Summary
Background
Magnetic resonance (MR) enterography has emerged as a new imaging modality in evaluating patients with Crohns disease. However, whether interpretations of MR enterography findings are consistent among radiologists has not yet been fully investigated. The purpose of this study is to evaluate the intraobserver and interobserver agreement for identifying extraluminal manifestations of Crohns disease with MR enterography.
Methods
MR enterography was performed with a 3-tesla system. We retrospectively enrolled patients with Crohns disease that had MR enterography between November 2011 and March 2013. Three radiologists reviewed the images independently. Extraluminal findings of these patients were recorded and described. Intraobserver and interobserver agreement were calculated using the kappa statistic.
Results
A total of 22 sessions of MR enterography were performed on 15 patients (12 men and 3 women) with Crohns disease. The mean age was 38.7 ± 11.4 years. We identified extraluminal manifestations such as engorged vasa recta, enlarged mesenteric lymph nodes, fibrofatty proliferation, fistulas, and abscesses. In addition, avascular necrosis of the femoral head as a complication of long-term steroid treatment was also depicted. The intraobserver agreement was almost perfect (κ = 0.83; p < 0.001), and the interobserver agreement was substantial (κ = 0.65; p < 0.001).
Conclusion
MR enterography is a clinically useful tool for evaluating extraluminal manifestations of Crohns disease with good intraobserver and interobserver agreement.
Keywords
Crohns disease ; Inflammatory bowel disease ; Magnetic resonance imaging
Introduction
Crohns disease is a chronic relapsing inflammatory process of the gastrointestinal tract, which usually begins in young adulthood and persists throughout life. It most commonly involves the distal ileum, and is characterized by intestinal ulcerations in discontinuous segments, transmural inflammation, and penetrating and stricturing complications [1] .
It is important to recognize extraluminal manifestations of Crohns disease because these conditions may cause significant morbidities. These include disease-related mesenteric changes, such as engorged vasa recta, fibrofatty proliferation of the mesentery, and lymphadenopathy; penetrating complications such as fistulas and abscesses; and extraintestinal manifestations of the disease itself, such as uveitis, pyoderma gangrenosum, primary sclerosing cholangitis, and ankylosing spondylitis [2] .
Cross-sectional imaging techniques are useful and complementary to endoscopy in the assessment of the disease extent of Crohns disease. Magnetic resonance (MR) enterography is an emerging imaging tool, which requires orally administered enteral contrast agents, an antiperistaltic medication, and fast imaging sequences [3] ; [4] . The unique advantages of MR enterography include clear soft tissue delineation and freedom from radiation hazards. MR enterography has high sensitivity and specificity in evaluating Crohns disease (per patient sensitivity of 93%; per patient specificity of 90–92.8%) [5] ; [6] , and can be used to assess disease extent and activity, detect perianal disease, evaluate complications, and monitor treatment response [7] ; [8] . MR enterography is especially helpful in evaluating extraluminal involvement of Crohns disease [9] ; [10] , to which endoscopic examinations have limited access.
However, whether the interpretations of MR enterography findings are consistent among radiologists has not yet been fully investigated. In this study, we summarized our experience in identifying extraluminal manifestations of Crohns disease with MR enterography, and determined the intra- and interobserver agreement.
Methods
Participants
Between November 2011 and March 2013, we retrospectively enrolled adult patients with an established diagnosis of Crohns disease that had MR enterography. The diagnosis of Crohns disease was made according to clinical, endoscopic, radiological, and pathological findings. Patients who were younger than 20 years or had indeterminate colitis were excluded. The hospital institutional review board had approved this retrospective study, and the requirement to obtain informed consent was waived.
MR enterography protocol
MR enterography was performed with a 3-tesla system (MAGNETOM Verio, Siemens Medical Solutions, Erlangen, Germany). Patients were instructed to have nothing per os for 4 hours before examination, and drink 1500–2000 mL of a 2.5%-mannitol solution as an enteric contrast ∼90 minutes before examination. Intravenous hyoscine-N -butylbromide (20 mg, Buscopan; Boehringer Ingelheim Espana, S.A., Barcelona, Spain) was injected to halt peristalsis of the intestines, in order to minimize motion artifacts on the images.
