 84% and specificity 81% [1].
Beyond diagnostic performance, there is accumulating data on the prognostic significance of PET perfusion abnormalities with regard to patient outcomes [2]; [3] ; [4]. Most studies have focused on associations between MPI measures and outcomes but statistical association, even though a fundamental condition, is insufficient to establish a markers role in clinical decision-making. A clinically useful biomarker should essentially offer incremental predictive information beyond well-established risk factors and improve risk stratification with the ultimate goal of altering patient management and outcomes [5]; [6] ; [7].
In the present study we aim to map the current evidence on the prognostic value of PET MPI measures in patients with known or suspected CAD. We aim to assess the statistical significance and strength of associations with patient outcomes, and comprehensively evaluate the predictive value of PET perfusion measures according to the most recent American Heart Association (AHA) recommendations for assessment of novel cardiovascular biomarkers on the basis of discrimination ability, model calibration, and risk reclassification [5]; [8]; [9] ; [10].
2. Methods
2.1. Literature search and study eligibility
We searched MEDLINE, EMBASE, and CENTRAL using the terms positron emission tomography, myocard*, perfusion, and (prognos* OR predict*) for eligible studies without year restriction. We limited the search to English language studies in humans. Latest update search was performed on April 25, 2014. We also searched abstracts and presentations of the most recent major cardiology meetings and the clinicaltrials.gov registry for yet unpublished studies. Finally, we perused the reference lists of all eligible articles for any additional studies not identified with the above searches.
All studies were assessed for eligibility at the title and abstract level and potentially eligible ones were assessed in full text. We included prospective and retrospective studies in patients with known or suspected CAD reporting on associations of any PET MPI measure with clinical outcomes during follow-up. Such measures include summed stress score (SSS), summed rest score (SRS), summed difference score (SDS), myocardial blood flow (MBF), myocardial perfusion reserve (MPR), extent of abnormal, ischemic or scarred myocardium, and transient ischemic dilatation (TID) ratio. We acknowledged that there might exist subtle variations in techniques for acquisition of these measures but adhered to the definition provided in each study. We only focused on perfusion measures and did not consider left ventricular ejection fraction reserve among the measures of interest. We excluded studies focusing on diagnostic performance without outcome reporting; studies assessing the prognostic value of tracer uptake or perfusion-uptake mismatch measures; those evaluating prognostic factors in patients with normal PET MPI scans; studies on perfusion changes in response to cold pressor testing; studies reporting non-clinical outcomes (e.g. changes in echocardiographic measures); and studies in patients with non-ischemic cardiomyopathy. When two different studies on the same patient cohort were identified, we included the study with the longest follow-up. Literature search and study selection were performed by two investigators who reached consensus in case of discrepancies.
2.2. Data extraction and measures of prognostic value
We recorded information on imaging technique, patient enrollment period, demographics, follow-up duration, and type and number of clinical events. Outcomes of interest included all-cause death, cardiac death, myocardial infarction (MI) and the composite of major adverse cardiovascular events (MACE) as defined by each study. We extracted risk estimates with 95% confidence intervals (CI) and p-values for associations between MPI measures and the outcomes of interest. When both univariate and multivariate risk estimates were presented, we included only the latter, and among the multiple multivariate models in the same study, we kept the one with the larger number of adjusting variables. When effect estimates were not available, we documented the p-values derived from survival comparisons in different perfusion categories.
Furthermore, in order to assess how the predictive ability of models consisting of standard clinical or imaging variables improved with the addition of PET MPI measures we documented information on statistical measures proposed by the AHA for the evaluation of novel markers of cardiovascular risk [5]. These included discrimination ability, model calibration, and risk reclassification. Discrimination ability indicates how well a model differentiates those who will suffer an event from those who will not. We documented the C index and other discrimination metrics (D statistic, R2 statistic, Brier score, when available) after the addition of the PET MPI measures [9] ; [11]. Model calibration indicates how well predicted and observed risks correlate. It is quantified with goodness-of-fit statistics such as Hosmer–Lemeshow and Nam–D'Agostino [10] and we documented how these changed with the addition of PET MPI measures to the standard baseline prognostic model. Finally, a new biomarker should ideally reclassify patients in more appropriate risk categories. We documented percentages of patients correctly reclassified (upwards or downwards) and, when available, the net reclassification index (NRI), which indicates the net number of patients reclassified to the correct risk category [8] ; [12].
