Abstract
Introduction
The aim of this study was to evaluate the clinical and radiological outcomes of total hip arthroplasty (THA) in patients with Ankylosing Spondylitis (AS).
Patients and methods
One hundred five hips of 61 AS patients (mean age: 41.3 ± 10.2 years) who underwent THA between 1997 and 2012 were included into the study. Dorrs classification of proximal femoral geometry, acetabular protrusio, bone ankylosis, acetabular protrusion, Brooker classification of heterotopic ossification (HO), Gruen and Charnley classifications of implant loosening were used in radiographic assessments. Patients were called back to return for an additional long-term follow-up for functional assessment.
Results
Cementless total hip arthroplasty was used in 83 hips (79%) and cemented TKA was used in 22 hips (21%). The overall rate of aseptic loosening was 7.6% at a mean follow-up of 5.4 years. Femoral loosening was statistically similar in cemented and cementless femoral components (14% vs. 8%, p = 0.089). Acetabular component loosening was statistically higher in patients with any degree of HO (p = 0.04). Regardless of the type of femoral implant (cemented or cementless), femoral component loosening was higher in Dorrs type C patients (p = 0.005). The average pre-operative HSS was 46.6 ± 16.3, and it improved to 80.7 ± 18.7 at last follow-up (p < 0.01).
Conclusion
Revision incidence was similar in between ankylosed and non-ankylosed hips. While complication rates are high, significant functional improvement can be achieved after THA in patients with AS.
Keywords
Ankylosing spondylitis (AS) ; Total hip arthroplasty (THA) ; Acetabular protrusion ; Bone ankylosis ; Bath Ankylosing Spondylitis Disease Activity Index (BASDAI)
Introduction
Ankylosing spondylitis (AS) is a prototype of seronegative spondyloarthropathies and characterized by progressive erosion of effected joints as a result of inflammation.1 Onset of AS often occurs at a relatively young age and that is accepted as a greater risk of hip involvement.2 The incidence of hip involvement in AS is between 30% and 50% of patients, and 47–90% of patients who have such involvement have it bilaterally.3 ; 4 ; 5 In addition to hip involvement, spine stiffness and intra-thoracic problems can cause severe disability in AS patients.3
Disease modifying anti-rheumatic drugs (DMARDs) such as sulfasalazine and methotrexate have limited in treatment of hip problems.6 ; 7 Standard treatment option for advanced hip disease is THA.4 Indications of THA are refractory pain, disability and radiologic evidence of damage in hips, regardless of age.3 Reported mean implant survival at 8.5 years follow-up was 85.9% and all patients were satisfied with using cementless THA.8 Also cemented THA in AS is provided satisfactory clinical and radiologic outcome, with a 71% survival rate at 27 years follow-up.4
The aim of this study is to evaluate the clinical and radiologic outcomes of cemented and cementless THA in patients with AS at a single institution. We also identified the factors that are associated with poor outcome.
Patients and methods
This is an institutional review board (IRB) approved study. Retrospective review was included all patients diagnosed with hip involvement of AS and treated with THA at a single institution from 1997 to 2012. Patients with minimum 2 year follow up were included. Charts were analyzed for clinical and radiologic features preoperatively and at last follow-up.
The radiographic study involved the review of anteroposterior (AP) both hips x-ray taken pre-operatively, immediate post-operative period and at last follow-up. Preoperative x-ray assessments were included Dorrs classification,9 acetabular protrusio and bone ankylosis. Acetabular protrusion was defined as femoral head in that the medial aspect of the femoral cortex is medial to the ilioischial line.10 Brooker classification11 of heterotopic ossification (HO), Gruen12 and Charnley13 classifications of implant loosening were assessed at last follow-up x-ray.