The range of image acquisition included the abdomen and pelvic cavity, from the diaphragm to the anus. Breath holding was essential. We utilized the pulse sequences indicated in Table 1 . Volumetric interpolated breath-hold examination (VIBE) sequences were acquired before and 20 seconds, 50 seconds, and 80 seconds after an intravenous administration of gadolinium chelate, 0.3 mL/kg body weight (gadodiamide, 0.5 mmol/mL; GE Healthcare AS, Oslo, Norway; or gadoterate meglumine, 0.5 mmol/mL; Guerbet, Villepinte, France).
| Plane | Slice thickness (mm) | FOV (mm) | TR/TE (ms) | Flip angle | |
|---|---|---|---|---|---|
| T2-HASTE | Coronal | 5 | 300 × 300 | 1200/97 | 160 |
| T2-HASTE | Axial | 5 | 300 × 300 | 1600/99 | 160 |
| T2-HASTE with fat saturation | Axial | 5 | 300 × 300 | 1600/99 | 160 |
| VIBE | Coronal | 1.2–1.4 | 450 × 450 | 3.16/1.08 | 9 |
| FLASH 2D | Axial | 5 | 300 × 300 | 140/3.69 | 70 |
FLASH = fast low-angle shot; FOV = field of view; MR = magnetic resonance; T2-HASTE = T2-weighted half-Fourier single-shot turbo spin-echo; TE = echo time; TR = repetition time; VIBE = volumetric interpolated breath-hold examination.
Image interpretation
The images were independently reviewed by three radiologists (I.L.S., C.C.C., and K.L.L., who had 8 years, 9 years, and 15 years of experience, respectively, in a medical center with ∼1500 abdominal MR readings per radiologist per year). The radiologists were aware of the established diagnosis of Crohns disease in these patients, but were blinded to the clinical records and the original image report. All of the extraluminal manifestations related to Crohns disease, such as engorged vasa recta (increased conspicuity of the vasa recta in the affected intestinal loop compared with other unaffected segments), enlarged mesenteric lymph nodes (long axis > 1 cm, or < 1 cm but clustered), fibrofatty proliferation (increased mesenteric fat adjacent to the affected intestinal loop), fistulas, abscesses, osseous findings (such as sacroiliitis), and biliary tract abnormalities (such as cholelithiasis, bile duct stricture, and autoimmune pancreatitis), were identified and recorded. Image findings were considered positive if more than two of the three radiologists had recognized them. In order to calculate the intraobserver agreement, one of the radiologists (I.L.S.) had reviewed the images again, 2 months after the initial review.
Statistical analysis
We used the kappa statistic to measure the intraobserver and interobserver agreement. Intraobserver agreement was calculated using the results from two chronologically separate readings from the same radiologist for all the images. Interobserver agreement was calculated using the results of the three radiologists, using multi-rater kappa statistic. Furthermore, we calculated image-specific intra- and interobserver agreement according to seven specific extraintestinal findings, including engorged vasa recta, enlarged mesenteric lymph nodes, fibrofatty proliferation, fistulas, abscesses, osseous findings, and biliary tract abnormalities. A kappa (κ) > 0.8 denotes almost perfect agreement, κ = 0.8–0.6 denotes substantial agreement, κ = 0.6–0.4 denotes moderate agreement, κ = 0.4–0.2 denotes fair agreement, and κ = 0.2–0 denotes slight agreement; however, κ < 0 denotes poor agreement [11] . The analysis was performed using Small Stata 11 (StataCorp LP, College Station, TX, USA).
Results
In this study, there were a total of 22 MR enterography sessions performed for evaluating 15 patients with Crohns disease, including 12 men and three women. The mean age was 38.7 ± 11.4 years. Some of the patients had more than one MR enterography session during this period, including up to four sessions for one patient, three sessions for another patient, and two sessions for two patients.
