- Data presented in part at the annual meeting of the European Society of Veterinary Oncology, Krakow, Poland 2015.
Abstract
Optimal chemotherapy protocols for high-risk mast cell tumours (MCTs) are unknown. The purpose of this study was to determine the tolerability and toxicity profile of a rapidly escalating vinblastine and prednisolone protocol (VPP) in which 3.00 mg/m2 was administered once 7 days apart: at day 14 and at day 21. Dogs with chemotherapy-naïve MCTs presenting to the Oncology Service of a single institution were prospectively enrolled to receive escalating vinblastine, and haematology and a standardised quality-of-life questionnaire were assessed prior to each dosage. Thirty-four dogs were included: 30 with microscopic disease treated with adequate local therapy and four with macroscopic disease. Of 220 doses of vinblastine administered, 4% were associated with grade 3 and 4 toxicity. A total of 70% of dogs tolerated 3.00 mg/m2 given 7 days apart at day 14 and 21, although 29% of dogs developed dose-limiting toxicities and 8% discontinued the protocol due to toxicity. In conclusion, VPP was well-tolerated overall, although prior to further dose intensity optimisation, it is important to determine if dose intensity is linked to outcome in canine MCT to avoid unwarranted toxicity.
Introduction
Mast cell tumours (MCTs) represent one of the most common tumours in the dog, accounting for 16–21% of all cutaneous tumours (Bostock 1986). MCTs are heterogeneous in nature with marked variation in biological behaviour (Patnaik et al. 1984). Current treatment paradigms suggest that adequate local treatment with surgery or a combination of surgery and definitive intent radiation therapy (RT) is the treatment of choice, although adjuvant systemic treatment is commonly recommended for high-risk MCTs (Blackwood et al. 2012). High-risk MCTs are commonly considered to include grade III Patnaik tumours, high grade Kiupel tumours, recurrent MCTs, ≥stage II tumours or tumours arising in specific locations (such as scrotum or mucous membranes) (Baginski et al. 2014; Blackwood et al. 2012; Cahalane et al. 2006b; Murphy et al. 2006; Patnaik et al. 1984; Sfiligoi et al. 2005; Thamm et al. 2006).
Vinblastine is a vinca-alkaloid extracted from the periwinkle plant (Catharanthus roseus) (Golden & Langston 1988; Rowinsky 2011; William et al. 1975). It is cell cycle specific and binds tubulin to inhibit microtubule formation during mitosis (Golden & Langston 1988; Rowinsky 2011; William et al. 1975). The dose-limiting toxicity (DLT) of vinblastine is neutropenia, with a neutrophil nadir occurring approximately 1 week after drug administration (Golden & Langston 1988; Rowinsky 2011; William et al. 1975). In veterinary medicine, although efficacy has been demonstrated for various types of neoplasia, it is most often used as adjunctive treatment for canine MCTs (Arnold et al. 2011; Bailey et al. 2008; Crow 1977; Davies et al. 2004; Rassnick et al. 2008; Singh et al. 1996; Thamm et al. 1999, 2006; Trumel et al. 2005; Vickery et al. 2008). Vinblastine can be prescribed either as a single agent when local treatment is not an option, or as adjuvant systemic therapy to adequate local control in high-risk canine MCTs (Crow 1977; Davies et al. 2004; Rassnick et al. 2008; Thamm et al. 1999, 2006; Trumel et al. 2005; Vickery et al. 2008).
Chemotherapy is generally dosed near each drugs maximally tolerated dose in order to optimise tumour cell kill (Frei & Canellos 1980; Madewell & Theilen 1979). Previous work has demonstrated the importance of dose–response relationships and dose intensity, defined as chemotherapy dose per unit time, in improving the outcomes of cancer (Budman et al. 1998; Chabner 2011; Frei & Canellos 1980; Kwak et al. 1990; Loibl et al. 2011; Lyman 2009; Norton 1997; Wudhikarn et al. 2015). For tumours considered potentially curable in humans, there is convincing evidence supporting the relevance of delivered dose intensity, and it has been suggested that dose intensity is a quality of care indicator in clinical oncology (Lyman 2009; Norton 1997). In canine lymphoma, dogs which developed grade 3 or 4 neutropenia following chemotherapy demonstrated improved outcomes, raising the possibility that more appropriate individual dosing was administered (Sorenmo et al. 2010; Vaughan et al. 2007).
A commonly used and well-tolerated protocol in dogs with high grade or metastatic MCTs, which was initially empirically extrapolated without phase I data in dogs, consists of eight doses of vinblastine at a dosage of 2 mg/m2. The first four doses are given weekly, followed by four doses given every other week (Crow 1977; Davies et al. 2004; Rassnick et al. 2008; Thamm et al. 1999, 2006; Trumel et al. 2005; Vickery et al. 2008). Prednisolone is administered concurrently, as it significantly enhances efficacy compared to vinblastine alone (Stanclift & Gilson 2008). One study evaluating this protocol reported severe adverse effects in only 5% of dogs, suggesting that dogs may tolerate a higher dosage of vinblastine (Thamm et al. 1999). In the last decade, several studies have attempted a dosage optimisation for vinblastine in dogs.
In a phase I dose escalation trial of vinblastine, the maximally tolerated dose for vinblastine was 3.50 mg/m2 every other week. However, grade 4 toxicity, as graded according to Veterinary Cooperative Oncology Group Common Terminology Criteria for Adverse Effects v 1.1 (VCOG CTCAE), was common (Bailey et al. 2008; Veterinary cooperative oncology group, 2011). Notably, of 26 dogs that received vinblastine at 3.50 mg/m2 in a subsequent study, 46% developed grade 4 neutropenia and two dogs presented with febrile neutropenia despite the use of prophylactic antibiotics (Rassnick et al. 2008). The intended dose intensity of that protocol was 1.94 mg/m2/week; however, dose intensity in the first 4 weeks (1.75 mg/m2/week) was lower than that in the first 4 weeks of the traditional vinblastine protocol using a dosage of 2.00 mg/m2 (2 mg/m2/week) (Rassnick et al. 2008).
In a separate strategy to increase the dose intensity in canine MCTs, a dose-escalating vinblastine-prednisolone protocol provided a starting dosage of 2.00 mg/m2 that escalated in weekly increments to 2.33 mg/m2, 2.67 mg/m2 and 3.00 mg/m2 followed by four doses at 3.00 mg/m2 every other week, with an intended dose intensity of 1.83 mg/m2/week (Vickery et al. 2008). Of 24 dogs treated, only three dogs (12.5%) required dose reductions during the protocol, and fewer than 10% of vinblastine administrations at 2.67 mg/m2 or 3.00 mg/m2 were associated with grade 3 or 4 toxicity (Vickery et al. 2008).