2.3. Statistical analysis
We report categorical variables as frequencies and percentages and continuous variables as means and standard deviations (SD) or medians and interquartile ranges (IQR). Effect size estimates of associations between the PET MPI measures and patient outcomes were pooled in meta-analyses per perfusion measure using DerSimonian–Laird random-effects models for cardiac death and MACE [13]. Estimates derived from univariate analyses were pooled separately from those of the multivariate analyses. Special consideration was made not to include results of studies with potentially overlapping populations in the same meta-analysis. Heterogeneity was assessed with the Cochrane Q statistic based on chi-square testing (statistically significant when p-value < 0.10). Its magnitude was quantified with the I2 statistic (on a scale of 0–100%, with values > 50% indicating large heterogeneity) [14]. Analyses were conducted using Stata 12.0 software (StataCorp, College Station, TX, USA). P-values are two-tailed.
3. Results
3.1. Literature search
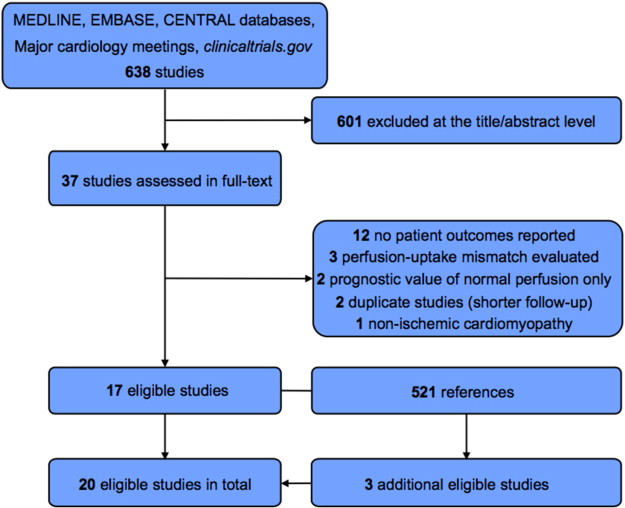
The literature search yielded a total of 620 studies that were assessed in the title and/or abstract level and 37 potentially eligible studies were assessed in full-text. Seventeen studies were deemed eligible after the exclusion of studies mainly because of lack of reporting of patient outcomes (n = 12). Another 8 studies were excluded for other reasons as shown in Fig. 1. Three additional eligible studies were identified by scrutinizing references of the eligible studies. One potentially eligible study with suspended participant recruitment and without any published results available was identified in clinicaltrials.gov. Thus, 20 studies were finally eligible. One of the included studies [15] reported on a multicenter registry and partially overlapped with 4 of the other included studies [16]; [17]; [18] ; [19]. Partial overlap potentially also existed between different single-center studies from the same institution focusing on different perfusion metrics or patient subgroups.
|
|
|
Fig. 1. Flowchart of study selection. |
3.2. Study characteristics
Studies were published over a span of 20 years (1993–2013) and 7 were prospective. Most studies (n = 15) used 82Rb as a perfusion tracer and the rest utilized 13N-ammonia or both. One study specifically evaluated patients with chronic kidney disease [20]. The median number of included patients was 551 (IQR 232–1291). The mean or median follow-up for clinical outcomes ranged from 1 to 7.3 years. Further details on the study characteristics are shown in Table 1.
| Study | Radionuclide | Study type | N patients (male) | Age, years | Follow-up, years | Outcomes (N events) | Perfusion measure |
|---|---|---|---|---|---|---|---|
| Farhad 2013 [21] | 82Rb | Prospective | 335 (139) | 64 ± 11 (no MACE) | Median 1.7 (IQR 1.5–1.9) | MACE (35) | SSS, SDS, SRS, stress MBF, MPR |
| Dorbala 2013 [15] | 82Rb | Retrospective | 7061 (3715) | 63 ± 13 | Median 2.2 (IQR 1.3–3.3) | Cardiac death (169), death (570) | % myocardium abnormal, scarred, or ischemic |
| Rischpler 2012 [30] | 82Rb | Retrospective | 265 (99) | 49 ± 9 | 2.7 ± 0.9 | Death (34) | SSS, MPR, TID ratio |
| Williams 2012 [19] | 82Rb | Retrospective | 3739 (1982) | 62 ± 13 | 5.2 ± 1.7 | Cardiac death (187), death (510) | % myocardium abnormal |
| Murthy 2012 [20] | 82Rb | Retrospective | 866 (435) | Median 71 (IQR 61–80) | Median 1.28 (IQR 0.64–2.34) | Cardiac death (88), death (155) | % myocardium abnormal, MPR |
