Highlights
- Pre-pregnancy problem drinking is more common in patients seeking specialty care.
- Problem drinking is significantly reduced during pregnancys first trimester.
- There was no association between pregnancy or patient characteristics and reduced alcohol consumption during pregnancy.
- Smoking status was not associated with alcohol use reduction in pregnant females.
Abstract
Introduction
Studies show alcohol-preferring mice reduce their alcohol intake during pregnancy; this study questions if the same is true for humans. The current investigation compares womens pre-pregnancy and first trimester alcohol consumption, examines if women with problem drinking diminish their alcohol intake during pregnancy, and determines if prenatal alcohol reduction is associated with characteristics of pregnancy, patients or smoking.
Methods
126 participants in weeks 1–12 of pregnancy, recruited from Obstetric and Family Practices, completed a survey during their initial prenatal visit including two gender-specific AUDITs (Alcohol Use Disorders Identification Tests) querying current and pre-pregnancy alcohol use. AUDIT-C (AUDIT items 1–3) scores measuring pre-pregnancy and first trimester alcohol consumption were compared, analyzed and tested using general linear model repeated. A p ≤ 0.05 was accepted as significant.
Results
Most participants were multiparous, Caucasian high school graduates experiencing nausea and vomiting. Pre-pregnancy alcohol use was significantly (p = 0.019, Fishers exact) higher among women seeing obstetricians. Pre-pregnancy AUDIT-C scores (m (mean) = 2.22, sd (standard deviation) = 2.19) were significantly higher (p < 0.001) than first trimester scores (m = 0.143, sd = 0.532). Among 49 with pre-pregnancy AUDIT-C scores ≥ 3, 45/49 (92%) reduced their alcohol use to zero during the first trimester. Age, race, education, marital status, parity, nausea and vomiting, gestational age and smoking were non-factors in score reduction.
Conclusions
Women reported reducing their alcohol consumption during pregnancy, including those screening positive for pre-pregnancy problem drinking. First trimester alcohol reduction cannot be accounted for by smoking, patient or pregnancy characteristics; public health initiatives, psychological factors and hormonal mechanisms may be implicated.
Keywords
Alcohol;Problem drinking;Pregnancy;Smoking;First trimester
1. Introduction
Alcohol aversion in pregnancy has been demonstrated in rats (Means & Goy, 1982), monkeys (Elton & Wilson, 1977), alcohol-preferring mice (Randall, Lochry, Hughes, & Boggan, 1980) and women with severe alcohol use disorders (Little et al., 1976 ; Little and Streissguth, 1978). In a recent analysis of the prevalence of alcohol use among pregnant women in the United States, 8.7% used alcohol in the past 30 days compared to 58.2% of non-pregnant adults (Oh, Gonzalez, Salas-Wright, Vaughn, & DiNitto, 2017). Many have argued that nausea and vomiting resulting from the first trimester pregnancy hormone, beta human choriogonadotropin (beta hcg) may be part of an endogenous embryo-protective mechanism to deter women from ingesting toxic substances like alcohol (Flaxman and Sherman, 2000 ; Cardwell, 2012). In addition to hormonal factors, public policy may play a role in alcohol use reduction during pregnancy.
In 2016, the Center for Disease Control (CDC) released new guidelines encouraging increased health education, alcohol use screening interventions, and contraception for women with reproductive potential who were using alcohol (Centers for Disease Control and Prevention, 2016). Psychological factors such as mother-infant bonding may also be implicated in gestational alcohol use reduction. Studies evaluating maternal-fetal attachment showed maternal health practices like alcohol abstinence were significantly and positively correlated with fetal attachment and improved neonatal outcomes of normal birth weights (Maddahi et al., 2016 ; Lindgren, 2001).
It remains plausible that like alcohol-preferring mice, problem drinkers may experience a new aversion to alcohol during pregnancy. This aversion may be related to pregnancy characteristics such as nausea and vomiting. The objectives of the current study were to compare womens pre-pregnancy and first trimester alcohol consumption, examine if women screening positive for problem drinking diminish their alcohol intake during pregnancys first trimester, and determine if the alcohol reduction is associated with characteristics of the pregnancy, patient or smoking status.