The current prospective study was undertaken in an attempt to further optimise dose intensity with a rapidly escalating vinblastine protocol (VPP), shown in Table 1, in which vinblastine was escalated from 2.30 mg/m2 weekly such that 3.00 mg/m2 was given 7 days apart once, at day 14 and day 21, prior to continuing a standard every other week administration with a dosage of 3.00 mg/m2 for the latter half of the protocol. VPP was designed as an interim step to assess the tolerability of vinblastine given weekly at one point in the protocol prior to instituting weekly vinblastine at 3.00 mg/m2. The primary hypothesis was that VPP would be well tolerated in dogs with MCTs with fewer than 20% DLTs as defined by grade 3 gastrointestinal toxicities or grade 4 neutropenias. While arbitrarily chosen, 20% was considered acceptable for continued optimisation of the protocol, and therefore was selected as a defined endpoint. The occurrence of greater than 20% DLTs was deemed unacceptable and would require alteration of the protocol to reduce toxicities. The primary objective of the study was to determine the toxicity profile of VPP.
| Day | Vinblastine (mg/m2) | Prednisolone (mg/kg SID) |
|---|---|---|
| 0 | 2.3 | 1 |
| 7 | 2.6 | 1 |
| 14 | 3 | 0.5 |
| 21 | 3 | 0.5 |
| 35 | 3 | 0.5 |
| 49 | 3 | 0.5 |
| 63 | 3 | 0.5 |
| 77 | 3 | 0.5 |
Materials and methods
Dogs
Chemotherapy-naïve client-owned dogs that were referred to the Oncology Department of the Hospital for Small Animals of the Royal (Dick) School of Veterinary Studies with cytologically or histopathologically confirmed MCTs from February 2013 to July 2015, and with clinical indication for receiving chemotherapy, were eligible to receive VPP. The clinical protocol and data collection were approved by the institutional Veterinary Ethics and Review Committee. Chemotherapy was used as an adjuvant treatment to local therapy in dogs with high-risk MCTs or as a sole or adjuvant therapy for dogs in which adequate local treatment was not feasible or declined. A ‘high-risk’ MCT was defined as a MCT with at least one of the following negative prognostic factors: high grade (Patnaik or Kiupel), present in a high-risk location (mucosal, preputial or scrotal), recurrence and/or documented locoregional or distant metastases. Dogs with distant metastasis were eligible to be included. Dogs with ‘high risk’ subcutaneous MCTs could also be included. Although there is not a reliable grading scheme for subcutaneous or mucosal MCTs, Kiupel grading criteria was applied by a pathologist in these tumours in order to provide some measure of histologic features of malignancy (Kiupel et al. 2011). Dogs with completely excised MCTs were defined as those in which ≥3 mm radially and at least one fascial plane deep tumour-free margins were obtained. Incomplete excision was defined as <1 mm of margin histologically. All others were considered narrowly excised (1–3 mm of margin). For dogs with narrowly excised or incompletely excised high-risk MCTs, revision surgery and/or definitive-intent RT with photons or electrons was recommended. All radiation treatments were prescribed by a radiation oncologist board-certified by the American College of Veterinary Radiology (ACVR) and administered by a licensed radiation therapist. Radiation-induced acute toxicity was monitored with routine weekly rechecks until resolution, and graded according to the Veterinary Radiation Therapy Oncology Group acute radiation morbidity scoring scheme (Ladue & Klein 2001). In dogs with microscopic disease, chemotherapy with or without concurrent RT was initiated following recovery from surgery.
All dogs underwent clinical staging prior to starting chemotherapy, consisting of a full physical examination, complete blood count (CBC), serum biochemistry profile, fine needle aspirate of regional lymph nodes if accessible, three-view thoracic radiographs and abdominal ultrasound. In dogs with high-risk MCTs, routine fine needle aspirate of liver and spleen were performed regardless of their ultrasonographic appearance when possible. Ki67 expression was not determined. Exclusion criteria included dogs with a suggestion of significant bone marrow dysfunction (assessed with a CBC), inadequate performance status [Modified Eastern Cooperative Oncology Group (ECOG) constitutional performance score > 1], concurrent diseases requiring immunosuppressive therapy (i.e. severe atopy, immune-mediated disease) other than prednisolone and concurrent systemic anti-neoplastic treatment (Oken et al. 1982). Dog and tumour characteristics, including signalment, clinical and histopathologic features, were recorded.
Treatment and toxicity assessment
VPP is described in Table 1. Dogs with macroscopic disease were concurrently treated with gastro-protectant therapy (a proton pump inhibitor) as well as a systemic histamine blocker.
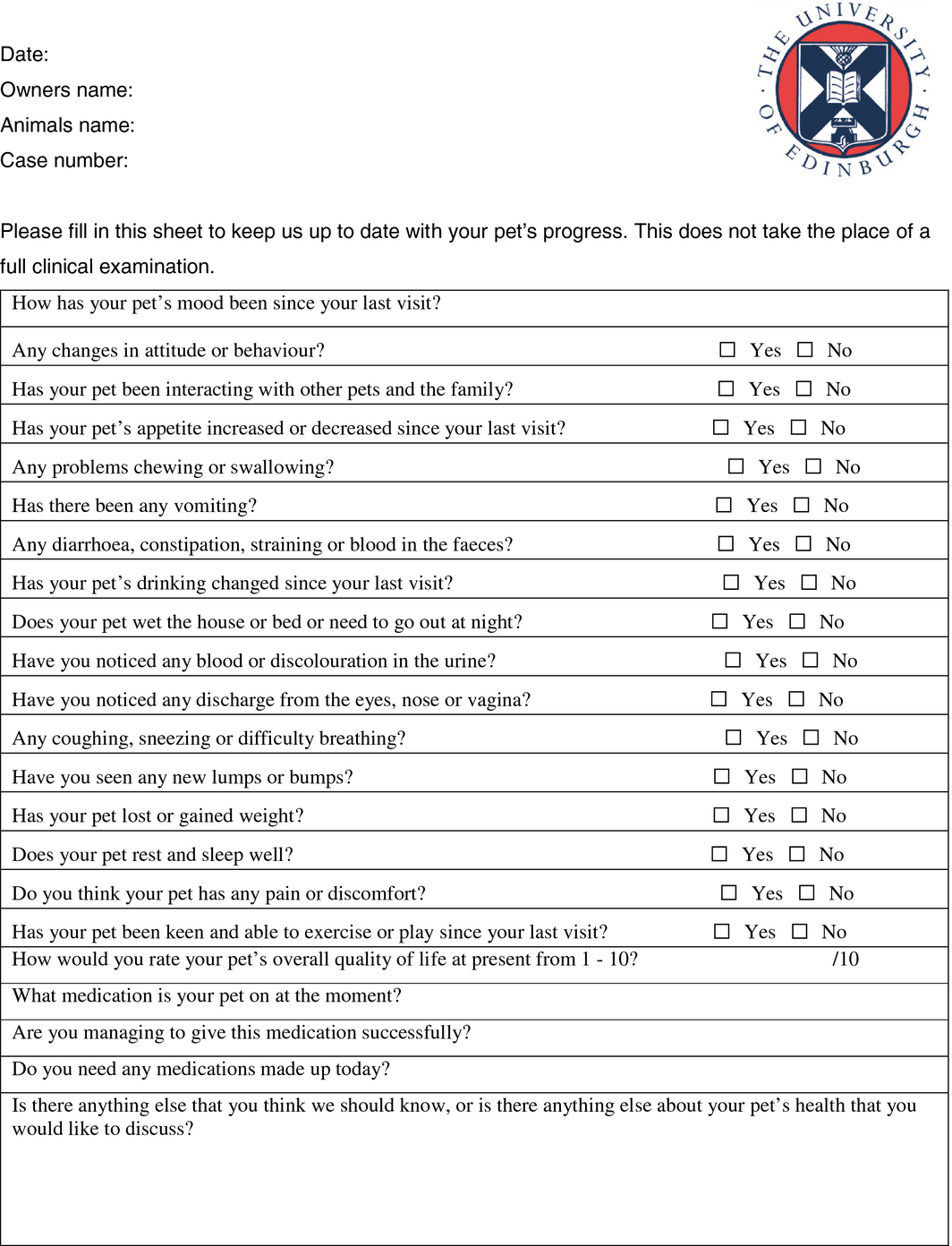
A complete physical examination was performed and both CBC and standardised quality-of-life questionnaire (Fig. 1) were assessed prior to each dosage of chemotherapy. The decision to perform a CBC at weeks 5, 7, 9, 11 and 13 (1-week post vinblastine) was clinician-dependent and varied among dogs. All toxicities were graded according to VCOG CTCAE v1.1 and the quality-of-life questionnaire aided in ensuring all side effects reported by the owner were documented and graded (Stanclift & Gilson 2008). The following were considered DLTs: grade 4 neutropenia, ≥ grade 3 thrombocytopenia, ≥ grade 3 gastrointestinal toxicity or any neutropenia that caused a dose delay. Neutrophil and platelet counts were required to be ≥1.5 × 109 neutrophils/l (1500/μL) and ≥ 50 × 109 platelets/l (50 000/μL), respectively, immediately prior to vinblastine administration. Vinblastine dose reductions of 10% were calculated following the occurrence of any DLT. Subsequent to a dose delay associated with neutropenia or thrombocytopenia, a CBC was reassessed 1–3 days after delay. Dose escalation was permitted in the protocol following early dose reduction and was performed in 5% dose increments. Grade 2 gastrointestinal toxicities were managed with supportive care if spontaneous resolution did not occur and/or when clients deemed effects intolerable. Maropitant was used as a first-line medication for vomiting, nausea or decreased appetite, and metronidazole was used as a first-line medication for colitis.