In addition to the chart and radiographic review, patients were called back to return for additional long-term follow up. Those able to return (32 patients, 59 hips) had additional radiographs, functional outcome assessment with Harris Hip Score (HHS).14 Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) was also assessed to evaluate the activity of disease.15
Statistical analysis was performed using Microsoft Excel (Redmond, WA) and MedCalc B-8400 (Ostend, Belgium). Categorical data were compared using chi-square test, and continuous data using two-sample Students t-test. A p value of ≤0.05 was considered significant. Kaplan–Meier survival analysis with 95% confidence intervals (CI) was used to assess implant survival, with clinical or radiological failure as the endpoint.
Results
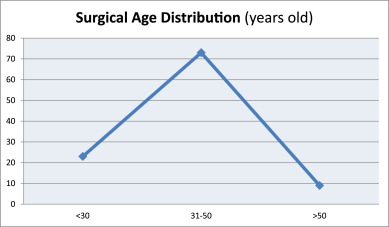
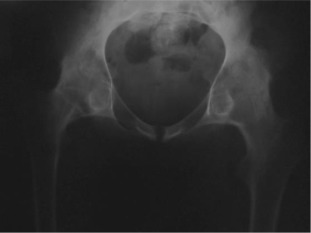
There were 61 patients (50 male, 11 female) with 105 affected hips (72% bilateral, 28% unilateral). The average patient age at surgery was 41.3 ± 10.2 years old. The age of patients at THA was as follows: <30 years for 14 patients (23 hips), 31–50 years for 41 patients (73 hips) and >50 years for 6 patients (9 hips) (Graph 1 ). The younger age at diagnosis (<30 years old) of AS was correlated with younger age at THA (p < 0.05). Bone ankylosis was detected in 37 (35%) and acetabular protrusion was noticed in 18 (17%) hips in pre-operative radiographs (Fig. 1 , Fig. 2 , Fig. 3 ; Fig. 4 ) (Table 1 ). The mean pre-operative flexion contracture was 20.3°±21.8°. In patients without ankylosis, the mean total hip range of motion (ROM) was 67.8°±25.7°.
Graph 1.
Age distribution at surgery (THA).
|
|
|
Fig. 1. Pre-operative x-ray of a patient with bony ankylosis. |
|
|
|
Fig. 2. Four years after bilateral simultaneous THA. |
|
|
|
Fig. 3. Pre-operative x-ray of a patient with protrusio acetabuli. |
|
|
|
Fig. 4. Six years after right side, five years after left side THA. |
| Patients | 61 patients (50 male, 11 female) (72% bilateral, 28% unilateral) | |||
| The average patient age at surgery | 41.3 ± 10.2 | |||
| Cemented (22 hips – 21%) | Non-cemented (83 hips – 79%) | |||
| Acetabular protrusion | 7 | 11 | ||
| Bone ankylosis | 11 | 26 | ||
| Heterotopic ossification (HO) | 5 | 9 | ||
| Aseptic implant loosening | Femoral | Acetabular | Femoral | Acetabular |
| 2 | 2 | 4 | 3 | |
Cementless total hip arthroplasty was used in 83 hips (79%) and cemented TKA was used in 22 hips (21%) though lateral Hardinge approach. Dorrs classification was used as a guide for femoral component selection. In all Dorrs type A patients, cementless femoral component was used, but in the majority of Dorrs type C patients (60%) cemented femoral components were selected. The trend for using cementless type femoral components were increased after 2002 as a result of surgeon preference.
There were early post-operative complications in 9 hips (8.5%). Superficial wound infection in 3 hips, deep infection in 1 hip, peri-prosthetic fracture in 2 hips, sciatic neuropraxy in 1 hip, dislocation in 2 hips. All peri-prosthetic fractures were treated with plate and cable fixation. After close reduction of two acute dislocations, a major instability was noted and treated with revision including realignment of THA components. The sciatic nerve palsies were resolved in two months. Superficial wound infections were treated with antibiotics and daily dressing successfully (Table 3 ).