2. Material and methods
2.1. Study design
This study was a cross-sectional comparison of womens alcohol use three months before pregnancy and during the first trimester.
2.2. Participants
Participants were recruited by self-selection at five medical practices, in a rural and a small metropolitan area, (non-rural), in Illinois as follows: 2 family practice clinics (1 rural, 1 non-rural) and three private obstetric practices (non-rural). Recruitment occurred during the period of August to December 2011. Any woman in her first trimester of pregnancy was eligible for participation. Women > 12 weeks pregnant were excluded from the study to limit retrospective bias regarding pre-pregnancy alcohol use. Women of all ages were allowed to participate. A special waiver of informed consent by guardian for participation by minors was obtained from the IRB. As a result, the consent procedure for pregnant women under age 18 did not differ from those aged 18 and older.
2.3. Procedures
Participants received a one-time anonymous survey from nursing staff at their initial prenatal visit and were allowed to complete the survey, while alone in an exam room. Due to the sensitive nature of reporting alcohol use during pregnancy and to encourage full patient disclosure on alcohol use, survey procedures to ensure patient anonymity were conducted: survey responses were anonymous, locked ballot boxes were provided at all of the sites and participants were instructed to deposit the completed surveys inside them. For similar reasons, no follow up assessment was done. To reduce a social desirability bias in participant responses, surveys were completed in the privacy of an exam room and locked in ballot boxes to protect anonymity. Women were asked by questionnaire to complete two identical measurement tools regarding alcohol. One pertained to current first trimester alcohol habits, while the other elicited retrospective history from three months prior to pregnancy. No other materials or behavioral interventions were offered.
2.4. Measurement
The two outcomes of interest were pre-pregnancy and first trimester alcohol consumption, measured using the Alcohol Use Disorders Identification Test (World Health Organization, 2001) questions 1 through 3 (AUDIT-C) (Bradley et al., 2003). The AUDIT-C is an effective tool for screening hazardous drinking and alcohol use disorders (Bradley et al., 2003) and has been validated for use in primary care settings (Bradley et al., 2007), among female Veteran populations (Bradley et al., 2003 ; Chavez et al., 2012) and pregnant females (Burns, Gray, & Smith, 2010). In order to mirror the female specific definition of risk drinking provided by the National Institute on Alcohol Abuse and Alcoholism (2013), and improve the sensitivity of screening for risk drinking in a female population (Dawson, Grant, Stinson, & Zhou, 2005), the female specific version of AUDIT question 3 was included (Bradley et al., 2003 ; Chavez et al., 2012). Question 3 of this study frames frequency of drinking on one occasion as “four or more drinks” rather than the standard AUDITs “six or more drinks” (World Health Organization, 2001).
Each AUDIT-C question is scored from 0 to 4 points, with a summed total score ranging from 0 to 12 points. Problem drinking was assumed positive with an AUDIT-C score ≥ 3, which was the cutoff observed to balance sensitivity and specificity for problem drinking in female Veterans Affairs patients (Bradley et al., 2003 ; Chavez et al., 2012), and pregnant females (Burns et al., 2010). Participants were classified as non-drinkers (AUDIT-C = 0), mild drinkers (AUDIT-C = 1–2), and problem drinkers (AUDIT-C ≥ 3). Problem drinkers included those who engaged in hazardous drinking and were at-risk for an alcohol use disorder, whereas mild drinkers are assumed not to engage in drinking that puts their health at risk (Bradley et al., 2003 ; Bradley et al., 2007).
2.5. Explanatory variables
To understand if alcohol consumption was associated with patient demographics or pregnancy characteristics, the following variables were included in the self-reported survey: age, race, education, marital status, parity, number of weeks pregnant, and nausea and vomiting of pregnancy (identified as none, mild, moderate, or severe). As smoking status may be associated with alcohol consumption, we asked participants to report their smoking status, using an ordinal scale with quantity of cigarettes smoked, three months prior to pregnancy as well as their current first trimester smoking status. Community survey site was recorded by medical office location, and practice provider was recorded by medical practice type.