| Fiechter 2013 [22] | 13N-ammonia | Retrospective | 621 (484) | 60 ± 12 | 5.7 ± 2.5 | Cardiac death or non-fatal MI (135), MACE (275) | Normal vs abnormal perfusion (semiquantitative scoring) |
| Fukushima 2011 [4] | 82Rb | Retrospective | 224 (86) | 58 ± 13 | 1 ± 0.8 | MACE (33) | SSS, stress MBF, MPR |
| Ziadi 2011 [18] | 82Rb | Prospective | 677 (430) | 64 ± 12 | Median 1.1 (IQR 1–1.14) | Cardiac death or MI (27), MACE (71) | SSS, MPR |
| Murthy 2011 [3] | 82Rb | Retrospective | 2783 (1333) | Median 65 (IQR 56–75) | Median 1.4 (IQR 0.7–3.2) | Cardiac death (137) | MPR |
| Slart 2011 [27] | 13N-ammonia | Retrospective | 119 (96) | 67 ± 11 | Median 7.3 (IQR NA) | Cardiac death (22), MACE (35) | MPR |
| Tio 2009 [28] | 13N-ammonia | Prospective | 480 (271) | 66 ± 11 | Median 7.1 | MACE (NA), cardiac death (60) | MPR |
| Herzog 2009 [23] | 13N-ammonia | Retrospective | 256 (69) | 60 ± 12 | 5.4 ± 2.2 | MACE (78), cardiac death (29) | SSS, MPR |
| Dorbala 2009 [17] | 82Rb | Retrospective | 1432 (675) | 63 ± NA | 1.7 ± 0.7 | MACE (83), death (140) | % myocardium abnormal, scarred, or ischemic based on SSS, SRS, or SDS, respectively |
| Chow 2009 [24] | 13N-ammonia or 82Rb | Prospective | 124 (77) | 62 ± 11 (abnormal PET) | 2.3 ± 1.6 | Cardiac death or non-fatal MI (5), MACE (16) | SSS |
| Lertsburapa 2008 [37] | 82Rb | Retrospective | 1441 (602) | 69 ± 12 (alive) | 2.7 ± 0.8 | Death (132) | SSS |
| Schenker 2008 [29] | 82Rb | Retrospective | 621 (249) | 61 ± 13 | 1.4 ± 0.6 | Death or MI (55) | SDS |
| Yoshinaga 2006 [16] | 82Rb | Prospective | 367 (168) | 59 ± 11 | 3.1 ± 0.9 | MACE (17), total cardiac events (59) | SSS |
| Marwick 1997 [26] | 82Rb | Prospective | 685 (486) | 62 ± 11 | 3.4 ± NA | MACE (151), cardiac death (81) | Summed score defects (rest and stress) categories: none, small, moderate, extensive |
| Marwick 1995 [25] | 82Rb | Retrospective | 72 (48) | 67 ± 11 | 1.5 ± 1 | Perioperative (14) and late (7) cardiac events | Rest and stress perfusion defect (sensitivity, PPV for adverse outcome) |
| Yoshida 1993 [38] | 82Rb | Prospective | 35 (22) | 54 ± NA | 3 ± 0.3 | Death (7) | Infarct size ≥ 23% myocardium |
Abbreviations: CAD, coronary artery disease; CKD, chronic kidney disease; MACE, major adverse cardiovascular events (definition varies across studies); MBF, myocardial blood flow; MI, myocardial infarction; MPR, myocardial perfusion reserve; NA, not available; PPV, positive predictive value; SDS, summed difference score; SSS, summed stress score; SRS, summed rest score; and TID, transient ischemic dilation;
“Age” and “follow-up” data are shown as mean ± standard deviation unless otherwise specified.
3.3. Evaluated outcomes and strength of prognostic associations
Semiquantitative measures showed a variable association with adverse outcomes (Supplementary Table 1). In the recent study by Fahrad et al., SDS, SSS, and SRS were all significantly associated with MACE in univariate analyses but only SDS remained significant in the multivariate analysis [21]. Fixed and reversible defects were strong predictors of adverse outcomes in the multivariate analyses in the studies by Fiechter et al. [22], Fukushima et al. [4], Herzog et al. [23], Chow et al. [24], Yoshinaga et al. [16], Marwick et al. [25] ; [26] but not in Ziadi et al. [18]. In quantitative perfusion analysis, impaired MBF and MFR were associated with MACE in all studies [3]; [4]; [18]; [21]; [23]; [27] ; [28].