Image findings
Extraluminal manifestations were common, and all 15 patients had at least one extraluminal finding. Five of the patients had two findings, two patients had three findings, and four patients had four findings. Table 2 summarizes the extraluminal manifestations of these patients. The most common extraluminal finding was enlarged mesenteric lymph nodes, which were identified in all of the patients. Other findings included engorged vasa recta, fibrofatty proliferation, fistulas, abscesses, and osseous findings. No definite biliary tract abnormality was identified.
| Age (y) | Sex | Enlarged mesenteric lymph nodes | Engorged vasa recta | Fibrofatty proliferation | Fistulas | Abscesses | Osseous findings | Biliary tract findings | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 62 | M | + | − | − | − | − | − | − |
| 2 | 35 | M | + | − | − | − | − | − | − |
| 3 | 24 | M | + | − | − | − | − | − | − |
| 4 | 43 | F | + | − | − | − | − | − | − |
| 5 | 28 | M | + | + | − | − | − | − | − |
| 6 | 58 | M | + | + | − | − | − | − | − |
| 7 | 44 | M | + | + | − | − | − | − | − |
| 8 | 45 | F | + | + | − | − | − | − | − |
| 9 | 30 | M | + | − | − | + | − | − | − |
| 10 | 36 | M | + | + | + | − | − | − | − |
| 11 | 48 | M | + | + | − | + | − | − | − |
| 12 | 25 | M | + | + | + | + | − | − | − |
| 13 | 40 | F | + | + | + | − | − | + | − |
| 14 | 28 | M | + | + | − | + | + | − | − |
| 15 | 35 | M | + | − | − | + | + | + | − |
| Subtotal | 15 | 9 | 3 | 5 | 2 | 2 | 0 | ||
F = female; M = male.
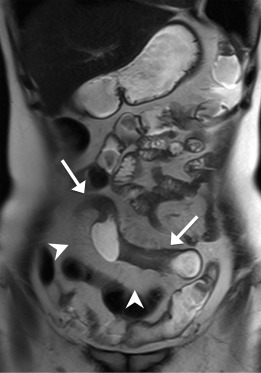
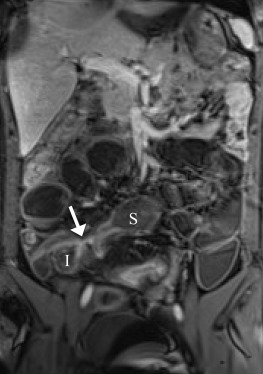
Enlarged mesenteric lymph nodes were most clearly seen on the postcontrast VIBE images, presenting as ovoid or lobulated nodular lesions between the mesenteric vessels (Figure 1 ). Engorged vasa recta were often identified adjacent to an active inflamed intestinal loop and were also best demonstrated on the postcontrast VIBE images (Figure 2 ). Fibrofatty proliferation was best seen on the coronal T2-weighted half-Fourier single-shot turbo spin-echo (T2-HASTE) images that presented as increased mesenteric fat surrounding the affected intestinal loops (Figure 3 ). Fistula tracts were often identified between an inflamed bowel and adjacent structures, showing tethering of the two structures with a contrast-enhanced fistula tract between them (Figure 4 ). Meanwhile, abscesses often manifested as fluid collections with a high signal on T2-HASTE images and well-enhanced walls on the postcontrast VIBE images (Figure 5 ).