3. Theory/calculation
Analyses compared patient demographic and pregnancy characteristics across AUDIT-C score groups using chi-square for nominal and one way anova for interval variables such as age and weeks pregnant. The difference between pre-pregnancy and first trimester AUDIT-C scores was analyzed using a repeated general linear model and descriptive demographic. Smoking and pregnancy variables were tested as independent variables to determine if they influenced the AUDIT-C change from pre-pregnancy to first trimester. Secondary analyses examined smoking differences by comparing patient demographic and pregnancy characteristics with first trimester smoking status using chi-square for nominal variables and t-test for interval variables such as age and weeks pregnant. Pre-pregnancy and first trimester AUDIT-C means for first trimester smokers and non-smokers were analyzed for significance using matched t-tests. All data were obtained from self-report surveys and entered into EXCEL with analysis done by SPSS ver 21.0.0.0.
4. Results
4.1. Patient & pregnancy characteristics
Among the 126 women who participated in the study, most were in their late twenties, Caucasian, had an advanced education, lived in a non-rural community and were non-smokers (Table 1). The mean for gestational age was 8.28 (sd (standard deviation) = 1.97), with most women reporting a prior pregnancy and experiencing some amount of nausea and vomiting during the current pregnancys first trimester.
| PreAUDIT-C 0 (n = 36; 28.6%) | PreAUDIT-C 1–2 (n = 41; 32.5%) | PreAUDIT-C ≥ 3 (na = 49; 38.9%) | Total population (n = 126) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Demographic characteristic | n (m) | %(sd) | n (m) | %(sd) | n (m) | %(sd) | p | n (m) | %(sd) |
| Patient | |||||||||
| Age | 27.31 | 5.35 | 28.37 | 4.93 | 27.18 | 5.34 | 0.532 | 27.63 | 5.18 |
| Race | 0.569 | ||||||||
| Black | 7 | 19.4 | 8 | 19.5 | 6 | 12.2 | 21 | 16.7 | |
| Caucasian/Elseb | 29 | 80.6 | 33 | 80.5 | 43 | 87.8 | 105 | 83.3 | |
| Education | 0.719 | ||||||||
| High school/< | 10 | 27.8 | 7 | 17.1 | 8 | 16.7 | 25 | 20.0 | |
| Some college | 10 | 27.8 | 13 | 31.7 | 17 | 35.4 | 40 | 32.0 | |
| A.D. & above | 16 | 44.4 | 21 | 51.2 | 23 | 47.9 | 60 | 48.0 | |
| Marital status | 0.258 | ||||||||
| Married | 21 | 58.3 | 25 | 61.0 | 22 | 44.9 | 68 | 54.0 | |
| Non-marriedc | 15 | 41.7 | 16 | 39.0 | 27 | 55.1 | 58 | 46.0 | |
| Community | 0.093 | ||||||||
| Rural | 5 | 13.9 | 1 | 2.40 | 8 | 16.3 | 14 | 11.1 | |
| Non-rural | 31 | 86.1 | 40 | 97.6 | 41 | 83.7 | 112 | 88.9 | |
| Provider | 0.019d | ||||||||
| Obstetrician | 23 | 63.9 | 37 | 90.2 | 38 | 77.6 | 98 | 77.8 | |
| Family practice | 13 | 36.1 | 4 | 9.80 | 11 | 22.4 | 28 | 22.2 | |
| Smoking (pre) | 0.204 | ||||||||
| Smoker | 9 | 25.0 | 6 | 14.6 | 15 | 30.6 | 30 | 23.8 | |
| Non-smoker | 20 | 75.0 | 35 | 85.4 | 34 | 69.4 | 96 | 76.2 | |
| Pregnancy | |||||||||
| Weeks pregnant | 8.63 | 1.91 | 8.23 | 2.05 | 8.07 | 1.96 | 0.436 | 8.28 | 1.97 |
| Parity | 0.823 | ||||||||
| Prior pregnancy | 27 | 77.1 | 31 | 77.5 | 34 | 72.3 | 92 | 75.4 | |
| First pregnancy | 8 | 22.9 | 9 | 22.5 | 13 | 27.7 | 30 | 24.6 | |
| NVP | 0.154 | ||||||||
| + | 31 | 86.1 | 30 | 73.2 | 43 | 87.8 | 104 | 82.5 | |
| − | 5 | 13.9 | 11 | 26.8 | 6 | 12.2 | 22 | 17.5 | |
a. Only 1 respondent received all points from question 1.