Cardiac death was one of the evaluated outcomes in 8 studies with a median number of 85 events (IQR 37–161) and associations with several different perfusion measures were reported. In the largest study by Dorbala et al. [15], a 10-unit increase in the percentage of ischemic myocardium was associated with a 70% increased risk for cardiac death in univariate analysis and 34% increased risk in multivariate analysis. This was concordant to the effect observed in the Murthy et al. study (univariate HR 1.58, p < 0.001, for cardiac mortality) [3]. The SDS was also significantly predictive of hard cardiac events in two studies [21] ; [29]. SSS ≥ 4 predicted cardiac death or MI and other MACE in three studies [4]; [23] ; [24] but not in Ziadi et al. [18]. It also failed to predict all-cause mortality in the study by Rischpler et al. [30]. Age- and sex-adjusted proportional hazards analysis suggested a 4-fold increased risk for cardiac death per 1-SD decrease of MFR in the Tio et al. study [28] and MPR < 2 was associated with nearly 3-fold increased risk of cardiac death in Herzog et al. [23]. Finally, TID was reported in one study only and a ratio of > 1.13 did not predict all-cause mortality [30].
3.4. Meta-analyses of prognostic effect estimates
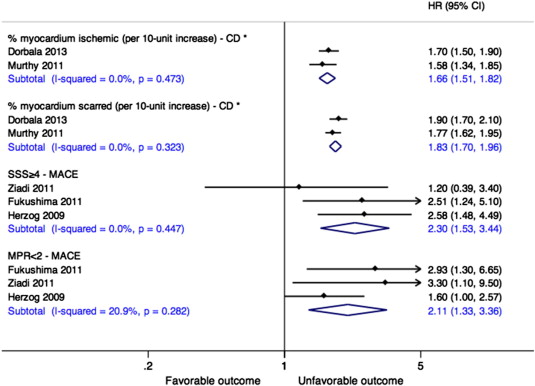
Five studies reported non-overlapping data that were suitable for inclusion in the meta-analyses. The results from the Dorbala et al. study published in 2013 [15] were not included in the same analyses with the results from four other studies [16]; [17]; [18] ; [19] due to partial overlap of patient populations. In the meta-analyses of univariate estimates, 10% increases in ischemic and scarred myocardium were associated with significant increases in cardiac death risk (summary HR 1.66, 95% CI 1.51–1.82, and HR 1.83, 1.70–1.96, respectively) (Fig. 2). Abnormal SSS and MPR were also strongly associated with MACE based on estimates from the multivariate analyses with HR (95% CI) 2.30 (1.53–3.44) and 2.11 (1.33–3.36), respectively. There was no significant heterogeneity in any of the meta-analyses (all Cochran Q p-values > 0.05 and I2 < 50%).
|
|
|
Fig. 2. Meta-analyses of associations of PET MPI measures with patient outcomes. Effect estimates are derived from multivariate analyses unless marked with * in which case estimates are derived from univariate analyses. Abbreviations: CD, cardiac death; CI, confidence interval; HR, hazard ratio; MACE, major adverse cardiovascular events; MPR, myocardial perfusion reserve; and SSS, summed stress score. |
3.5. Discrimination, calibration and risk classification
Five studies reported changes in ≥ 1 additional metric of prognostic value (discrimination, calibration, or risk classification) after inclusion of PET MPI measures to models including clinical and/or echocardiographic variables in a total of 8 prognostic evaluations (Table 2).
| Study | N patients | Outcome (N events) | Prognostic model | Perfusion measure(s) added | Prognostic metrics |
|---|---|---|---|---|---|
| Dorbala 2013 [15] | 7061 | Cardiac death (169) | Clinical covariates†, history of PCI or CABG, aspirin, beta-blockers, rest heart rate | % myocardium abnormal | C index change 0.844 → 0.875 (p = 0.05) NRI 11.6% (95% CI, 2.1%–21%) for annual risk categories < 1%, 1–2.9%, ≥ 3% |
| Murthy 2012 [20] | 866 | Cardiac death (88) | Duke clinical score, early revascularization, eGFR, rest LVEF | % myocardium abnormal | C index (95% CI) 0.75 (0.70–0.81), p = 0.17⁎ Calibration Hosmer–Lemeshow chi-square change 11.31 → 5.83, p = 0.76 |
| Duke clinical score, early revascularization, eGFR, rest LVEF, % myocardium abnormal, LVEF reserve | MPR | C index (95% CI) 0.77 (0.72–0.82), p = 0.17⁎ Calibration Hosmer–Lemeshow chi-square change 6.92 → 8, p = 0.53 NRI 14.2% (95% CI, 7.6%–21.9%) for annual risk categories < 2%, 2–4%, > 4% | |||
| Murthy 2011 [3] | 2783 | Cardiac death (137) | Clinical covariates‡, early revascularization, rest LVEF | % myocardium abnormal | C index (95% CI) 0.82 (0.78–0.86), p = 0.17⁎⁎ Calibration Nam–D'Agostino chi-square change 6.2 → 10.3, p = 0.32 |
| Clinical covariates‡, early revascularization, rest LVEF, % myocardium abnormal, LVEF reserve | MPR | C index (95% CI) 0.84 (0.80–0.87), p = 0.02⁎⁎ Calibration Nam–D'Agostino chi-square change 9.18 → 10.97, p = 0.28 NRI 9.8% (95% CI, 2.5%–18%) for annual risk categories < 1%, 1–3%, > 3% | |||
| Ziadi 2011 [18] | 677 | Cardiac death or MI (27) | SSS, history of MI, stress LVEF | MPR | NRI 11% (p = 0.092) (risk categories NA) |
| MACE (71) | SSS, demographic factors, CCS angina class, diabetes, stress LVEF | MPR | NRI 11.2% (p = 0.048) (risk categories NA) | ||
| Dorbala 2009 [17] | 1432 | Cardiac death or MI (83) | Clinical covariates, rest LVEF | % myocardium abnormal | C index change 0.79 → 0.82, p = 0.04 |
Abbreviations: CABG, coronary artery bypass graft; CCS, Canadian Cardiovascular Society; CI, confidence interval; eGFR, estimated glomerular filtration rate; LVEF, left ventricular ejection fraction; MACE, major adverse cardiovascular events; MI, myocardial infarction; MPR, myocardial perfusion reserve; NA, not available; and NRI, net reclassification improvement.