|
|
|
Figure 1. “Quality-of-life” form. |
Statistical analysis
Statistical analyses were performed by a statistician (IH) using the R Statistical System (R Core Team, 2015). Initial univariable analysis was performed on the following variables, which were evaluated as possible predictors of toxicity or tolerability of 3.00 mg/m2 administered 7 days apart at days 14 and 21: age, weight, sex, neuter status, stage, Patnaik grade, Kiupel grade, margin status, mitotic index (MI) and concurrent RT. Dichotomous variables were evaluated via Fishers exact test, while the numerical variables were evaluated via Mann–Whitney test. Variables with a univariable P ≤ 0.2 were entered into a multi-variable binary logistic regression model to assess potential confounding and allow estimation of a corrected strength of association between predictive factor and outcome conditional on other factors. Where data were missing in factors for multi-variable modelling, a subset dataset of complete observations on variables of interest was used. The multi-variable models were simplified to minimise Akaikes Information Criteria (AIC) – a parameter count penalised measure of model fit. A P ≤ 0.05 was considered statistically significant for reporting of final variables from the models. The study involved multiple comparisons and hypothesis tests. No explicit corrections are made for this and P-values from hypothesis tests are presented as is.
Results
Dog and tumour characteristics
Thirty-four dogs were enrolled in the study. Clinical characteristics for all dogs are listed in Table 2. Median age at the time of first dose of vinblastine was 6 years, and median weight was 24.8 kg. Three dogs weighed less than 10 kg.
| Median age (range) | 6 years (1–12 years) |
| Median weight (range) | 24.8 kg (7.2–48.6 kg) |
| Sex | |
| Male neutered | 12 |
| Female neutered | 14 |
| Male intact | 4 |
| Female intact | 4 |
| Breed | |
| Labrador Retriever | 12 |
| Mixed Breed | 4 |
| Springer Spaniel | 3 |
| Boxer | 3 |
| Weimaraner | 2 |
| Stafford Bull Terrier | 2 |
| Jack Russell Terrier | 2 |
| Lhasa Apso | 1 |
| Native American Indian | 1 |
| Pug | 1 |
| Rottweiler | 1 |
| Scottish Terrier | 1 |
| Shar Pei | 1 |
A diagnosis of MCT was achieved histopathologically in 33 dogs and cytologically in one dog. In all cases where histopathology was available, tumours were graded via the Patnaik and/or Kiupel grading system. The median MI for all tumours was 1 (range: 0–39). Multiple pathologists in several laboratories evaluated biopsy specimens. Histopathological margins were evaluated in all cases where surgery was performed (30 dogs; Table 3). Complete margins were achieved in 17 dogs (56.6%), incomplete margins were achieved in 11 dogs (36.6%) and narrow margins were achieved in two dogs (6.6%).
| MCT Characteristics | Number |
|---|---|
| Macroscopic MCT | 4 |
| Diffuse, grade 3 high grade, recurrent, regional metastases, MI > 5 | 1 |
| Diffuse, grade 1–2 low grade | 1 |
| Unknown grade – cutaneous, visceral metastases | 1 |
| Unknown grade – nasal mucosa | 1 |
| Microscopic MCT | 30 |
| Subcutaneous high grade MCT | 2 |
| Regional metastases | 1 |
| Recurrent | 1 |
| Incomplete excision | 2 |
| Subcutaneous low grade MCT | 3 |
| Regional metastasis | 2 |
| Complete excision | 1 |
| Incomplete excision | 2 |
| Cutaneous grade 3 MCT | 7 |
| MI >5 | 5 |
| Regional metastases | 2 |
| Recurrent | 1 |
| Complete excision | 4 |
| Incomplete excision | 3 |
| Cutaneous grade 2 high grade MCT | 3 |
| Regional metastases | 3 |
| Visceral metastases | 1 |
| Recurrent | 1 |
| Complete excision | 1 |
| Narrow excision | 1 |
| Incomplete excision | 1 |
| Cutaneous grade 2 low grade MCT | 11 |
| Regional metastases | 9 |
| Recurrent | 2 |
| Complete excision | 9 |
| Narrow excision | 1 |
| Incomplete excision | 1 |
| High-risk location | 4 |
| Nasal mucosa high grade | 1 |
| Oral mucosa low grade | 2 |
| Scrotal grade 2 low grade with regional metastases | 1 |
| Complete excision | 2 |
| Incomplete excision | 2 |
Tumour characteristics at the time of chemotherapy initiation are provided in Table 3. Twenty-nine dogs had high-risk MCTs and received VPP as a first-line adjuvant treatment for microscopic disease. Eight dogs received concurrent definitive-intent RT. One dog received VPP for potential improved local control of an incompletely excised Kiupel low-grade subcutaneous MCT after declining RT. Three dogs received VPP as treatment for multifocal macroscopic disease, and one dog with a high-risk MCT received four doses of cytoreductive chemotherapy followed by definitive intent RT concurrently with the remaining doses of vinblastine.
Out of the dogs with high-risk MCTs, several dogs had multiple factors associated with aggressive disease: three dogs with grade 3 MCTs, one dog with a scrotal MCT, one dog with splenic and hepatic metastases and one dog with diffuse macroscopic cutaneous MCT (two of which were recurrent) had concurrent regional lymph node metastasis. All dogs with lymph node metastasis had at least one metastatic lymph node confirmed histopathologically.
Treatment
Of the nine dogs that received RT, three were treated with conformal RT utilising computerised treatment plans (Eclipse, Varian Medical Systems, Palo Alto, CA) while the remainder were manually treated with 6–12 MeV electrons (n=3) or 6 MV photons (n=3). Five dogs with confirmed metastatic lymph nodes that had been surgically removed had regional lymph node beds irradiated in conjunction with the primary MCT site. Radiation was prescribed to the planning target volume (PTV) in all cases; the radiation prescription consisted of 48 Gy in seven dogs, with six dogs prescribed 16 fractions of 3 Gy and one dog prescribed 15 fractions of 3.2 Gy. Two dogs were prescribed 18 fractions of 2.8 Gy to 48.6 Gy due to dose-limiting normal tissues adjacent to the surgical sites. For conformal treatments, the clinical target volume (CTV) was defined by post-surgical changes evident on CT with a 5 mm margin in all directions unless a natural barrier was present. The PTV was expanded from the CTV by 3 mm in all directions. For manual photon and electron plans, the CTV included 2.5 cm of margins to account for non-visible/non-palpable microscopic disease and the PTV included an additional margin of 0.5 cm where possible. Seven of nine dogs developed grade 3 radiation-induced skin toxicity, while two dogs developed grade 2 radiation-induced skin toxicity; all resolved within 3 weeks of completion of RT.