|
|
|
Figure 1. A 36-year-old man. Coronal postcontrast VIBE image shows several enhancing enlarged lymph nodes on the mesentery (arrows). VIBE = volumetric interpolated breath-hold examination. |
|
|
|
Figure 2. The same patient as in Figure 1 . Coronal postcontrast VIBE image shows an active inflamed ileal segment in the right lower abdomen (arrows), with wall-thickening and increased enhancement. There are prominent engorged adjacent mesenteric vessels (arrowheads). VIBE = volumetric interpolated breath-hold examination. |
|
|
|
Figure 3. A 40-year-old woman. Coronal T2-HASTE image shows skipped disease-involved ileal segments with abnormal wall-thickening (arrows). There is increased amount of the adjacent mesenteric fat (arrowheads), indicating fibrofatty proliferation. T2-HASTE = T2-weighted half-Fourier single-shot turbo spin-echo. |
|
|
|
Figure 4. A 25-year-old man. Coronal postcontrast VIBE image shows affected tethering segments of ileum (I) and sigmoid colon (S), with an enhancing fistula tract (arrow) between them. VIBE = volumetric interpolated breath-hold examination. |
|
|
|
Figure 5. A 35-year-old man. Coronal postcontrast VIBE image shows multiple mesenteric abscesses, with well-enhancing walls. VIBE = volumetric interpolated breath-hold examination. |
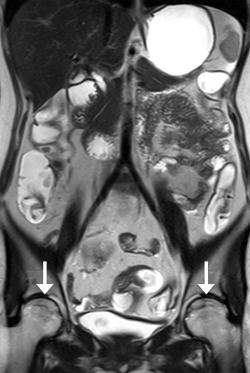
No definite inflammatory spondyloarthropathy (such as sacroiliitis) was identified in this study. Interestingly, avascular necrosis of the femoral head was identified in two patients, despite the lack of clinical symptoms. One of the patients had imaging with MR enterography four times during this study period for monitoring the treatment response. Avascular necrosis was identified since the third MR enterography session, which showed serpiginous lines over the superior portion of the bilateral femoral heads (Figure 6 ). This might relate to her long-term steroid usage for treatment of repeated flare-ups.
|
|
|
Figure 6. The same patient as in Figure 3 . Coronal T2-HASTE image shows hypointense irregular serpiginous lines over the superior portion of bilateral femoral heads (arrows). The femoral heads are preserved without collapse, suggesting Stage II avascular necrosis. T2-HASTE = T2-weighted half-Fourier single-shot turbo spin-echo. |
Intraobserver and interobserver agreement
The intraobserver agreement of the same radiologist was almost perfect, with κ = 0.83 (p < 0.001), whereas the interobserver agreement among the three radiologists was substantial, with κ = 0.65 (p < 0.001; Table 3 ). The image-specific intraobserver and interobserver agreement are also listed in Table 3 . The intraobserver agreement was almost perfect for detecting fistulas, osseous findings, abscesses, and fibrofatty proliferation (all κ = 1; p < 0.001), and a moderate agreement in detecting engorged vasa recta (κ = 0.59; p = 0.002). For the interobserver agreement, there was almost perfect agreement for detecting fistulas (κ = 1; p < 0.001), substantial agreement for osseous findings (κ = 0.74; p < 0.001) and abscesses (κ = 0.63; p < 0.001), and moderate agreement in fibrofatty proliferation (κ = 0.49; p < 0.001). There was only a slight interobserver agreement for detecting engorged vasa recta, with κ = 0.02, without statistical significance (p = 0.45).
| Intraobserver | Interobserver | |||
|---|---|---|---|---|
| Kappa | p | Kappa | p | |
| Overall agreement | 0.83 | < 0.001 | 0.65 | < 0.001 |
| Image-specific agreement | ||||
| Fistula | 1.00 | < 0.001 | 1.00 | < 0.001 |
| Osseous findings | 1.00 | < 0.001 | 0.74 | < 0.001 |
| Intraabdominal abscess | 1.00 | < 0.001 | 0.63 | < 0.001 |
| Fibrofatty proliferation | 1.00 | < 0.001 | 0.49 | < 0.001 |
| Engorged vasa recta | 0.59 | 0.002 | 0.02 | 0.45 |
| Enlarged mesenteric lymph nodes | NA a | NA a | NA a | NA a |
| Biliary tract findings | NA b | NA b | NA b | NA b |
The kappa statistic may be unreliable if one classification category dominates.
MR = magnetic resonance.
a. NA not applicable due to positive findings in all 15 patients.
b. NA not applicable due to negative findings in all 15 patients.
As discussed in the literature, a limitation of the kappa statistic is that it depends strongly on the distribution of categorical results among observation samples. It may be unreliable if one classification category dominates, and a very low kappa value may not necessarily reflect low agreement [12] ; [13] . Enlarged mesenteric lymph nodes were detected in all 15 patients, whereas no biliary tract abnormality was detected in any patient. Therefore, the kappa statistic was not applicable for these two image findings (NA a and NA b , Table 3 ). The percentage of agreement among the three radiologists was 63.6% (14 of 22 MR studies) for enlarged mesenteric lymph nodes and 95.5% (21 of 22 MR studies) for biliary tract findings.