⁎. p-Value for comparison to C-statistic of model including Duke clinical score and early revascularization [0.65 (95% CI 0.59–0.71)].
⁎⁎. p-Value for comparison to C-statistic of model including clinical covariates and early revascularization [0.78 (95% CI 0.74–0.82)].
†. Age, sex, hypertension, dyslipidemia, diabetes mellitus, history of angina, smoking, BMI.
‡. Age, sex, hypertension, dyslipidemia, diabetes mellitus, family history of coronary artery disease, tobacco use, CAD, BMI, chest pain, and dyspnea.
Discrimination ability (based on the C index) for cardiac death and/or non-fatal MI improved in all 4 studies that evaluated the addition of the percentage of abnormal myocardium to baseline models but the improvement was statistically significant only in the study by Dorbala et al. in 2009 [17]. Abnormal MPR significantly improved the discrimination for cardiac mortality only in one study [3]. Hosmer–Lemeshow or Nam–D'Agostino chi-square statistics of model calibration for cardiac mortality did not improve significantly with the inclusion of any MPI measure. Finally, information on risk reclassification was reported in 4 studies. In Dorbala et al. in 2013 [15] there was a significant improvement in risk classification with the addition of the percentage of abnormal myocardium as net 11.6% of patients were reclassified to correct annual cardiac death risk categories. The inclusion of MPR in models already including a semiquantitative MPI measure also resulted in a significantly improved cardiac death risk classification in the studies by Murthy et al. (NRI 14.2% and 9.8%) [3] ; [20]. In contrast, MPR did not have a significant risk reclassification effect for cardiac death when added to a model including SSS in the study by Ziadi et al. (p = 0.092) [18]. NRI was marginally statistically significant for MACE in the same study (p = 0.048).
4. Discussion
We identified 20 studies that cumulatively provide strong evidence on associations between myocardial perfusion abnormalities and adverse outcomes in patients with known or suspected CAD. In the meta-analyses of studies with available data, 10% increases in ischemic and scarred myocardium conferred significantly increased risks of cardiac death. Abnormal SSS and reduced MPR were strongly associated with MACE in pooled analyses of univariate risk estimates. Beyond statistical significance, reporting of discrimination, calibration and risk reclassification metrics was infrequent. The addition of the percentage of abnormal myocardium or MPR to models including standard risk variables did not improve model calibration and there was only marginal or no improvement in discrimination ability. The PET MPI measures reclassified a net of 10–15% of patients to more appropriate risk categories.
The cardiovascular prognostic research agenda has been enriched in recent years with metrics assessing the impact of biomarkers on clinical decision making and outcomes rather than statistical associations alone [5] ; [31]. Statistical significance and magnitude of association between a biomarker and an outcome are essential but only suggestive of a biomarkers ultimate clinical value. In addition, the performance of a prognostic model does not necessarily improve with the incorporation of a biomarker that can predict outcomes when studied independently. A paradigm shift has occurred with the more widespread use of the C index change that quantifies the ability to better discriminate patients who will suffer adverse outcomes from those who will not, and calibration measures which indicate the agreement between predicted and observed risks. It can be argued, however, that risk reclassification may have the greatest clinical implications [8]. Frequently, clinical decisions are made on the basis of the perceived risk for adverse outcome and management dilemmas tend to be more complex in intermediate risk patients. Thus, a clinically useful marker should have a significant effect on the reclassification of patients across all risk categories, but most importantly intermediate-risk patients. In the current body of the PET MPI literature, information on discrimination and calibration was limited and argues against consistent improvements in either of these measures. Nevertheless, net reclassification was positive in all studies where this was reported which suggests that PET MPI measures can have a role in clinical decision making.