A total of 220 treatments of vinblastine were administered with a median dosage of 3.00 mg/m2 (range: 2.00–3.00 mg/m2); the median number of doses administered to each dog was 8 (range: 1–8). Despite the intended dosages in the protocol, variable doses administered as adverse events caused dose adjustments (Table 4). Twenty-four of the 34 dogs initially enrolled (70%) tolerated 3.00 mg/m2 administered at day 14 and 21.
| Dose | Number administered (220 total) | Number of Grade 1 or 2 toxicities (%*) | Number of Grade 3 toxicities (%*) | Number of Grade 4 toxicities (%*) |
|---|---|---|---|---|
| 2.00 mg/m2 | 2 | 0 (0%) | 0 (0%) | 0 (0%) |
| 2.10 mg/m2 | 4 | 0 (0%) | 0 (0%) | 0 (0%) |
| 2.20 mg/m2 | 2 | 0 (0%) | 0 (0%) | 1 (50%) |
| 2.30 mg/m2 | 43 | 3 (7.0%) | 3 (7.0%)† | 0 (0%) |
| 2.40 mg/m2 | 5 | 1 (20%) | 0 (0%) | 0 (0%) |
| 2.50 mg/m2 | 1 | 0 (0%) | 0 (0%) | 0 (0%) |
| 2.60 mg/m2 | 29 | 4 (13.8%) | 0 (0%) | 3 (10.3%)† |
| 2.70 mg/m2 | 5 | 1 (20%) | 0 (0%) | 0 (0%) |
| 2.80 mg/m2 | 3 | 0 (0%) | 0 (0%) | 0 (0%) |
| 2.90 mg/m2 | 2 | 1 (50%) | 0 (0%) | 0 (0%) |
| 3.00 mg/m2 | 124 | 9 (7.2%) | 1 (0.8%) | 1 (0.8%) |
*Percentages calculated as the number of toxicities per dosage divided by the total number of doses administered at that dosage multiplied by 100. †One dog in each group developed concurrent toxicities of the same grade, and thus were counted as two separate instances. | ||||
Eight dogs (23.5%) required dose reductions, although 11 dogs (32%) would have required dose reductions had treatment not been discontinued in three dogs that developed DLT. Six of the eight dogs that required dose reductions were subsequently escalated by 5% increments in the dosage at each dose. One dog developed an additional DLT at 2.20 mg/m2, while the remaining five dogs tolerated dose escalations well. One dog was escalated to 3.0 mg/m2.
Twenty-three dogs (68%) completed the 12-week protocol. In total, 24 dogs tolerated 3.00 mg/m2 administered at days 14 and 21 with 17 dogs completing the protocol at the planned dosages and schedule. The remaining seven dogs required protocol alterations in the latter half of the protocol: two dogs developed DLT, one dog was dose-reduced at the clients request following grade 2 gastrointestinal toxicity, three3 dogs developed progressive disease and discontinued VPP and one dog terminated treatment early at the clients request following possible vinblastine extravasation, although extravasation was not confirmed and an extravasation reaction did not develop. Ten dogs did not receive 3.00 mg/m2 on day 14 and 21 for variable reasons: eight dogs developed DLT earlier in the protocol, while two dogs had progressive disease after the first dose of vinblastine and were therefore not escalated.
Toxicity
Neutropenia was the primary DLT and occurred across multiple dosages (Table 4). A total of 11 episodes of dose-limiting neutropenia occurred: one episode following a dosage less than 2.30 mg/m2, seven episodes following dosages between 2.30 and 3.00 mg/m2 and two episodes following administration of 3.00 mg/m2. Five of these episodes caused dose delay, therefore negatively impacted the intended dose intensity. In four dogs that discontinued the protocol early, four additional dose delays would have occurred if affected dogs had continued VPP. None of the other dogs in the study required a dose delay for any other reasons.
Four dogs (12%) developed asymptomatic grade 2 neutropenia at a dosage of 2.30 mg/m2 (N=3) and 2.60 mg/m2 (N=1). As their subsequent scheduled dose of vinblastine was delayed, these four dogs were dose-reduced. Two dogs (5%) developed asymptomatic grade 3 neutropenia at a dose of 2.30 mg/m2: one dog was dose-reduced, while the remaining dog also had concurrent grade 3 thrombocytopenia but stopped VPP due to progressive disease. One dog (2%) developed grade 3 neutropenia at a dosage of 3.00 mg/m2 and required prophylactic antibiotics. Four dogs (12%) developed febrile grade 4 neutropenia. Out of these four dogs, one died following acute respiratory distress and upper airway obstruction approximately 10 days following vinblastine administered at a reduced dosage of 2.20 mg/m2; the neutrophil count had recovered at the time of respiratory distress. This dog had previously required a dose reduction after developing grade 3 neutropenia at a dosage of vinblastine of 2.30 mg/m2 and was being slowly escalated with 5% increase intervals. Post-mortem examination was consistent with pharyngeal oedema and inflammation as well as necrosuppurative pneumonia and disseminated intravascular coagulation (DIC). This dog completed definitive intent RT 12 days prior to developing febrile neutropenia, however, the pharynx and larynx were not in the irradiated field. One dog with febrile grade 4 neutropenia and concurrent grade 4 thrombocytopenia 5 days following vinblastine at 2.60 mg/m2 was euthanized on presentation, as the client declined supportive treatment. The remaining two dogs with febrile neutropenia recovered following 24 h of supportive care: one dog had received a dosage of 2.60 mg/m2, while the other had received 3.00 mg/m2. Three of the four dogs with grade 4 neutropenia underwent concurrent RT upon starting VPP chemotherapy: only one dog developed neutropenia while undergoing RT; the other two dogs had completed RT a minimum of 14 days prior. None of the other dogs receiving RT developed any DLT. Asymptomatic grade 4 neutropenia was not detected in any dog, although a CBC was only consistently performed at the expected nadir in 12 out of 27 dogs that received more than three doses. In the latter half of the protocol, one dog developed grade 3 neutropenia, while a second dog developed grade 4 neutropenia following vinblastine administered at 3.00 mg/m2 even though both dogs had previously tolerated 3.00 mg/m2 at days 14 and 21.
Low-grade myelosuppression and gastrointestinal toxicity were common. Twenty dogs (58%) developed grade 1 neutropenia at a range of dosages (2.30–3.00 mg/m2), and two dogs (5%) developed grade 2 neutropenia that did not disrupt the dose intensity of the protocol as the neutrophil count recovered by the time of the next scheduled dose of vinblastine. Grade 1 thrombocytopenia occurred in seven dogs (20%) at dosages ranging from 2.10 to 3.00 mg/m2 and one dog developed grade 2 thrombocytopenia following vinblastine administered at 2.60 mg/m2. None of these toxicities affected dose intensity. No gastrointestinal DLT was recorded, however, 10 dogs (29%) developed at least one episode of grade 1 or 2 gastrointestinal toxicity during the protocol. Five dogs developed multiple episodes of gastrointestinal toxicity at various vinblastine dosages (2.30–3.00 mg/m2). One dog developed one episode of grade 2 anorexia (2.30 mg/m2), two episodes of grade 2 diarrhoea and anorexia (both at 3.00 mg/m2) and one episode of grade 2 diarrhoea (at 2.9 mg/m2). Despite the lack of conventional gastrointestinal DLT, this dog was dose-reduced because the owner considered these adverse effects unacceptable.