| Pre-operative | Post-operative | p Value | |
|---|---|---|---|
| Harris Hip Score (HHS) | 46.6 ± 16.3 | 80.7 ± 18.7 | p < 0.01 |
| Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) | 7.3 ± 1.6 | 4.1 ± 1.1 | p < 0.01 |
| Early (within the post-operative first year) | Late (after the first post-operative year) | |||
|---|---|---|---|---|
| Cemented | Cementless | Cemented | Cementless | |
| Superficial wound infection | 1 | 2 | 0 | 0 |
| Deep infection | 0 | 1 | 2 | 3 |
| Girdlestone pseudarthrosis | 0 | 0 | 1 | 1 |
| Peri-prosthetic fracture | 0 | 2 | 0 | 2 |
| Sciatic neuropraxy | 0 | 1 | 0 | 0 |
| Dislocation | 1 | 1 | 0 | 0 |
| Aseptic implant loosening (number of hips) | 0 | 0 | 4 | 4 |
| Heterotopic ossification (HO) | 1 | 1 | 4 | 8 |
Heterotopic ossification (HO) was found in 14 hips (13.3%), with Brooker class 1 in 9 hips, Brooker class 2 in 2 hips, Brooker class 3 in 2 hips and Brooker class 4 in 1 hip (Fig. 5 ). Once the HO was diagnosed by x-ray, 75 mg/day indomethacin was initialed.
|
|
|
Fig. 5. Brooker type 1 heterotopic ossification on the right and type 2 on the left side. |
In the late post-operative period, radiographic loosening of femoral component was present in 6 stems, with subsidence of >5 mm was present in 2 patients according to Gruen classification (Fig. 6 ). For the acetabular component, radiographic loosening was present in 4 patients according to Charnley classification. In 2 patients, radiographic loosening was present both in femoral and acetabular components. Femoral loosening was statistically similar in cemented and cementless femoral components (14% vs. 8%, p = 0.089). Acetabular component loosening was statistically higher in patients with any degree of HO (p = 0.04). Regardless of the type of femoral implant (cemented or cementless), femoral component loosening was higher in Dorrs type C patients (p = 0.005).
|
|
|
Fig. 6. Bone-cement demarcation of left femur was present in the zones on Gruen I-IV-V-VI-VII. Fracture of the cement mantle was seen at the tip of the femoral component on the left side. |
Revision surgery was performed in 17 hips (16.1%). The mean time after the first operation to the first revision was 5.1 ± 1.8 years. Five hip revisions were for late peri-prosthetic infection, and of these, implants were needed to be removed and converted to a Girdlestone pseudarthrosis after several debridement-irrigations, revisions and prolonged antibiotic regimes in two patients. Eight hips were revised because of aseptic implant loosening. Acetabular augments, such as acetabular cup-cage or ring, were used in 4 hips for major column defects and pelvic discontinuity. In these cases, depending on the severity of bone loss, morcellised allograft was used for reconstruction of the medial wall for possible further interventions. Dislocation was not seen in late post-operative period. Two peri-prosthetic fractures were treated with plate and cable fixation. Two patients were underwent removal of HO because of serious limitation of hip motion. These two patients were received a single perioperative dose of 700 cGy radiotherapy on the day of surgery. Two patients had spine osteotomy after the hip procedures. Revision incidence was similar in between patients who had pre-operative bony ankylosis and a mobile hip joint (9% vs. 7%, p = 0.40) (Table 3 ).
The average pre-operative HSS was 46.6 ± 16.3, and it improved to 80.7 ± 18.7 at last follow-up (p < 0.01). The average BASDAI score, which shows the activity of disease, was 7.3 ± 1.6, and it decreased to 4.1 ± 1.1 at last follow-up (p < 0.01) (Table 2 ). Kaplan–Meier survival rate for two years after surgery was 97.7% (95% CI). At a mean follow-up of 5.4 ± 3.3 years, final examination showed 78% of the hips had minimal or no pain, 68.8% patients had good-excellent function.