Statistical significance, magnitude of associations, improvements in discrimination, calibration, and risk classification should qualify a marker for further evaluation, ideally in randomized controlled trials. The ultimate evidence on clinical utility of a diagnostic test stems from its ability to improve outcomes when its result help determine further diagnostic and therapeutic decisions. Unfortunately, diagnostic randomized clinical trials are rather sparse in clinical medicine and tests that reach such level of scrutiny are often shown to have minimal or no effect on patient outcomes [32]. In a trial evaluating patient outcomes with F-18-fluorodeoxyglucose PET imaging, patients with severe left ventricular dysfunction and known or suspected CAD were randomized to PET-guided management vs. standard care. After 1 year of follow-up, there was no difference in the composite MACE outcome between the two arms, but there was a significant benefit in the group of patients that adhered to revascularization recommendations based on the PET findings [33]. In a post-hoc analysis of the same trial focusing on a subset of patients treated in an experienced PET center, there were significantly better outcomes with PET-guided management [34], while another analysis also showed improvement in quality of life [35]. In another trial, patients with CAD considered for revascularization underwent randomized evaluation with PET vs SPECT MPI with no difference in patient management or outcomes between the two arms [36].
Our study has limitations. First, the performance of PET MPI, including the methods of image analysis and types of radionuclide tracers, was not standardized among the studies. Second, reporting of perfusion measures, outcomes and perfusion measure increments for effect estimates was heterogeneous which prohibited the inclusion of a larger number of studies in the meta-analyses. Thus, it is difficult to draw strong conclusions based on these analyses and the results should be interpreted with caution. Finally, discrimination, calibration and risk classification measures were rather infrequently reported and meta-analysis estimates of these metrics were not possible to be derived.
In conclusion, our comprehensive evaluation of the current body of literature on the prognostic value of PET MPI reveals consistent associations between abnormal quantitative and semiquantitative perfusion measures and adverse patient outcomes. There is paucity of evidence on improvements in discrimination and calibration ability with the inclusion of PET MPI measures in prognostic models but limited data suggests that improved risk classification may be achieved which can in turn guide management decisions. The PET MPI research agenda will benefit from a more standardized reporting of prognostic techniques, perfusion measures, and outcomes, as well as evaluation of promising diagnostic strategies in randomized controlled trial settings.
The following are the supplementary data related to this article.
Table S1.
Statistical significance and magnitude of associations between PET MPI measures and patient outcomes.
Conflicts of interest
The authors report no relationships that could be construed as a conflict of interest.
References
- [1] C. Jaarsma, T. Leiner, S.C. Bekkers, H.J. Crijns, J.E. Wildberger, E. Nagel, et al.; Diagnostic performance of noninvasive myocardial perfusion imaging using single-photon emission computed tomography, cardiac magnetic resonance, and positron emission tomography imaging for the detection of obstructive coronary artery disease: a meta-analysis; J Am Coll Cardiol, 59 (2012), pp. 1719–1728
- [2] M.E. Merhige, W.J. Breen, V. Shelton, T. Houston, B.J. D'Arcy, A.F. Perna; Impact of myocardial perfusion imaging with PET and (82)Rb on downstream invasive procedure utilization, costs, and outcomes in coronary disease management; J Nucl Med, 48 (2007), pp. 1069–1076
- [3] V.L. Murthy, M. Naya, C.R. Foster, J. Hainer, M. Gaber, G. Di Carli, et al.; Improved cardiac risk assessment with noninvasive measures of coronary flow reserve; Circulation, 124 (2011), pp. 2215–2224