b. There were 12 non-Caucasians; 6 had AUDIT-C = 0, 4 had AUDIT-C = 1–2, 2 had AUDIT-C ≥ 3.
c. Includes separated, divorced & widowed.
d. Fishers exact. A.D. = associates degree. NVP = nausea & vomiting of pregnancy.
4.2. Pre-pregnancy alcohol use
The sample included 29% (36) non-drinkers (AUDIT-C = 0), 33% (41) mild drinkers (AUDIT-C = 1–2), and 39% (49) problem drinkers (AUDIT-C ≥ 3). These results are consistent with the CDCs recent estimate of alcohol use prevalence in 65.9–74.3% of sexually active, non-pregnant woman (Green, McKnight-Eily, Tan, Mejia, & Denny, 2016). Patient and pregnancy characteristics did not differ significantly across AUDIT-C groups (p > 0.05), with the exception of patient care provider. Pre-pregnancy alcohol use was significantly higher in those participants assessed at private obstetrician practices (p = 0.019, Fishers exact).
4.3. First trimester alcohol use
Of pre-pregnancy drinkers, 91% (82/90) reduced their first trimester AUDIT-C to zero. The mean of first trimester AUDIT-C scores (m (mean) = 0.143, sd = 0.532) was significantly (p < 0.001) reduced from its pre-pregnancy (m = 2.22, sd = 2.19) value. First trimester alcohol use was not significantly associated with any patient or pregnancy characteristics. In addition, care provider was no longer significantly associated with alcohol use during the first trimester.
4.4. First trimester problem drinking
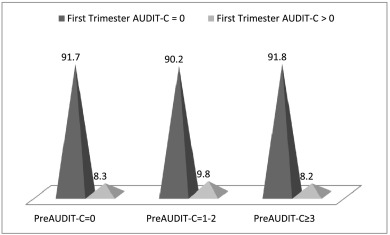
Among 49 respondents with a pre-pregnancy AUDIT-C ≥ 3, only one participant (2%) had a first trimester AUDIT-C ≥ 3. This is compared to 92% (45/49) of pre-pregnancy problem drinkers (AUDIT-C ≥ 3) who reduced their alcohol consumption to zero in the first trimester (Fig. 1).
|
|
|
Fig. 1. Pre-pregnancy AUDIT-C score by first trimester AUDIT-C score. |
4.5. Alcohol use reduction & patient & pregnancy characteristics
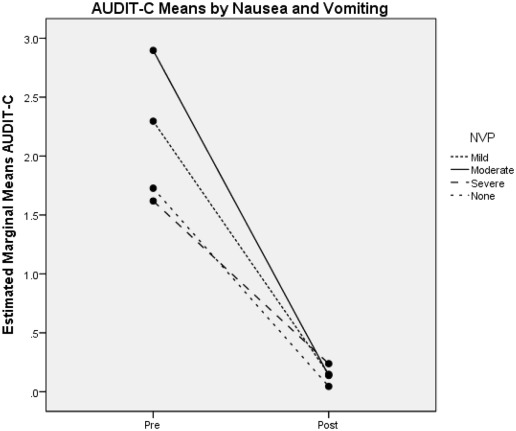
Although alcohol use was diminished during the first trimester of pregnancy, correlates that might account for that change were not significantly associated with alcohol use reduction. None of the patient factors (age, race, education, marital status, community, care provider) or pregnancy factors (parity, number of weeks of pregnancy, nausea and vomiting), were significantly associated with alcohol use reduction. Neither the presence nor intensity of nausea and vomiting was related to alcohol use reduction (Fig. 2).
