Summary
Henoch-Schönlein purpura (HSP) is a systemic vasculitis characterized by a classic tetrad of nonthrombocytopenic palpable purpura, arthritis, gastrointestinal, and renal involvement. The most common gastrointestinal complaint is abdominal pain. The characteristic endoscopic findings are ulcers seen in the second portion of the duodenum. We present the case of a 45-year-old man suffering from abdominal pain. Erythematous purpura over bilateral lower extremities and soreness of the joints developed 3 days before abdominal pain. An abdominal computed tomography showed an edematous change of the intestinal wall and the distal part of the ileum. A retrograde single balloon enteroscopy revealed several discrete ulcers and hyperemic mucosa in the distal ileum. The middle, proximal, and terminal ileum and ileocecal valve to the rectum were not affected. Under the impression of HSP, nonsteroidal anti-inflammatory drugs and prednisolone were administered. We concluded that balloon-assisted enteroscopy is helpful for differential diagnosis of small bowel lesions in adult patients with HSP.
Keywords
Abdominal pain ; Enteroscopy ; Henoch-Schönlein purpura ; Ileal ulcers ; Skin rash
Introduction
Henoch-Schönlein purpura (HSP) is a common, self-limiting, systemic vasculitis affecting both children and adults. The estimated annual incidence of HSP is 3–26.7/100,000 for children and 0.8–1.8/100,000 for adults [1] . The clinical manifestations and severity of HSP are different among adults and children. HSP etiology is unclear and is usually associated with infections (including bacterial and viral) and medication [1] ; [2] ; [3] . HSP is a clinical diagnosis, but may need histologic confirmation when atypical presentation occurs.
Clinical diagnosis is established by a characteristic symmetric nonthrombocytopenic palpable purpura, gastrointestinal/renal involvement, and arthritis. Skin manifestation consisting of erythematous macular wheels or palpable purpura with petechiae is the most common presentation. Classic purpuras are symmetrically distributed in dependent areas such as the lower extremities and buttocks. Abdominal pain is the most common gastrointestinal related complaint and other symptoms include nausea, melena and hematochezia. These symptoms are secondary to mesenteric vasculitis. Intussusception, ischemic bowel, intestinal perforation, and gastrointestinal bleeding may also occur. Skin manifestation usually occurs before abdominal complications. Joint involvement is symmetrical in distribution and involves the knees and ankles. It is more commonly seen in adults than in children. Hematuria and proteinuria are common manifestations of HSP nephritis which resolve spontaneously, only 5% of patients progress to chronic end-stage renal disease at 5 years follow-up [2] .
According to the new criteria proposed by the European League Against Rheumatism (EuLAR) and Pediatric Rheumatology Society (PReS) 2006, diagnosis requires the mandatory criterion of palpable purpura plus at least one of the following: (1) diffuse abdominal pain, (2) IgA deposition in any biopsy, (3) arthritis/arthralgia, or (4) renal involvement (hematuria and/or proteinuria). However, diagnosis of HSP in adult patients is sometimes difficult when clinical manifestation is obscure and inconclusive, especially for those without dermatological signs or with mid-gut involvement.
Case report
The patient involved in this case was a 45-year-old male office worker who had a history of gastric ulcers 6 years previously and suffered from severe epigastric dull pain 3 days prior to index admission. Moreover, he had several erythematous papules and macules over bilateral lower extremities with joint soreness 3 days before the development of abdominal pain (Fig. 1 ). He also had a sore throat 2 weeks prior to this episode.