Variables associated with toxicity or tolerability
Univariable analysis (Table 5) for toxicity suggested that dogs receiving concurrent RT (P = 0.048) and intact dogs (P = 0.033) were more likely to develop grade 4 neutropenia, while younger dogs (P = 0.042) were more likely to develop grade 3 neutropenia.
| Grade 3 neutropenia | Grade 4 neutropenia | Increased risk of dose reduction | Decreased tolerability of vinblastine 3.00 mg/m2 weekly administered once | |
|---|---|---|---|---|
| Age | 0.042* | 0.872 | 0.074* | 0.179* |
| Weight | 0.172* | 0.748 | 0.127* | 0.155* |
| Sex | 0.230 | 0.604 | 0.152* | 0.446 |
| Neutered | 0.128* | 0.033* | 1.000 | 0.648 |
|
Patnaik Grade (2 vs. 3)
|
0.249 | 1.000 | 0.362 | 0.41 |
|
Kiupel (High vs. Low)
|
0.561 | 1.000 | 0.459 | 0.699 |
| Margin (incomplete) | 1.000 | 0.126* | 0.696 | 0.244 |
|
MI (>5)
|
0.156* | 1.000 | 0.074* | 0.185* |
| Radiation therapy | 1.000 | 0.048* | 1.000 | 1.000 |
Representative P-values are shown (Fishers exact test). *variables selected for subsequent multi-variable analysis. Values in bold indicate P < 0.05. | ||||
On multi-variable analysis, no variables were associated with toxicity or tolerability of VPP with the exception of MI. Dogs with a MI >5 were more likely to require a dose reduction (P = 0.048 odds ratio 15.9 95% CI 1.44–500.0).
Discussion
The purpose of this study was to evaluate the tolerability of VPP. The demographics and staging of dogs in this study were similar to other studies evaluating canine MCTs (White et al. 2011). Intermediate grade (Patnaik) MCTs were more common in this population of dogs but all of the dogs with intermediate grade MCTs had recurrent or metastatic disease. Although most dogs included in the study had high-risk MCT, the low median MI is not surprising, as this marker lacks sensitivity as a negative prognostic factor (Lelyveld et al. 2015).
As expected, the DLT in this study was neutropenia. While the primary hypothesis was correct in fewer than 20% of dogs that developed grade 4 neutropenia, an unexpected finding was that at least 11% of dogs developed grade 4 febrile neutropenia, which is higher than has been reported in other studies using lower dosages of vinblastine (0–7%) (Davies et al. 2004; Rassnick et al. 2008; Thamm et al. 1999, 2006; Trumel et al. 2005). However, this compares favourably to the 46% of dogs that developed grade 4 neutropenia treated with vinblastine at 3.50 mg/m2 every other week, a protocol that carries similar dose intensity to VPP (Rassnick et al. 2008). Also surprising was the fact that two dogs (6%) died following grade 4 febrile neutropenia, although one of them was euthanized without attempting supportive care.
Interestingly, the only two dogs that developed dose-limiting neutropenia (grade 3 and febrile grade 4 neutropenia) after receiving 3.00 mg/m2 vinblastine had previously tolerated the same dosage given weekly. Vinblastine has not been previously reported in humans or dogs to cause cumulative toxicity; indeed, some authors have suggested that tolerance may develop following prior vinblastine drug exposure (Rowinsky 2011; Vickery et al. 2008). This study suggests that tolerance is unlikely with two dogs developing dose-limiting neutropenia in the latter every other week aspect of the protocol despite previously tolerating the same vinblastine dosage at a 7-day interval. This finding highlights the importance of performing a CBC (or minimally a neutrophil count) approximately 6–7 days following every dose of vinblastine, even if the dosage was previously well tolerated.
No episodes of gastrointestinal DLT were reported, however, 29% of dogs developed grade 1 or grade 2 gastrointestinal toxicity during the protocol. This rate of gastrointestinal adverse effects is slightly higher than the rates previously reported (8–21%) in other studies using the dosage of 2.00 mg/m2 (Rassnick et al. 2008; Thamm et al. 1999, 2006; Trumel et al. 2005). The use of the quality-of-life questionnaire at every visit ensured that owners reflected and reported on any clinical signs. The rate reported here was unlikely to have been under-reported as any adverse gastrointestinal event, whether witnessed by the clinician or reported by the client, was attributed to chemotherapy. It is possible that other reports may have underestimated the rate of low-grade toxicity if clients were not specifically queried. Alternatively, it is possible that this study overestimated gastrointestinal toxicity as not all episodes of diarrhoea, inappetence or vomiting may have been related to chemotherapy.
On univariable analysis, dogs that received RT were at increased risk of grade 4 neutropenia, although this lost significance in multi-variable analysis. While three dogs (33%) developed grade 4 neutropenia, only one occurred during the radiation protocol, while two developed 14 days or longer after completion of RT, following escalated vinblastine dosage. When considering the location and size of the irradiated fields, the three dogs that developed grade four neutropenia had three of the four smallest treatment volumes and contained no or minimal active marrow sites in adult dogs. The remaining six dogs (67%) that received RT tolerated the chemotherapy protocol without dosage reductions or toxicity. Of the 25 dogs that did not receive RT, 25% required dosage reductions during the protocol even though only one (4%) developed grade 4 neutropenia. Previous studies assessing tolerability of dose-escalating vinblastine protocols also did not find that RT was associated with increased risk of toxicity despite the use of radiation units that may increase dose to bone (Vickery et al. 2008). Larger number of dogs would be needed to determine if this is a type II error on multi-variable analysis. As suggested by recent literature, RT alone may control some dogs with locoregional disease for extended periods of time, thus questioning the utility of systemic therapy (Baginski et al. 2014; Chaffin & Thrall 2002; Hume et al. 2011; Schulman 2015). A randomized trial would be useful to compare adequate local control with and without adjuvant VPP to assess if chemotherapy is beneficial in this setting.
Although dogs with a MI >5 were found to be more likely to require a dose reduction in multi-variable analysis, neither Patnaik nor Kiupel grade were associated with toxicity or tolerability of VPP. It is difficult to hypothesise why dogs with high MI would be more likely to require a dose reduction compared to dogs with low MI, particularly in the adjuvant setting following local control. As no correction was made for multiple comparisons, the correlation of MI >5 and toxicity could be due to a type I error.
To the authors’ knowledge, there are no previous published studies assessing the tolerability of vinblastine given at 3.00 mg/m2 7 days apart. This study only included administration of 3.00 mg/m2 at day 14 and day 21 before switching to administration of 3.00 mg/m2 every other week. Dose escalation tolerability could not be assessed in two dogs due to progressive disease following the first dose of vinblastine. Of the remaining 32 dogs, 24 (75%) tolerated 3.00 mg/m2 at a 7-day interval at one point in the protocol, however, two of those dogs required dose reductions once switching to every other week administration of the same dosage. Due to the fact that 26% of dogs required dose reductions, and almost 10% of dogs discontinued the protocol due to toxicity, it is unlikely that a vinblastine protocol can be started at 3.00 mg/m2 and administered weekly for six doses, as was the authors’ proposal prior to this study. More importantly, of the DLTs that occurred, 81% developed following a dosage lower than 3.00 mg/m2. It is also unlikely based on results of this study and previous reports, that the dosage can be systematically further increased without an associated increase in the rate of grade 4 neutropenia (Bailey et al. 2008; Rassnick et al. 2008).