The interobserver agreement for detecting fistula was excellent (κ = 1). However, this result only represented the reliability for detecting the presence of fistulas, and we further analyzed the agreement for the locations of the fistulas. There were five patients who were identified as having fistulas. Three of them had ileoileal fistulas, and two of them had ileocolonic fistulas, which were recognized by the three radiologists without any disagreement regarding the location. However, in one of the patients with an ileocolonic fistula, one of the radiologists pointed out an additional ileoileal fistula.
Discussion
To date, there is limited evidence regarding the intra- and interobserver agreement for evaluating the extraluminal manifestations of Crohns disease with MR enterography, especially in a 3-tesla system. In this study, there was almost perfect intraobserver agreement and substantial interobserver agreement for detecting the extraluminal manifestations with MR enterography. Our study indicates that MR enterography is a precise and reliable tool.
Moreover, when we looked into the image-specific agreement, we found excellent agreement for detecting fistulas and good agreement for detecting intraabdominal abscesses that is important because these two findings may alter subsequent treatment strategies. Several studies have evaluated the interobserver agreement for extraluminal findings with MR enterography in a 1.5-tesla system [14] ; [15] ; [16] . Siddiki et al [14] found a substantial agreement for identifying penetrating diseases (κ = 0.62), and Fiorino et al [15] reported a high interobserver agreement (100%) for detecting fistulas. These results are comparable to our study. However, some uncertainty in detecting fistulas and abscesses were reported by Jensen et al [16] . Nevertheless, we found a moderate interobserver agreement for fibrofatty proliferation and a low agreement for engorged vasa recta, probably because of a lack of clear quantifiable definitions among the radiologists. Similarly, Jensen et al [16] found a low agreement for creeping fat (κ = 0.39). However, Siddiki et al [14] reported a high agreement for engorged vasa recta (κ = 0.9–1), which differs from the result of our study. More studies in the future may be needed to clarify these inconsistent findings.
Detecting extraluminal manifestations with MR enterography is important for the comprehensive assessment of patients with Crohns disease. These image findings can aid in diagnosis, help in assessing disease activity, and may alter the treatment plan of these patients. Mesenteric lymphadenopathy is a common finding in patients with Crohns disease. It is assumed to be reactive because of intestinal inflammation. The degree of contrast enhancement on MRI is shown to be an indicator of disease activity in Crohns disease [17] ; [18] . Engorged vasa recta often presents adjacent to an active inflamed intestinal segment, which is known as the “comb sign” [3] . These two findings are helpful in evaluating the degree of active inflammation in the intestines.
Fibrofatty proliferation of the mesentery is known as creeping fat, which is demonstrated by increased abdominal fat surrounding the affected intestinal segment. It is assumed to be secondary to intestinal inflammation, but a recent study indicated that it may have an active role by secreting proinflammatory substances [19] .
Fistulas and abscesses are important penetrating complications in Crohns disease. MRI has high sensitivity (76%) and specificity (96%) for detecting fistulas, with a comparable accuracy as that of CT, and a better accuracy than that of a small bowel follow-though study [6] ; [20] . The sensitivity (75–100%) and specificity (91–100%) of MRI for detecting intraabdominal abscesses are also high [7] . Detection of an intraabdominal abscess is important before starting immunosuppressive or biologic therapies, such as infliximab [9] and adalimumab. CT and MRI have similar accuracy in the diagnosis of intestinal inflammation and extraluminal complications of patients with Crohns disease [5] ; [20] . However, the most important advantage of MRI is the lack of ionizing radiation. As these patients are relatively young and often require multiple image studies to monitor disease status and complications, MRI would be a good choice for them.