|
|
|
Fig. 2. Estimated means of AUDIT-C before pregnancy (pre) and during the first trimester (post) by intensity of nausea and vomiting of pregnancy (NVP). |
4.6. Smoking
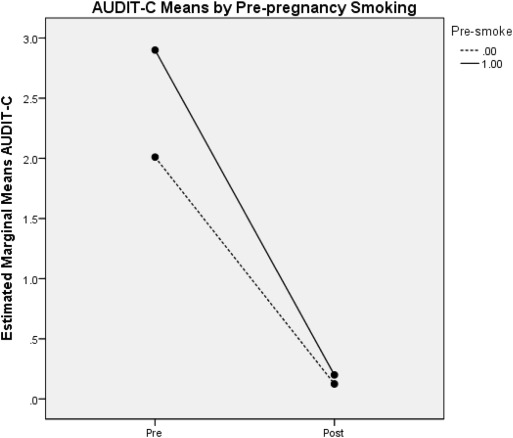
Among participants, 24% (Oh et al., 2017) were smokers prior to pregnancy. There was not any significant difference between pre-pregnancy smokers' AUDIT-C mean (m = 2.90, sd = 2.77) and pre-pregnancy non-smokers' AUDIT-C mean (m = 2.01, sd = 1.95) (Fig. 3). During the first trimester, approximately half (16/30) of pre-pregnancy smokers reported smoking. Among first trimester smokers, 94% (15/16) abstained from alcohol use in the first trimester (AUDIT-C = 0). This is compared to only 38% (6/16) of first trimester smokers reporting zero alcohol use before pregnancy (AUDIT-C = 0); and, 56% (9/16) screening positive for pre-pregnancy problem drinking (AUDIT-C ≥ 3). Among the 16 first trimester smokers, the pre-pregnancy AUDIT-C mean (m = 2.94,sd = 2.72) was significantly different (p = 0.002) from the first trimester AUDIT-C mean (m = 0.250, sd = 1.00). This suggests that the majority of first trimester smokers, including those who screened positive for problem drinking before pregnancy, reduced their alcohol use to zero while continuing to abuse nicotine. There was not any significant association between post-pregnancy smoking and post-pregnancy alcohol use or patient and pregnancy characteristics.
|
|
|
Fig. 3. Estimated means of AUDIT-C before pregnancy (pre) and during the first trimester (post) by pre-pregnancy smoking002E |
5. Discussion
The purpose of this study was to determine if women reduce their alcohol consumption in the first trimester of pregnancy. Our results show that the majority of women who drink prior to pregnancy significantly reduce their alcohol use once they become pregnant. In fact, most women reported not only reducing their alcohol consumption, but abstaining from alcohol use altogether during pregnancys first trimester.
Another noteworthy result of this study was that pre-pregnancy alcohol use was significantly related to having a private practice obstetrician for care. This may reflect a disparity in patient health insurance status as private practice groups are less likely to have uninsured patients. It was noted by Brown et al. in a recent investigation that having health insurance was associated with greater odds of alcohol use among non-pregnant women (Brown et al., 2016).
The second objective of this study was to see if women with hazardous drinking and alcohol use disorders were able to reduce their alcohol use in the first trimester. The results suggest that problem drinkers were able to significantly reduce their alcohol use during pregnancy. Only one respondent (2%) continued problem drinking, compared to 92% of pre-pregnancy problem drinkers (AUDIT-C ≥ 3) who reduced their alcohol consumption to zero in the first trimester. These numbers are nearly identical to the results obtained from the 2011 National Survey on Drug Use and Health (National Survey on Drug Use and Health, 2011).