One of the reasons to explain the difference in tolerability of this protocol among different dogs is the significant inter-individual variation in the pharmacologic behaviour of vinblastine (Beck et al. 1979). Several attempts were made to model the data collected in order to identify any algorithms that could predict the ‘ideal’ characteristics to predict tolerability of weekly vinblastine at 3.00 mg/m2, but it was not possible given the small number of dogs. It is important to emphasise that statistical analysis must be interpreted with caution given the low numbers and lack of information on known prognostic factors for toxicity. This is a limitation of statistical analysis with only a small number of dogs, however, the goal was to identify any patterns that could guide further studies with more robust analysis.
Most chemotherapy dosages for companion animals and humans are prescribed on the basis of the patients body surface area (BSA), which tends to correlate poorly with drug pharmacokinetics (Arrington et al. 1994; Frazier & Price 1998a; Page et al. 1988; Frazier & Price 1998b; Walko & McLeod 2009). BSA is proportional to blood volume and glomerular filtration rate, despite that neither contribute to chemotherapy efficacy nor toxicity as much as liver function or other metabolic variations (Freireich et al. 1966; Gao et al. 2008; Goldsmith et al. 1975; Gurney 1996). However, it provides a method by which the maximum tolerated dose of many chemotherapy drugs in various species including humans, dogs, rats and mice is normalised (Freireich et al. 1966; Gao et al. 2008; Goldsmith et al. 1975; Pinkel 1958). To date, there is no clear relationship between pharmacokinetic parameters and BSA for common chemotherapy drugs; in some BSA-calculated doses administered to people, up to 20-fold variation in pharmacokinetics may routinely occur (Gurney 1996). For drugs like vinblastine that are metabolised, the use of BSA may not be ideal as tumour effects and adverse effects are based on complex processes such as metabolism and genetics, making it challenging to develop a system that works for all dosing (Frazier & Price 1998a; Greek & Rice 2012; Frazier & Price 1998b). Tumour and patient chemosensitivity variations likely depend on pharmacokinetic, pharmacodynamic and pharmacogenomic differences, which are early areas of active research in veterinary medicine. In this particular group of dogs, multi-drug resistance 1 gene (MDR-1) polymorphisms and/or concurrent prednisolone administration may have altered drug disposition (Sathiapalan & El-Soth 2001).
As previous studies have suggested, myelosuppression may be predictive of cancer response to chemotherapy (Sorenmo et al. 2010; Vaughan et al. 2007). Therefore, dogs that do not develop substantial neutropenia may benefit from individual dosage escalations, even above 3.00 mg/m2, in order to achieve a lower neutrophil count. An alternative strategy to further optimise the dose intensity of the protocol would be to increase dose density. Dose-dense chemotherapy regimens aim to potentiate response by decreasing the inter-treatment interval (Chabner 2011; Norton 1997). The decision to administer vinblastine every other week after the fourth treatment was initially empirically extrapolated, and as this drug has not been reported to have cumulative toxicity and typically causes a neutrophil nadir between 5 and 7 days after administration, dogs would be expected to tolerate weekly treatments (Golden & Langston 1988; Rowinsky 2011; William et al. 1975). Theoretically, Nortons model of fractional cell kill supports a benefit from maximising dose intensity, and dose intensity optimisation may reduce hospital visits and shorten the duration of the protocol (Norton 1997). Both dose density and administered dosage are known to affect response of cancer to chemotherapy, and they both determine the dose intensity of a protocol (Citron et al. 2003; Frei & Canellos 1980; Loibl et al. 2011). Dose reductions and dose delays have both shown to be associated to a more negative outcome in human patients with cancer (Citron et al. 2003; Loibl et al. 2011). In this study, when toxicity caused dose delay, the authors preferred to dose-reduce affected dogs, in order to standardise an approach and ensure tolerability for the pet and owner. Notably, dose delays within an institution may vary from 2 to 7 or more days depending on the clients ability to return. Dogs in this study were dose-reduced in an attempt to standardise administration time points and enable more consistent assessment of dose intensity. Grade 2 neutropenias that required dose delay were also dose-reduced in order to maintain a consistent schedule, although if dogs were switching to administration every 14 days, dose reductions were not necessary. Only 10% dose reductions were performed, as an attempt to limit any negative effect in treatment efficacy. It is important to reiterate that a prospective trial is required to definitively determine if increasing dose intensity or altering dose density improves efficacy and outcome, particularly as quality-of-life measures are vital when considering chemotherapy regimens in pet dogs.
Multiple reports of chemotherapy have suggested that the use of BSA to calculate chemotherapeutic doses results in smaller dogs to be overdosed (Arrington et al. 1994; Frazier & Price 1998a; Page et al. 1988; Frazier & Price 1998b). Although there were few dogs weighing less than 10 kg in this study, they were not at a higher risk of developing toxicities, which correlates well with results in other work investigating mitotic spindle inhibitors (Bailey et al. 2008). The authors were surprised at the range of vinblastine dosages that caused DLT and disruption of the intended protocol. There are obvious flaws in the use of BSA dosing of chemotherapy in dogs, and drug regimen design in human pharmacology and oncology have considered an integrative system to incorporate pharmacokinetics, pharmacodynamics and pharmacogenomics (Frazier & Price 1998a; Frazier & Price 1998b; Swen et al. 2011; Walko & Ikediobi 2012). While veterinary literature currently lacks sufficient information regarding pharmacogenomics differences across dog breeds, it may be that as veterinary knowledge of both genetic and metabolic differences increases, alternative strategies for chemotherapy dosing may be feasible (Lawrence et al. 2015).
Overall, this rapid dose-escalating vinblastine-prednisolone protocol was well tolerated and reported adverse effects were acceptable. Although there is a higher rate of toxicity compared to protocols utilising a lower dosage of vinblastine, this protocol increases dose intensity by 45% compared to the conventional protocol using the static 2.00 mg/m2 dosage protocol, and a 5% increase over the initial dose-escalating protocol (Vickery et al. 2008). Toxicity was similar to that reported in the initial dose escalation protocol in which of 136 doses administered, 3% resulted in grade 3 or 4 adverse event (Vickery et al. 2008). Of 220 doses of vinblastine administered, there were only nine episodes of grade 3 or 4 toxicity (4%) in this study. Although this was a tolerability study and dogs with both microscopic and macroscopic disease were included, the majority of dogs in this study had microscopic disease that was adequately locally controlled (N = 29), whereas in previous studies, many dogs had measurable disease (Rassnick et al. 2008; Thamm et al. 1999). Retrospective comparison between different protocols is problematic due to different sample sizes, patient demographics and response criteria among studies. A prospective randomised trial evaluating a uniform population of dogs with MCTs with similar histopathologic and clinical features should be done to compare protocols.
This study had multiple limitations, many of which have been discussed. It was not a randomised controlled study, therefore historical data were used for comparison of toxicity and tolerability of VPP and the conventional protocol using a dosage of 2.00 mg/m2. As the study was not funded, not all dogs were treated as per clinician recommendations. Specifically, one dog was euthanized due to toxicity, and another dog was dose-reduced despite grade 2 gastrointestinal toxicity. During dose escalation, CBCs were only performed 7 days post-vinblastine administration and were not consistently performed during the latter half of the protocol, therefore episodes of silent grade 4 neutropenia may have been missed. The detection of non-haematological toxicity was dependent on owners recollection of events, and therefore, the grading and frequency of toxicity events could have been under- or overestimated depending on the owners perception. Dogs were included based on their initial histopathologic report and review of slides by one pathologist was not performed. As grade was assessed statistically, this may have influenced the statistical significance. Lastly, although an effort was made to look for factors predictive of toxicity, the small number of dogs included in the study precluded a clinically useful result.