Patients with Crohns disease may receive accumulated doses of steroids during their lifelong disease course, a condition that places them at a higher risk of avascular necrosis of the bones. The hips are the most commonly affected joints, followed by the knees and shoulders [21] . The early stages of these conditions are usually asymptomatic, but pain may occur as the disease progresses; eventually, the femoral head may collapse and cause secondary osteoarthritis. Early diagnosis and treatment may prevent collapse and reduce the chance for joint replacement. A study described the ability of computed tomography (CT) enterography for the detection of avascular necrosis in patients with Crohns disease [22] . However, MRI is the most sensitive imaging technique for diagnosing avascular necrosis [23] . A study described the typical MRI findings of avascular necrosis in patients with inflammatory bowel disease [24] . However, the MR protocol is for the femoral heads, and the intestines cannot be evaluated using the same protocol. Our study is the first to emphasize the capability and importance of detecting avascular necrosis of the femoral heads in MR eneterography.
Our study had several limitations: (1) the prevalence of Crohns disease in East Asia is low [1] and the number of patients was limited. Several important extraluminal manifestations, such as primary sclerosing cholangitis and ankylosing spondylitis, were not identified in our patients; and (2) most of the image findings illustrated in this study were not confirmed by other examinations or surgery. To avoid the image readers subjective observations, the result of this study was based on the independent readings of three radiologists. In addition, because of the small number of patients and no definite gold standard, the sensitivity and specificity were not calculated in this study.
In conclusion, MR enterography is a clinically useful tool for the evaluation of the extraluminal involvement of Crohns disease, including enlarged mesenteric lymph nodes, engorged vasa recta, fibrofatty proliferation, fistulas, abscesses, and avascular necrosis of the femoral head. Our study showed almost perfect intraobserver and substantial interobserver agreement among the radiologists.
Conflicts of interest
All authors have no conflicts of interest to declare.
References
- [1] J. Cosnes, C. Gower-Rousseau, P. Seksik, A. Cortot; Epidemiology and natural history of inflammatory bowel diseases; Gastroenterology, 140 (2011), pp. 1785–1794
- [2] C.N. Bernstein, J.F. Blanchard, P. Rawsthorne, N. Yu; The prevalence of extraintestinal diseases in inflammatory bowel disease: a population-based study; Am J Gastroenterol, 96 (2001), pp. 1116–1122
- [3] J.R. Leyendecker, R.S. Bloomfeld, D.J. DiSantis, G.S. Waters, R. Mott, R.E. Bechtold; MR enterography in the management of patients with Crohn disease; Radiographics, 29 (2009), pp. 1827–1846
- [4] R. Sinha, R. Verma, S. Verma, A. Rajesh; MR enterography of Crohn disease: part 1, rationale, technique, and pitfalls; AJR Am J Roentgenol, 197 (2011), pp. 76–79
- [5] K. Horsthuis, S. Bipat, R.J. Bennink, J. Stoker; Inflammatory bowel disease diagnosed with US, MR, scintigraphy, and CT: meta-analysis of prospective studies; Radiology, 247 (2008), pp. 64–79
- [6] J. Panes, R. Bouzas, M. Chaparro, V. Garcia-Sanchez, J.P. Gisbert, B. Martinez de Guerenu, et al.; Systematic review: the use of ultrasonography, computed tomography, and magnetic resonance imaging for the diagnosis, assessment of activity and abdominal complications of Crohns disease; Aliment Pharmacol Ther, 34 (2011), pp. 125–145
- [7] G. Fiorino, C. Bonifacio, A. Malesci, L. Balzarini, S. Danese; MRI in Crohns disease—current and future clinical applications; Nat Rev Gastroenterol Hepatol, 9 (2012), pp. 23–31