What could account for alcohol reduction in the first trimester? According to our results, neither patient nor pregnancy characteristics were significant factors. Age, race, education, marital status and community setting did not significantly influence alcohol reduction. And while it is true that the majority of our participants experienced nausea and vomiting, the presence or intensity of NVP (nausea and vomiting of pregnancy) was not significantly associated with reduced alcohol use. This is consistent with Littles findings in 1976, where 41% of those who reported no nausea, 36% of those with slight nausea and 38% of those with moderate or severe nausea changed their alcohol consumption during pregnancy (Little et al., 1976). Perhaps this is because it is not the amount of nausea or emesis that contributes to alcohol use reduction, but possibly pregnancy hormones that are responsible for first trimester aversions.
Beta hCG has been proposed as one potential culprit for new onset taste aversions in pregnant females (Lawson, LeMasters, & Wilson, 2004). Beta hCG is a glycoprotein produced almost exclusively by the placenta that attains maximal levels during the first trimester (Cunningham et al., 2009, chap. 3). Lawson et al. showed an inverse correlation existed between beta hCG levels and coffee consumption, while a positive relation existed between beta hCG levels, nausea and appetite loss (Lawson et al., 2004).
Whatever mechanism exists to reduce alcohol use during pregnancy, it appears that nicotine craving is affected differently. While the majority of smokers reduced their alcohol use to zero, only half (55%) quit smoking during pregnancy. This is consistent with data obtained in 2008 from 28 states as a part of the Pregnancy Risk and Monitoring System (PRAMS), which found that 45% of women who smoked three months before pregnancy quit during pregnancy (Centers for Disease Control and Prevention, 2013). These findings are especially provocative, given national results showing alcohol use to be only approximately 9% during pregnancy (National Survey on Drug Use and Health, 2011) and the current studys finding that over half of first trimester smokers were pre-pregnancy problem drinkers and all but one reduced their alcohol use to zero. A disparity appears to exist between the mechanism for alcohol reduction and nicotine cessation during pregnancy; this mechanism seems to be founded on something other than public messages regarding fetal health. After all, it is inconsistent to choose to adhere to messages regarding fetal alcohol exposure, while disregarding similar messages related to smoking.
No doubt conscious and conscientious embryo-protection may play a role in alcohol reduction during the first trimester of pregnancy. Health concerns for the fetus were frequently cited as a reason for reducing alcohol consumption in Hooks, 1978 study of aversion (Hook, 1978). However, this too must be examined in light of the fact that women with possible alcohol use disorders also reduced their alcohol use to zero during pregnancy. This not only raises questions about the biological processes and advantages of pregnancy, but the true meaning of “addiction,” as there are many mothers who seem unable to “choose” abstinence from alcohol after the fetus leaves the womb. Maternal health concerns also fail to address alcohol abstaining smokers or the previous findings of rat (Means & Goy, 1982), mice (Randall et al., 1980) and macaque (Elton & Wilson, 1977) studies that are replicated by this current investigation.
Limitations to the current study include the possibility that social desirability biased self-reports of alcohol consumption. By taking appropriate procedural measures to ensure patient anonymity, social desirability inaccuracies were minimized. Another limitation is potential inaccuracies in participant reporting due to the retrospective nature of the survey. Retrospective bias was minimized by excluding women who were beyond their first trimester of pregnancy. Since the studys mean number of weeks pregnant was approximately eight, the majority of women only had to reflect two months prior to recall pre-pregnancy alcohol patterns. Despite its limitations, the findings appear to be generalizable as results of the current study were consistent with national (National Survey on Drug Use and Health, 2011 ; Centers for Disease Control and Prevention, 2013) and international findings (Maloney, Hutchinson, Burns, Mattick, & Black, 2011).
Finally, unlike other cross-sectional studies concerned with alcohol use during pregnancy, the retrospective component of this study allows us to track the progress of the individual drinker from pre-pregnancy to the first trimester. This allows us to go beyond the prevalence statements of previous studies. Thus, the current study finds that it is not only the prevalence of problem drinking that is reduced during pregnancy, but problem drinkers who are able to reduce their alcohol use in the first trimester. This may be a subtle, but significant distinction.