In conclusion, this dose-escalating vinblastine and prednisolone protocol was well-tolerated overall with 4% grade 3 or 4 toxicity following administration of 220 doses of vinblastine. Of the 34 dogs included, 70% tolerated 3.00 mg/m2 given 7 days apart at days 14 and 21 and 68% completed the protocol; 26% of the dogs required dose reductions and 8% discontinued VPP due to toxicity. It is unlikely that vinblastine can be started at 3.00 mg/m2 weekly without incurring unacceptable rates of toxicity. Optimisation of vinblastine dose intensity may be achieved by reducing the inter-treatment interval or by identifying those dogs that can safely be treated with higher dosages. Further investigation to determine if dose intensity is linked to outcome in high-risk canine MCTs is necessary.
Acknowledgements
The authors would like to acknowledge Spela Bavcar, David Argyle, Richard Elders and Pamela Martin for assistance in case accrual.
Source of funding
This study was not funded by any grant or agency.
Conflicts of interest
The authors have no conflicts of interest to disclose.
Contribution
None.
References
- Arnold E.J., Childress M.O., Fourez L.M., Tan K.M., Stewart J.C., Bonney P.L, Knapp D.W. et al. (2011) Clinical trial of vinblastine in dogs with transitional cell carcinoma of the urinary bladder. Journal of Veterinary Internal Medicine25, 1385–1390.
- Arrington K.A., Legendre A.M. & Tabeling G.S., Frazier D.l. (1994) Comparison of body surface area-based and weight-based dosage protocols for doxorubicin administration in dogs. American Journal of Veterinary Research55, 1587–1592.
- Baginski H, Davis G., Bastian R.P. (2014) The prognostic value of lymph node metastasis with Grade 2 MCTs in dogs: 55 Cases (2001–2010). Journal of the American Animal Hospital Association50, 89–95.
- Bailey D.B., Rassnick K.M., Kristal O., Chretin J.D., Balkman C.E. (2008). Phase I dose escalation of single-agent vinblastine in dogs. Journal of Veterinary Internal Medicine22, 1397–1402.
- Beck W.T., Mueller T.J. & Tanzer L.R. (1979) Altered cell surface membrane glycoproteins in Vinca alkaloid-resistant human leukemic lymphoblasts. Cancer Research39(6 Pt 1), 2070–2076.
- Blackwood L., Murphy S., Buracco P., De Vos J.P., De Fornel-Thibaud P., Hirschberger J.et al. (2012) European consensus document on mast cell tumours in dogs and cats. Veterinary and Comparative Oncology10, e1–e29.
- Bostock D.E.. (1986). Neoplasms of the skin and subcutaneous tissues in dogs and cats. British Veterinary Journal142, 1–19.
- Budman D.R., Berry D.A., Cirrincione C.T., Henderson I.C., Wood W.C., Weiss R.B.et al. (1998) Dose and dose intensity as determinants of outcome in the adjuvant treatment of breast cancer. The cancer and leukemia group B. Journal of the National Cancer Institute90, 1205–1211.
- Cahalane A.K., Payne S., Barber L.G., Duda L.E., Henry C.J., Mauldin G.E.et al. (2006b) Prognostic factors for survival of dogs with inguinal and perineal mast cell tumors treated surgically with or without adjunctive treatment: 68 cases (1994–2002). Journal of the American Veterinary Medical Association225, 401–408.
- Chabner B.A. (2011) Clinical Strategies for Cancer Treatment: the role of drugs. In: Cancer chemotherapy and biotherapy principles and practice. 5th edn, 3–14. (eds B.A. Chabner & D.L. Longo), Lippincott Williams and Wilkins: Philadelphia, PA.
- Chaffin K., Thrall D.E. (2002) Results of radiation therapy in 19 dogs with cutaneous mast cell tumor and regional lymph node metastasis. Veterinary Radiology & Ultrasound43, 392–395.
- Citron M.L., Berry D.A., Cirrincione C., Hudis C., Winer E.P., Gradishar W.J.et al. (2003) Randomized trial of dose-dense versus conventionally scheduled and sequential versus concurrent combination chemotherapy as postoperative adjuvant treatment of node-positive primary breast cancer: first report of intergroup trial C9741/Cancer and Leukemia Gorup B Trial 9741. Journal of Clinical Oncology12, 1431.
- Crow S.E. (1977) Treatment of a mast cell tumor in a dog. Modern Veterinary Practice58, 766–767.
- Davies D.R., Wyatt K.M., Jardine J.E., Robertson I.D., Irwin P.J. (2004) Vinblastine and prednisolone as adjunctive therapy for canine cutaneous mast cell tumours. Journal of the American Animal Hospital Association40, 124–130.
- Frazier D.L. & Price G.S. (1998a) Use of body surface area to calculate chemotherapeutic drug dose in dogs: I. Potential problems with current BSA formulae. Journal of Veterinary Internal Medicine/American College of Veterinary Internal Medicine12, 267–271.
- Frazier D.L. & Price G.S. (1998b) Use of body surface area to calculate chemotherapeutic drug dose in dogs: II. limitations imposed by pharmacokinetics factors. Journal of Veterinary Internal Medicine/American College of Veterinary Internal Medicine12, 272–278.
- Frei E. III & Canellos G.P. (1980) Dose: a critical factor in cancer chemotherapy. American Journal of Medicine69, 585–594.
- Freireich E.J., Gehan E.A., Rall D.P., Schmidt L.H., Skipper H.E. (1966) Quantitative comparison of toxicity of anticancer agents in mouse, rat, hamster, dog, monkey, and man. Cancer Chemotherapy Reports Part 150, 219–244.
- Gao B., Klumpen H.J. & Gurney H. (2008) Dose calculation of anticancer drugs. Expert Opinion on Drug Metabolism & Toxicology.4, 1307–1319.
- Golden D.L., Langston V.C. (1988). Uses of vincristine and vinblastine in dogs and cats. Journal of the American Veterinary Medical Association193, 1114–1117.
- Goldsmith M.A., Slavik M. & Carter S.K. (1975) Quantitative prediction of drug toxicity in humans from toxicology in small and large animals. Cancer Research.35, 1354–1364.
- Greek R. & Rice M.J. (2012) Animal models and conserved processes. Theoretical Biology & Medical Modelling9, 40.
- Gurney H. (1996) Dose calculation of anticancer drugs: a review of the current practice and introduction of an alternative. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology14, 2590–2611.
- Hume C.T., Kiupel M., Rigatti L., Shofer F.S., Skorupski K.A., Sorenmo K.U. (2011). Outcomes of dogs with Grade 3 mast cell tumors: 43 Cases (1997–2007). Journal of the American Animal Hospital Association47, 37–44.
- Kiupel M., Webster J.D., Bailey J.L., Best S., DeLay J., Detrisac C.J.et al. (2011) Proposal of a 2-tier histologic grading system for canine cutaneous mast cell tumors to more accurately predict biological behavior. Veterinary Pathology48, 147–155.
- Kwak L.W., Halpern J., Olshen R.A. & Horning S.J. (1990) Prognostic significance of actual dose intensity in diffuse large-cell lymphoma: results of a tree-structured survival analysis. Journal of Clinical Oncology8, 963–977.
- Ladue T. & Klein M.K. (2001) Toxicity criteria of the veterinary radiation therapy oncology group. Veterinary Radiology & Ultrasound42, 475–476.
- Lawrence J., Cameron D., Argyle D. (2015) Species differences in tumour responses to cancer chemotherapy. Philosophical Transactions of the Royal Society of London,Series B370, 1–12.