- [4] K. Fukushima, M.S. Javadi, T. Higuchi, R. Lautamaki, J. Merrill, S.G. Nekolla, et al.; Prediction of short-term cardiovascular events using quantification of global myocardial flow reserve in patients referred for clinical 82Rb PET perfusion imaging; J Nucl Med, 52 (2011), pp. 726–732
- [5] M.A. Hlatky, P. Greenland, D.K. Arnett, C.M. Ballantyne, M.H. Criqui, M.S. Elkind, et al.; Criteria for evaluation of novel markers of cardiovascular risk: a scientific statement from the American Heart Association; Circulation, 119 (2009), pp. 2408–2416
- [6] J.P. Ioannidis, I. Tzoulaki; What makes a good predictor?: the evidence applied to coronary artery calcium score; JAMA, 303 (2010), pp. 1646–1647
- [7] D.M. Lloyd-Jones; Cardiovascular risk prediction: basic concepts, current status, and future directions; Circulation, 121 (2010), pp. 1768–1777
- [8] M.J. Pencina, R.B. D'Agostino Sr., R.B. D'Agostino Jr., R.S. Vasan; Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond; Stat Med, 27 (2008), pp. 157–172 [discussion 207-12]
- [9] N.R. Cook; Use and misuse of the receiver operating characteristic curve in risk prediction; Circulation, 115 (2007), pp. 928–935
- [10] D.W. Hosmer, N.L. Hjort; Goodness-of-fit processes for logistic regression: simulation results; Stat Med, 21 (2002), pp. 2723–2738
- [11] K.H. Zou, A.J. O'Malley, L. Mauri; Receiver-operating characteristic analysis for evaluating diagnostic tests and predictive models; Circulation, 115 (2007), pp. 654–657
- [12] N.R. Cook, P.M. Ridker; Advances in measuring the effect of individual predictors of cardiovascular risk: the role of reclassification measures; Ann Intern Med, 150 (2009), pp. 795–802
- [13] J. Lau, J.P. Ioannidis, C.H. Schmid; Quantitative synthesis in systematic reviews; Ann Intern Med, 127 (1997), pp. 820–826
- [14] J.P. Higgins, S.G. Thompson; Quantifying heterogeneity in a meta-analysis; Stat Med, 21 (2002), pp. 1539–1558
- [15] S. Dorbala, M.F. Di Carli, R.S. Beanlands, M.E. Merhige, B.A. Williams, E. Veledar, et al.; Prognostic value of stress myocardial perfusion positron emission tomography: results from a multicenter observational registry; J Am Coll Cardiol, 61 (2013), pp. 176–184
- [16] K. Yoshinaga, B.J. Chow, K. Williams, L. Chen, R.A. deKemp, L. Garrard, et al.; What is the prognostic value of myocardial perfusion imaging using rubidium-82 positron emission tomography?; J Am Coll Cardiol, 48 (2006), pp. 1029–1039
- [17] S. Dorbala, R. Hachamovitch, Z. Curillova, D. Thomas, D. Vangala, R.Y. Kwong, et al.; Incremental prognostic value of gated Rb-82 positron emission tomography myocardial perfusion imaging over clinical variables and rest LVEF; JACC Cardiovasc Imaging, 2 (2009), pp. 846–854
- [18] M.C. Ziadi, R.A. Dekemp, K.A. Williams, A. Guo, B.J. Chow, J.M. Renaud, et al.; Impaired myocardial flow reserve on rubidium-82 positron emission tomography imaging predicts adverse outcomes in patients assessed for myocardial ischemia; J Am Coll Cardiol, 58 (2011), pp. 740–748
- [19] B.A. Williams, J.M. Dorn, M.J. LaMonte, R.P. Donahue, M. Trevisan, D.A. Leonard, et al.; Evaluating the prognostic value of positron-emission tomography myocardial perfusion imaging using automated software to calculate perfusion defect size; Clin Cardiol, 35 (2012), pp. E14–E21
- [20] V.L. Murthy, M. Naya, C.R. Foster, J. Hainer, M. Gaber, S. Dorbala, et al.; Coronary vascular dysfunction and prognosis in patients with chronic kidney disease; JACC Cardiovasc Imaging, 5 (2012), pp. 1025–1034
- [21] H. Farhad, V. Dunet, K. Bachelard, G. Allenbach, P.A. Kaufmann, J.O. Prior; Added prognostic value of myocardial blood flow quantitation in rubidium-82 positron emission tomography imaging; Eur Heart J Cardiovasc Imaging, 14 (2013), pp. 1203–1210
- [22] M. Fiechter, C. Gebhard, J.R. Ghadri, T.A. Fuchs, A.P. Pazhenkottil, R.N. Nkoulou, et al.; Myocardial perfusion imaging with 13 N-ammonia PET is a strong predictor for outcome; Int J Cardiol, 167 (2013), pp. 1023–1026
- [23] B.A. Herzog, L. Husmann, I. Valenta, O. Gaemperli, P.T. Siegrist, F.M. Tay, et al.; Long-term prognostic value of 13 N-ammonia myocardial perfusion positron emission tomography added value of coronary flow reserve; J Am Coll Cardiol, 54 (2009), pp. 150–156