6. Conclusions
In conclusion, we found that women reduce their alcohol consumption during the first trimester of pregnancy. This was true for subjects screening positive for problem drinking prior to pregnancy. Factors such as race, education, and smoking could not significantly account for the reduction in alcohol use. While a majority of women reported experiencing nausea and vomiting, the presence or intensity of these symptoms was unrelated to diminished alcohol use. Further research needs to be done to explore the relationship between the endogenous hormonal state of pregnancy and the neurobiological reward system to elucidate how alcohol aversion occurs in previously preferring populations.
Acknowledgements
The following individuals were fundamental to the success of the project:
Tracy A. Bochantin, M.D., Bochantin Obstetrics & Gynecology, Peoria, IL
W. Marc Boyd, M.D., and Dana Humes Goff, APN/CM, MS, Boyd Obstetrics & Gynecology, Peoria, IL
John G. Halvorsen, M.D., Methodist Family Medical Center, Peoria, IL
Thomas G. Lee, D.O., Lee Obstetrics & Gynecology, Peoria, IL
Remi Satkauskas, M.D., Regional Family Health Center, Kewanee, IL
Stephen Lasley, Ph.D., University of Illinois College of Medicine, Peoria, IL
Timothy J. Bruce, Ph.D., University of Illinois College of Medicine, Peoria, IL
Carmen Kirkness, Ph.D., University of Illinois College of Medicine, Peoria, IL
References
- Bradley et al., 2003 K. Bradley, K. Bush, A. Epler, et al.; Two brief alcohol-screening tests from the Alcohol Use Disorders Identification Test (AUDIT) validation in a female veterans affairs patient population; Archives of Internal Medicine, 163 (2003), pp. 821–829
- Bradley et al., 2007 K. Bradley, A. DeBenedetti, R. Volk, E. Williams, D. Frank, D. Kivlahan; AUDIT-C as a brief screen for alcohol misuse in primary care; Alcoholism, Clinical and Experimental Research, 31 (7) (2007), pp. 1208–1217
- Brown et al., 2016 Q.L. Brown, D.S. Hasin, K.M. Keyes, D.S. Fink, O. Ravenell, S.S. Martins; Health insurance, alcohol and tobacco use among pregnant and non-pregnant women of reproductive age; Drug and Alcohol Dependence, 166 (2016), pp. 116–124
- Burns et al., 2010 E. Burns, R. Gray, L. Smith; Brief screening questionnaires to identify problem drinking during pregnancy: A systematic review; Addiction, 105 (2010), pp. 601–614
- Cardwell, 2012 M. Cardwell; Pregnancy sickness: A biopsychological perspective; Obstetrical & Gynecological Survey, 67 (10) (2012), pp. 645–652
- Centers for Disease Control and Prevention, 2013 Centers for Disease Control and Prevention; Tobacco use and pregnancy. [Internet]; http://www.cdc.gov/reproductivehealth/tobaccousepregnancy/ (2013) (Retrieved from: updated April 11 2013, Accessed April 24, 2013)
- Centers for Disease Control and Prevention, 2016 Centers for Disease Control and Prevention; Alcohol and pregnancy. [Internet]; http://www.cdc.gov/vitalsigns/fasd/ (2016) (accessed in 2017)
- Chavez et al., 2012 L. Chavez, E. Williams, G. Lapham, K. Bradley; Association between alcohol screening scores and alcohol-related risks among female veterans affairs patients; Journal of Studies on Alcohol and Drugs, 73 (2012), pp. 391–400
- Cunningham et al., 2009 F.G. Cunningham, K.J. Leveno, S.L. Bloom, J.C. Hauth, D.J. Rouse, C.Y. Spong; Implantation, embryogenesis, and placental development; F.G. Cunningham, K.J. Leveno, S.L. Bloom, J.C. Hauth, D.J. Rouse, C.Y. Spong (Eds.), Williams Obstetrics (2009), p. 23e (Retrieved February 9, 2013 from http://www.accessmedicine.com.proxy.cc.uic.edu/content.aspx?aID=6030341)