- Lelyveld S.V., Warland J., Miller R., Maw H., Foale R., Goodfellow M.J.et al. (2015). Comparison between Ki-67 index and mitotic index for predicting outcome in canine mast cell tumours.Small Animal Practice. 56:312–319.
- Loibl S., Skacel T., Nekljudova V., Lück H.J., Schwenkglenks M., Brodowicz T., Zielinskt C., von Minckwitz G. (2011) Evaluating the impact of relative total dose intensity (RTDI) on patients short- and long-term outcome in taxane- and anthracycline-based chemotherapy of metastatic breast cancer: a pooled analysis. BMC Cancer12, 131.
- Lyman G.H. (2009) Impact of chemotherapy dose intensity on cancer patient outcomes. Journal of the National Comprehensive Cancer Network7, 99–108.
- Madewell B.R. & Theilen G.H. (1979) Chemotherapy. In: Veterinary Cancer Medicine, 95–112. (eds G.H. Theilen & B.R. Madewell), Lea and FebigerPhiladelphia, PA.
- Murphy S., Sparkes H.A., Blunden A.S., Brearley M.J. & Smith K.C. (2006) Effects of stage and number of tumours on prognosis of dogs with cutaneous mast cell tumours. The veterinary Record158, 287–291.
- Norton L. (1997). Evolving concepts in the systemic drug therapy of breast cancer. Seminars in Oncology24, S10.
- Oken M.M., Creech R.H., Tormey D.C., Horton J., Davis T.E., McFadden E.T., Carbone P.P. (1982). Toxicity and response criteria of the eastern cooperative oncology group. American Journal of Clinical Oncology5, 649–655.
- Page R.L., Macy D.W., Thrall D.E., Dewhirst M.W., Allen S.L., Heidner G.L.et al. (1988) Unexpected toxicity associated with use of body surface area for dosing melphalan in the dog. Cancer Research48, 288–290.
- Patnaik A.K., Ehler W.J. & MacEwen E.G. (1984) Canine cutaneous mast cell tumor: morphologic grading and survival time in 83 dogs. Veterinary Pathology21, 469–474.
- Pinkel D. (1958) The use of body surface area as a criterion of drug dosage in cancer chemotherapy. Cancer Research18, 853–856.
- R Core Team. (2015). R: A language and environment for statistical computing. R Foundation for Statistical Computing, 2015 Vienna. Available at: https://www.R-project.org/.
- Rassnick K.M., Bailey D.B., Flory A.B., Balkman C.E., Kiselow M.A., Intile J.L., Autio K. (2008). Efficacy of vinblastine for treatment of canine mast cell tumors. Journal of Veterinary Internal Medicine22, 1390–1396.
- Rowinsky K.E. (2011) Antimitotic drugs. In: Cancer chemotherapy and biotherapy principles and practice. 5th edn, 216–266. (eds B.A. Chabner & D.L. Longo), Lippincott Williams and Wilkins: Philadelphia, PA.
- Sathiapalan R.K. & El-Soth H. (2001) Enhanced vincristine neurotoxicity from drug interactions: case report and review of literature. Pediatric Hematology and Oncology18, 543.
- Schulman F.Y. (2015) Letter to the Editor: Is lymph node metastasis of canine grade 2 MCTs justification for adjuvant therapy?Veterinary and Comparative Oncology12, 151.
- Sfiligoi G., Rassnick K.M., Scarlett J.M., Northrup N.C. & Gieger T.L. (2005) Outcome of dogs with mast cell tumors in the inguinal or perineal region versus other cutaneous locations: 124 cases (1990-2001). Journal of the American Veterinary Medical Association226, 1368–1374.
- Singh J., Rana J.S., Sood N., Pangawkar G.R., Gupta P.P. (1996) Clinico-pathological studies on the effect of different anti-neoplastic chemotherapy regimens on transmissible venereal tumours in dogs. Veterinary Research Communications20, 71–1.
- Sorenmo K., Overley B., Krick E., Ferrara T., LaBlanc A. & Shofer F. (2010) Outcome and toxicity associated with a dose-intensified, maintenance-free CHOP-based chemotherapy protocol in canine lymphoma: 130 cases. Veterinary and Comparative Oncology8, 196–208.
- Stanclift R.M. & Gilson S.D. (2008) Evaluation of neoadjuvant prednisone administration and surgical excision in treatment of cutaneous mast cell tumors in dogs. Journal of the American Veterinary Medical Association232, 53–62.
- Swen J.J., Nijenhuis M., de Boer A., Grandia L., Maitland-van der Zee A.H., Mulder H.et al. (2011) Pharmacogenetics: from bench to byte–an update of guidelines. Clinical Pharmacology and Therapeutics89, 662–673.
- Thamm D.H., Mauldin E.A., Vail D.M. (1999) Prednisone and vinblastine chemotherapy for canine mast cell tumor–41 cases (1992-1997). Journal of Veterinary Internal Medicine13, 491–497.
- Thamm D.H., Turek M.M. & Vail D.M. (2006) Outcome and prognostic factors following adjuvant prednisone/vinblastine chemotherapy for high-risk canine mast cell tumour: 61 cases. Journal of Veterinary Medical Science68, 581–587.
- Trumel C., Bourges-Abella N., Touron C., Lanore D., Geffre A., Diquelou A., Guelfi J.F., Braun J.P. (2005) Adverse haematological effects of vinblastine, prednisolone and cimetidine treatment: a retrospective study in 14 dogs with mast cell tumours. Journal of Veterinary Medicine Series A52, 275–279.
- Vaughan A, Johnson J.L., Williams L.E. (2007). Impact of chemotherapeutic dose intensity and hematologic toxicity on first remission duration in dogs with lymphoma treated with a chemoradiotherapy protocol. Journal of Veterinary Internal Medicine21, 1332–1339.
- Veterinary Cooperative Oncology Group (2011) Common terminology criteria for adverse events (VCOG-CTCAE) following chemotherapy or biological antineoplastic therapy in dogs and cats v1.1. Veterinary and Comparative Oncology. DOI: 10.1111/j.1476-5829.2011.00283.x.
- Vickery K.R., Wilson H., Vail D.M. & Thamm D.H. (2008) Dose-escalating vinblastine for the treatment of canine mast cell tumour. Veterinary and Comparative Oncology6, 111–119.
- Walko C.M. & Ikediobi O. (2012) Pharmacogenomic applications in oncology. Journal of Pharmacy Practice25, 439–446.
- Walko C.M. & McLeod H. (2009) Pharmacogenomic progress in individualized dosing of key drugs for cancer patients. Nature clinical practice Oncology6, 153–162.
- White C.R., Hohenhaus A.E., Kelsey J., Procter-Gray E. (2011) Cutaneous MCTs: associations with spay/neuter status, breed, body size, and phylogenetic cluster.Journal of the American Animal Hospital Association47, 210–216.
- William A., Creasey A., Scott A.I., Wei C.C., Kutcher J., Schartz A., Marsh J.C. (1975) Pharmacological studies with vinblastine in the dog. Cancer Research35, 116–120.
- Wudhijarn K., Smith B.J., Button A.M., Habermann T.M., Thompson C.A., Rosenstein L.J.et al. (2015) Relationships between chemotherapy, chemotherapy dose intensity and outcomes of follicular lymphoma in the immunochemotherapy era: a report from the University of Iowa/mayo clinic lymphoma specialized program of research excellence molecular epidemiology resource. Leukaemia & Lymphoma9, 1–8.
Document information
Published on 09/06/17
Submitted on 09/06/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?