|
|
|
Figure 1. Several erythematous papules and macules over the bilateral lower extremities. |
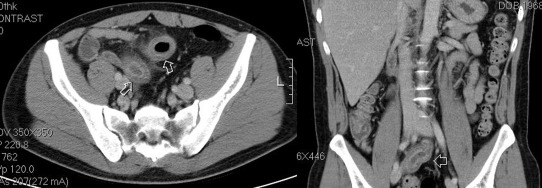
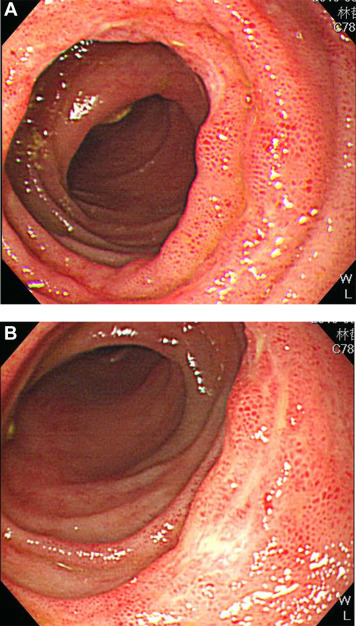
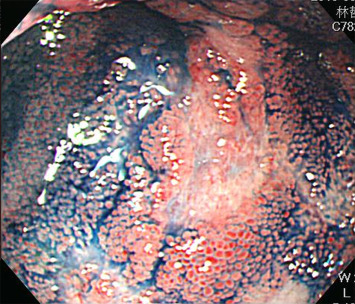
An esophagogastroduodenoscopy (EGD) showed erosive esophagitis, Los Angeles classification Grade A, and gastritis over antrum. An abdominal computed tomography (CT) showed an edematous change of the intestinal wall and the distal part of the ileum (Fig. 2 ). Empiric antibiotics with ciprofloxacin were prescribed for possible ileitis. A retrograde single balloon enteroscopy (SIF-260, Olympus Medical Systems, Tokyo, Japan) revealed several 0.5–1.5 cm discrete shallow ulcers and hyperemic mucosa at the distal ileum. The middle, proximal, and terminal ileum and the ileocecal valve to the rectum were not affected (Fig. 3 ). Chromoendoscopy with 0.2% indigo carmine dye demonstrated edematous hyperemic intestinal villi (Fig. 4 ). An endoscopic biopsy specimen of ileal ulcers showed chronic inflammation. The creatinine level was 76.9 μmol/L (normal range 61.88–106.08 μmol/L). The platelet level was 379 × 103 /μL (normal range 150–450 × 103 /μL).
|
|
|
Figure 2. An abdominal computed tomography shows edematous changes to the intestinal wall and the distal part of the ileum. |
|
|
|
Figure 3. A retrograde single balloon enteroscopy reveals several discrete 0.5–1.5 cm ulcers and hyperemic mucosa at the distal ileum. |
|
|
|
Figure 4. Chromoendoscopy with 0.2% indigo carmine dye demonstrates edematous hyperemic intestinal villi. |
In response to the diagnosis of HSP, nonsteroidal anti-inflammatory drugs (NSAIDs), prednisolone and colchicine were administered. Abdominal pain and arthralgia improved 10 days later and the skin rash disappeared gradually.
Discussion
HSP usually presents with a classic tetrad of skin purpura, poly-arthralgia, abdominal pain, and renal disease. Gastrointestinal symptoms include periumbilical and colicky pain, abdominal pain, occult blood loss, colorectal bleeding, nausea, vomiting, diarrhea, constipation, and abdominal distension [4] . Rare findings include intestinal perforation, ischemic vasculitis, intussusception, pseudomembranous colitis, pancreatitis, acute acalculous cholecystitis, appendicitis, and bowel necrosis [4] .
Regarding gastrointestinal involvement in HSP, the small intestine is the most frequently affected site, in particular the second portion part of the duodenum. In the lower gastrointestinal tract, lesions are more common in the rectum and the ileum. Lesions present more severely in the ileum than in other areas [2] . Image studies consist of abdominal X-ray film, abdominal echography, abdominal CT, and stool occult blood test. A gross mucosal thickening of the intestine on CT scan may indicate intramural hemorrhage with fluid accumulation in the wall due to vasculitis, which is frequently observed in HSP patients [5] . Endoscopic examinations are also important and include EGD, colonoscopy, small bowel barium radiogram, and enteroscopy. Otherwise, laparotomy can be performed in approximately 10% of patients when the above examinations show normal results [4] . The characteristic endoscopic findings include ulcers, edematous and diffuse erythematous mucosa, skin hyperemia or small ring-like ecchymotic lesions, hemorrhagic erosions and stricture. The ulcers are small, superficial, multiple, irregular, and clean-based [2] ; [4] .