- Dawson et al., 2005 D. Dawson, B. Grant, F. Stinson, Y. Zhou; Effectiveness of the derived Alcohol Use Disorders Identification Test (AUDIT-C) in screening for alcohol use disorders and risk drinking in the US general population; Alcoholism, Clinical and Experimental Research, 29 (5) (2005), pp. 844–854
- Elton and Wilson, 1977 R. Elton, M. Wilson; Changes in ethanol consumption by pregnant pigtailed macaques; Journal of Studies on Alcohol, 38 (1977), pp. 2181–2183
- Flaxman and Sherman, 2000 S. Flaxman, P. Sherman; Morning sickness: A mechanism for protecting mother and embryo; The Quarterly Review of Biology, 75 (2) (2000), pp. 113–148
- Green et al., 2016 P.P. Green, L.R. McKnight-Eily, C.H. Tan, R. Mejia, C.H. Denny; Vital signs: Alcohol-exposed pregnancies — United States, 2011–2013; MMWR. Morbidity and Mortality Weekly Report, 65 (2016), pp. 91–97 http://dx.doi.org/10.15585/mmwr.mm6504a6
- Hook, 1978 E. Hook; Dietary cravings and aversions during pregnancy; The American Journal of Clinical Nutrition, 31 (1978), pp. 1355–1362
- Lawson et al., 2004 C. Lawson, G. LeMasters, K. Wilson; Changes in caffeine consumption as a signal of pregnancy; Reproductive Toxicology, 18 (2004), pp. 625–633
- Lindgren, 2001 K. Lindgren; Relationships among maternal-fetal attachment, prenatal depression, and health practices in pregnancy; Research in Nursing & Health, 24 (2001), pp. 203–217
- Little et al., 1976 R. Little, F. Schultz, W. Mandell; Drinking during pregnancy; Journal of Studies on Alcohol, 37 (3) (1976), pp. 375–379
- Little and Streissguth, 1978 R. Little, A. Streissguth; Drinking during pregnancy in alcoholic women; Alcoholism: Clinical and Experimental Research, 2 (2) (1978), pp. 179–183
- Maddahi et al., 2016 M.S. Maddahi, M. Dolatian, M. Khoramabadi, A. Talebi; Correlation of maternal-fetal attachment and health practices during pregnancy with neonatal outcomes; Electronic Physician, 8 (7) (2016), pp. 2639–2644
- Maloney et al., 2011 E. Maloney, D. Hutchinson, L. Burns, R. Mattick, E. Black; Prevalence and predictors of alcohol use in pregnancy and breastfeeding among Australian women; Birth, 38 (2011), pp. 3–9
- Means and Goy, 1982 L. Means, H. Goy; Reduced preference for alcohol during pregnancy and following lactation in rats; Pharmacology Biochemistry and Behavior, 17 (1982), pp. 1097–1101
- National Institute on Alcohol Abuse and Alcoholism, 2013 National Institute on Alcohol Abuse and Alcoholism; Moderate & binge drinking. [Internet]; http://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking (2013) (Retrieved from: Accessed on April 24, 2013)
- National Survey on Drug Use and Health, 2011 National Survey on Drug Use and Health; Summary of national findings [Internet]; http://www.samhsa.gov/data/NSDUH/2011SummNatFindDetTables/Index.aspx (2011) (updated 2012 Dec 11. Retrieved from: Accessed March 13, 2013)
- Oh et al., 2017 S. Oh, J.M.R. Gonzalez, C.P. Salas-Wright, M.G. Vaughn, D.M. DiNitto; Prevalence and correlates of alcohol and tobacco use among pregnant women in the United States: Evidence from the NSDUH 2005–2014; Preventive Medicine, 97 (2017), pp. 93–99
- Randall et al., 1980 C. Randall, E. Lochry, S. Hughes, W. Boggan; Decreased ethanol consumption as a function of pregnancy and lactation in C57BL mice; Pharmacology Biochemistry and Behavior, 13 (1980), pp. 149–153
- World Health Organization, 2001 World Health Organization; AUDIT - the alcohol use disorders identification test: Guidelines for use in primary care (second edition) [Internet]; http://www.who.int/substance_abuse/publications/alcohol/en/ (2001) (Retrieved from: Accessed on March 13, 2013)
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?