- [8] J.G. Fletcher, J.L. Fidler, D.H. Bruining, J.E. Huprich; New concepts in intestinal imaging for inflammatory bowel diseases; Gastroenterology, 140 (2011), pp. 1795–1806
- [9] S. Mazziotti, A. Blandino, E. Scribano, M. Gaeta, A. Mileto, W. Fries, et al.; MR enterography findings in abdominopelvic extraintestinal complications of Crohns disease; J Magn Reson Imaging, 37 (2013), pp. 1055–1063
- [10] E.A. Smith, J.R. Dillman, J. Adler, V.L. Dematos-Maillard, P.J. Strouse; MR enterography of extraluminal manifestations of inflammatory bowel disease in children and adolescents: moving beyond the bowel wall; AJR Am J Roentgenol, 198 (2012), pp. W38–W45
- [11] J.R. Landis, G.G. Koch; The measurement of observer agreement for categorical data; Biometrics, 33 (1977), pp. 159–174
- [12] A.J. Viera, J.M. Garrett; Understanding interobserver agreement: the kappa statistic; Fam Med, 37 (2005), pp. 360–363
- [13] P.E. Crewson; Reader agreement studies; AJR Am J Roentgenol, 184 (2005), pp. 1391–1397
- [14] H.A. Siddiki, J.L. Fidler, J.G. Fletcher, S.S. Burton, J.E. Huprich, D.M. Hough, et al.; Prospective comparison of state-of-the-art MR enterography and CT enterography in small-bowel Crohns disease; AJR Am J Roentgenol, 193 (2009), pp. 113–121
- [15] G. Fiorino, C. Bonifacio, L. Peyrin-Biroulet, F. Minuti, A. Repici, A. Spinelli, et al.; Prospective comparison of computed tomography enterography and magnetic resonance enterography for assessment of disease activity and complications in ileocolonic Crohns disease; Inflamm Bowel Dis, 17 (2011), pp. 1073–1080
- [16] M.D. Jensen, T. Ormstrup, C. Vagn-Hansen, L. Ostergaard, S.R. Rafaelsen; Interobserver and intermodality agreement for detection of small bowel Crohns disease with MR enterography and CT enterography; Inflamm Bowel Dis, 17 (2011), pp. 1081–1088
- [17] N. Gourtsoyiannis, N. Papanikolaou, J. Grammatikakis, G. Papamastorakis, P. Prassopoulos, M. Roussomoustakaki; Assessment of Crohns disease activity in the small bowel with MR and conventional enteroclysis: preliminary results; Eur Radiol, 14 (2004), pp. 1017–1024
- [18] S. Gourtsoyianni, N. Papanikolaou, E. Amanakis, L. Bourikas, M. Roussomoustakaki, J. Grammatikakis, et al.; Crohns disease lymphadenopathy: MR imaging findings; Eur J Radiol, 69 (2009), pp. 425–428
- [19] L. Peyrin-Biroulet, M. Chamaillard, F. Gonzalez, E. Beclin, C. Decourcelle, L. Antunes, et al.; Mesenteric fat in Crohns disease: a pathogenetic hallmark or an innocent bystander?; Gut, 56 (2007), pp. 577–583
- [20] S.S. Lee, A.Y. Kim, S.K. Yang, J.W. Chung, S.Y. Kim, S.H. Park, et al.; Crohn disease of the small bowel: comparison of CT enterography, MR enterography, and small-bowel follow-through as diagnostic techniques; Radiology, 251 (2009), pp. 751–761
- [21] G. Klingenstein, R.N. Levy, A. Kornbluth, A.K. Shah, D.H. Present; Inflammatory bowel disease related osteonecrosis: report of a large series with a review of the literature; Aliment Pharmacol Ther, 21 (2005), pp. 243–249
- [22] D.H. Bruining, H.A. Siddiki, J.G. Fletcher, W.J. Tremaine, W.J. Sandborn, E.V. Loftus Jr.; Prevalence of penetrating disease and extraintestinal manifestations of Crohns disease detected with CT enterography; Inflamm Bowel Dis, 14 (2008), pp. 1701–1706
- [23] M.D. Mitchell, H.L. Kundel, M.E. Steinberg, H.Y. Kressel, A. Alavi, L. Axel; Avascular necrosis of the hip: comparison of MR, CT, and scintigraphy; AJR Am J Roentgenol, 147 (1986), pp. 67–71
- [24] N. Kamata, N. Oshitani, M. Sogawa, H. Yamagami, K. Watanabe, Y. Fujiwara, et al.; Usefulness of magnetic resonance imaging for detection of asymptomatic osteonecrosis of the femoral head in patients with inflammatory bowel disease on long-term corticosteroid treatment; Scand J Gastroenterol, 43 (2008), pp. 308–313
Document information
Published on 15/05/17
Submitted on 15/05/17
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?