Summary
A primary aneurysm in the saphenous vein is very rare. This case study is based on a 55-year-old male patient who applied for general surgery with a complaint of swelling in his left inguinal area, after examinations led to a provisional diagnosis of inguinal hernia. It was decided that surgery was the best option due to the risk of thromboembolism, and pain caused by the condition itself. Confusion with inguinal hernia can affect prognosis. It increases the risk of thromboembolism as well as preventing the chance of early response.
Keywords
aneurysmal dilatation;inguinal hernia;saphenous vein aneurysm;vascular mass
1. Introduction
A primary aneurysm in the saphenous vein is rare. It is deemed to be a life-threatening condition because of the risk of suffering a pulmonary embolism. Venous aneurysms were first identified in autopsy studies by Osler in 1915. Venous aneurysms can be caused by: trauma, inflammation, connective tissue deformations, and degenerative changes.1 ; 2 Most small saphenous vein aneurysms are caused by valve failures and chronic venous insufficiency. Venous aneurysms often occur in columns and in extremities.3 This case presentation draws attention to the longstanding confusion between saphenous vein aneurysms and inguinal hernias.
2. Case report
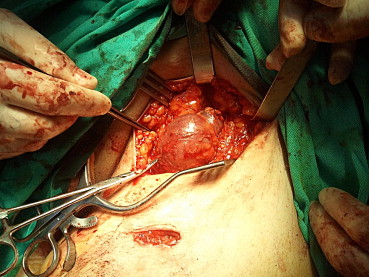
A 55-year-old male patient applied for general surgery because of extensive inguinal swelling in his left inguinal area. As a result of examinations, vascular pathology was detected and a consultation was held at our clinic. Assuming that the swelling was an inguinal hernia, the patient had not consulted a doctor for several years. A nonpulsatile swelling, which contracted through the use of compression, and became agitated through coughing and strain was identified in the left inguinal region of the patient, who had applied to the clinic because of increased pain and swelling in the past 3 months. There was no trauma, infection or inflammatory disease in his medical history. His results for electrocardiography, echocardiography, routine biochemistry, and blood analysis were normal. He had a stent placement in his right coronary artery 6 months previously. A saccular saphenous vein aneurysm in the saphenofemoral junction of the left inguinal region, and a stage III insufficiency throughout the saphenous trace were detected on Doppler ultrasonography. No signs of a thrombus were detected in the aneurysm. As a result of the high level of pain caused by the condition and the potential risk of thromboembolism, it was decided that surgery was the best option. Under spinal anesthesia, an oblique incision was made to the left inguinal and the saphenofemoral junction was localized (Fig. 1). A clamp was placed in the junction in order to prevent the occurrence of thromboembolism. The saphenous vein was separated from the junction and the junction was covered with 5/0 prolene. The saphenous vein was stripped and the aneurysm found was measured at 7 cm × 4 cm (Fig. 2). The patient, who did not experience any postoperative complications, was discharged from the clinic on his second day of recovery. No problem was detected on his 3-month and 6-month follow-up examinations and his Doppler ultrasonography showed no abnormalities.
|
|
|
Figure 1. Giant saphenous venous aneurysm in the area of the left saphenofemoral junction. |
|
|
|
Figure 2. After excision, measured saphenous venous diameter was 7 cm × 4 cm. |
3. Discussion
Primary venous aneurysms are morphologically divided into two subgroups as saccular and fusiform. Venous aneurysms can occur in many parts of the body. The aneurysms in the inguinal area are frequently confused with inguinal hernias.4
Patients often complain about pain, edema, and a gradual increase in swelling. Despite displaying the same symptoms in our patient, the confusion of the aneurysm with an inguinal hernia was an important factor in our prognosis.
Doppler ultrasonography and venography are used for diagnosing venous diseases. When there is a thrombus inside the aneurysmal sac of a venous aneurysm, the use of venography is insufficient because it is unable to display the aneurysm and its diameter. Venous Doppler ultrasonography is more effective in detecting the presence of a thrombus, and determining the diameter of an aneurysm.
Histologically, varicose enlargement and saphenous vein aneurysms are similar to each other; both involve intimal thickening and weakened or deficient smooth muscle tissue.5 ; 6
It is very important to make a distinction between superficial and deep venous system aneurysms. This is because there is a higher chance of observing a thromboembolism in deep venous system aneurysms. The higher frequency of pulmonary embolisms experienced in deep venous systems in comparison to superficial venous systems is most likely a result of the discharges that occur in the former, which are caused by the strong contractions of the muscular venous pump.7 Focal peripheral neuropathy has also been reported as a complication of venous aneurysms.
Venous aneurysms can be operated on using many methods, such as ligation, simple excision, excision and patch with the autologous vein, or complete resection. Tangential aneurysmectomy and lateral venorrhaphy are safe and preferred methods that are used for treating saccular aneurysms.8 Endovenous lasers, endovenous radiofrequency, and sclerotherapy are alternative methods of treatment but they are not as commonly used or preferred due to the size of the aneurysm and localization.
In conclusion, aneurysms that are localized in the inguinal region can be perceived as hernias and as a result can be neglected. These aneurysms may result in the occurrence of a thrombus, thromboembolism, pulmonary embolisms, and ruptures, and as such should be operated on as soon as possible.
References
- 1 H. Ekim, V. Kutay, M. Tuncer, U. Gultekin; Management of primary venous aneurysms; Saudi Med J, 25 (2004), pp. 303–307
- 2 G. Reggina, S. Rizzo, G. Impedova; Aneurysm of external jugular vein: case report and review of literature–a case report; Angiology, 108 (1992), pp. 92–95
- 3 S.G. Friedman, K.V. Krishnasastry, W. Doscher, S.L. Deckoff; Primary venous aneurysms; Surgery, 108 (1990), pp. 92–95
- 4 D.L. Gillespie, J.L. Villavicencio, C. Gallagher, et al.; Presentation and management of venous aneurysms; J Vascular Surgery, 26 (1997), pp. 845–852
- 5 C. Sessa, P. Nicolini, M. Perrin, I. Farah, J. Magne, H. Guidicelli; Management of symptomatic and asymptomatic popliteal venous aneurysms: a retrospective analysis of 25 patients and review of literature; J Vasc Surg, 32 (2000), pp. 902–912
- 6 M.A. Wali, M. Dewan, R.A. Eid; Histopathologic changes in the wall of varicose veins; Int Angiol, 22 (2003), pp. 188–193
- 7 C. Irwin, A. Synn, L. Kraiss, Q. Zhang, M.M. Griffen, G.C. Hunter; Metalloproteinase expression in venous aneurysms; J Vasc Surg, 48 (2008), pp. 1278–1285
- 8 G.A. Ranero-Juárez, R.H. Sánchez-Gómez, S.E. Loza-Jalil, A.M. Cano-Valdéz; Venous aneurysms of the extremities: report of 4 cases and review of literature; Angiology, 56 (2005), pp. 475–481
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?