There are few case reports of adult-onset HSP involving mid-gut (including jejunum to distal ileum) and colon. The diagnosis of gastrointestinal involvement in the small bowel is difficult. Endoscopically identified small bowel lesions are rare. Most of these cases were demonstrated by video capsule endoscopy (VCE) and colonoscopy. VCE findings include petechia/redness and erosions/ulcers. The petechia is sometimes referred to as intestinal purpura [6] . One case report of jejunal ischemia revealed by conventional upper endoscopy (approach via gastrojejunostomy) showed severe segmental ischemia of the efferent loop [7] . One VCE of a 32-year-old man with HSP showed extensive mucosal inflammation throughout the entire small bowel (duodenojejunoileitis) with redness, swelling and ulcerations [8] . Since 1980, few adult cases of HSP involving the terminal ileum have been proven by colonoscopy [9] . The endoscopic manifestation of the mid-gut in patients with HSP has not been reported by enteroscopy previously.
HSP spontaneously disappears without treatment in 94% of children and 89% of adults. The average duration of symptoms is 4 weeks. Symptomatic treatment with acetaminophen and NSAIDs is sufficient for skin rash and arthritis. Oral steroids are indicated for severe systemic manifestations, including severe colicky abdominal pain, skin rash and edema, renal involvement as proteinuria, and mesenteric vasculitis. Steroids can decrease the edema of the intestinal wall and improve gastrointestinal symptoms within 2 days compared with 12.3 days in patients without steroid treatment [2] . Some case reports demonstrate that colchicine can be used in the treatment of HSP [10] .
In summary, we presented a case of adult-onset HSP involving distal ileum and diagnosed by balloon-assisted enteroscopy. Our patient fits typical descriptions of HSP, including palpable purpura, abdominal pain, and arthritis. Typical endoscopic findings in the distal ileum included multiple shallow ulcers with hyperemic edematous mucosa. Gastrointestinal tract involvement in HSP patients is sometimes difficult to determine endoscopically, balloon-assisted enteroscopy is helpful for differential diagnosis of small bowel lesions in adult patients with HSP.
Conflicts of interest
All authors declare no conflicts of interest.
References
- [1] M. Piram, A. Mahr; Epidemiology of immunoglobulin A vasculitis (Henoch-Schonlein): current state of knowledge; Curr Opin Rheumatol, 25 (2) (2013), pp. 171–178
- [2] A.B. Sohagia, S.G. Gunturu, T.R. Tong, H.I. Hertan; Henoch-schonlein purpura-a case report and review of the literature; Gastroenterol Res Pract, 2010 (2010), p. 597648
- [3] E.C. Ebert; Gastrointestinal manifestations of Henoch-Schonlein Purpura; Dig Dis Sci, 53 (8) (2008 Aug), pp. 2011–2019
- [4] A. Hamzaoui, W. Melki, O. Harzallah, L. Njim, R. Klii, S. Mahjoub; Gastrointestinal involvement revealing Henoch Schonlein purpura in adults: report of three cases and review of the literature; Int Arch Med, 4 (1) (2011), p. 31
- [5] J.I. Shin, J.S. Lee; Indications of capsule endoscopy in Henoch-Schonlein syndrome with gastrointestinal symptoms; Am J Med, 120 (6) (2007), p. e13
- [6] R. Ichikawa, N. Hosoe, H. Imaeda, K. Takabayashi, R. Bessho, Y. Ida, et al.; Evaluation of small-intestinal abnormalities in adult patients with Henoch-Schonlein purpura using video capsule; Endoscopy, 43 (Suppl. 2) (2011), pp. E162–E163 UCTN
- [7] E.H. Kim, B.H. Park, J.W. Lim, S.W. Jung; Late diagnosis of Henoch-Schonlein purpura following detection of jejunal ischemia on conventional endoscopy; Endoscopy, 44 (Suppl. 2) (2012), pp. E393–E394 UCTN
- [8] E. Skogestad; Capsule endoscopy in Henoch-Schonlein purpura; Endoscopy, 37 (2) (2005), p. 189
- [9] R. Karagozian, C. Turbide, A. Szilagyi; Henoch-Schonlein purpura presenting with ileal involvement in an adult; Dig Dis Sci, 49 (10) (2004), pp. 1722–1726
- [10] F.T. Saulsbury; Successful treatment of prolonged Henoch-Schonlein purpura with colchicine; Clin Pediatr, 48 (8) (2009), pp. 866–868
Document information
Published on 15/05/17
Submitted on 15/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?