- [24] B.J. Chow, O.M. Al Shammeri, R.S. Beanlands, L. Chen, R.A. deKemp, J. DaSilva, et al.; Prognostic value of treadmill exercise and dobutamine stress positron emission tomography; Can J Cardiol, 25 (2009), pp. e220–e224
- [25] T.H. Marwick, K. Shan, R.T. Go, W.J. MacIntyre, M.S. Lauer; Use of positron emission tomography for prediction of perioperative and late cardiac events before vascular surgery; Am Heart J, 130 (1995), pp. 1196–1202
- [26] T.H. Marwick, K. Shan, S. Patel, R.T. Go, M.S. Lauer; Incremental value of rubidium-82 positron emission tomography for prognostic assessment of known or suspected coronary artery disease; Am J Cardiol, 80 (1997), pp. 865–870
- [27] R.H. Slart, C.J. Zeebregts, H.L. Hillege, J. de Sutter, R.A. Dierckx, D.J. van Veldhuisen, et al.; Myocardial perfusion reserve after a PET-driven revascularization procedure: a strong prognostic factor; J Nucl Med, 52 (2011), pp. 873–879
- [28] R.A. Tio, A. Dabeshlim, H.M. Siebelink, J. de Sutter, H.L. Hillege, C.J. Zeebregts, et al.; Comparison between the prognostic value of left ventricular function and myocardial perfusion reserve in patients with ischemic heart disease; J Nucl Med, 50 (2009), pp. 214–219
- [29] M.P. Schenker, S. Dorbala, E.C. Hong, F.J. Rybicki, R. Hachamovitch, R.Y. Kwong, et al.; Interrelation of coronary calcification, myocardial ischemia, and outcomes in patients with intermediate likelihood of coronary artery disease: a combined positron emission tomography/computed tomography study; Circulation, 117 (2008), pp. 1693–1700
- [30] C. Rischpler, T. Higuchi, K. Fukushima, M.S. Javadi, J. Merrill, S.G. Nekolla, et al.; Transient ischemic dilation ratio in 82Rb PET myocardial perfusion imaging: normal values and significance as a diagnostic and prognostic marker; J Nucl Med, 53 (2012), pp. 723–730
- [31] T.J. Wang; Assessing the role of circulating, genetic, and imaging biomarkers in cardiovascular risk prediction; Circulation, 123 (2011), pp. 551–565
- [32] K.C. Siontis, G.C. Siontis, D.G. Contopoulos-Ioannidis, J.P. Ioannidis; Diagnostic tests often fail to lead to changes in patient outcomes; J Clin Epidemiol, 67 (2014), pp. 612–621
- [33] R.S. Beanlands, G. Nichol, E. Huszti, D. Humen, N. Racine, M. Freeman, et al.; F-18-fluorodeoxyglucose positron emission tomography imaging-assisted management of patients with severe left ventricular dysfunction and suspected coronary disease: a randomized, controlled trial (PARR-2); J Am Coll Cardiol, 50 (2007), pp. 2002–2012
- [34] A. Abraham, G. Nichol, K.A. Williams, A. Guo, R.A. deKemp, L. Garrard, et al.; 18F-FDG PET imaging of myocardial viability in an experienced center with access to 18F-FDG and integration with clinical management teams: the Ottawa-FIVE substudy of the PARR 2 trial; J Nucl Med, 51 (2010), pp. 567–574
- [35] T. Shukla, G. Nichol, G. Wells, R.A. deKemp, R.A. Davies, H. Haddad, et al.; Does FDG PET-assisted management of patients with left ventricular dysfunction improve quality of life? A substudy of the PARR-2 trial; Can J Cardiol, 28 (2012), pp. 54–61
- [36] H.M. Siebelink, P.K. Blanksma, H.J. Crijns, J.J. Bax, A.J. van Boven, T. Kingma, et al.; No difference in cardiac event-free survival between positron emission tomography-guided and single-photon emission computed tomography-guided patient management: a prospective, randomized comparison of patients with suspicion of jeopardized myocardium; J Am Coll Cardiol, 37 (2001), pp. 81–88
- [37] K. Lertsburapa, A.W. Ahlberg, T.M. Bateman, D. Katten, L. Volker, S.J. Cullom, et al.; Independent and incremental prognostic value of left ventricular ejection fraction determined by stress gated rubidium 82 PET imaging in patients with known or suspected coronary artery disease; J Nucl Cardiol, 15 (2008), pp. 745–753
- [38] K. Yoshida, K.L. Gould; Quantitative relation of myocardial infarct size and myocardial viability by positron emission tomography to left ventricular ejection fraction and 3-year mortality with and without revascularization; J Am Coll Cardiol, 22 (1993), pp. 984–997
Document information
Published on 19/05/17
Submitted on 19/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?