Discussion
Ankylosing spondylitis is a chronic rheumatologic disease which affects 1% of the population. Hip involvement in AS is between 30% and 50%, and the disease may be bilateral in 47–90% of patients.3 ; 4 Most of the reported studies have either a small group of patient or short follow-up. The study by Joshi et al4 and Bhan et al8 are the largest reported series to date respectively (181 hips with an average of 10.3 years follow up; 92 hips with an average of 8.5 years follow-up). Our study involved 105 hips in 61 patients with an average follow-up of 5.4 years. Our aim was to evaluate the mid-term clinical and radiologic results of THA in patients with AS, and to identify the factors that are associated with poor outcome.
Disabling pain is the most common indication for THA. Patients with bony ankylosis usually do not have pain, but functional limitation and presence of severe deformity can be indications of THA in AS.3 ; 8 In our study, bony ankyloses was present in 35% of all hips pre-operatively. Although these patients were satisfied with the improvement of hip function, some of them were reported hip and groin pain post-operatively.
A high incidence of HO after THA has been reported in patients with AS (9–77%).4 ; 16 ; 17 ; 18 Re-ankylosis rates has been reported high and correlate with ankyloses of the hip before THA.4 ; 18 ; 19 ; 20 ; 21 In our study, HO rate after THA was 13.3% at an average follow-up of 5.4 years after surgery. Some authors suggest routine prophylaxis of non-steroidal anti-inflammatory (NSAI) drugs and single-dose of 700 cGy radiation therapy (RT) one day before or the day of surgery in selected patients, for prevention of HO after THA in high risk patients.16 ; 22 We routinely used indomethacin 75 mg per day post-operatively for one month for HO prevention and pain relief, whereas RT in only revision surgeries.
Surgeons may have some concerns about long-term outcome in young patients who undergo THA, several reports have shown good to excellent functional results with longer survivorship of the implant in AS patients.4 ; 8 ; 23 ; 24 In our study, 16.1% of all hips were undergone a second surgical intervention. The choice of cemented or un-cemented implant is important for long-term outcome and implant survival in this young patient group.8 ; 19 ; 25 ; 26 Recent literature has shown that un-cemented prosthetic designs have the potential of bone ingrowth and may increase the implant survival rates.27 ; 28 ; 29 Cementless THA was used in 79% of the hips in our study. Although, femoral loosening was statistically similar, cementless ones were more prone to loosening at a mean follow up of 5.4 years (p = 0.08).
Cementless prosthesis can still achieve good outcomes without significant proximal femoral morphologic changes, the AS patients were found to have severe osteoporosis in the upper femur, therefore cemented prosthetic designs were recommended for AS patients with severe osteoporosis.26 Class C bone lacks structural integrity, including osteoporotic degradation of the medial and posterior cortices and a wide intramedullary canal, leading to increased risk of loosening of a fixated implant as a result of compromised bone ingrowth between the bone and implant.9 ; 30 Dorr type C femurs are found predominantly in older women with lower body weight. These femurs have structural and cellular compromise and are less favorable for implant fixation.31 Cemented prostheses were predominantly used in Dorrs type C and osteoporotic patients, versus, the usage of cementless were trend to be higher after 2002 in this study. Surgeon preference and patients anatomy were the primary factors for choosing cemented or cementless implants.
Pelvic abnormalities and external rotation deformity may cause implant mal-position during surgery.8 ; 24 ; 32 Due to these abnormalities, surgeons are prone to position the acetabular component more anteverted and vertical. Implant malposition, soft tissue contractures and lateral Hardinge approach may lead to anterior dislocation of the hip.33 All the two dislocations were anterior in our patients.
The overall rate of aseptic loosening were 11.4% at a mean follow-up of 5.4 years in our series, which is slightly higher than the reported literature for AS patients.8 ; 20 ; 21 ; 24 In a systematic review of the literature Zwartele et al was reported the overall failure rate ratio (cementless/cemented) for the cup was 0.6 (95% CI: 0.14–2.60) and for the stem 0.71 (95% CI: 0.06–8.55), both favoring cementless fixation in Rheumatoid Arthritis.34 The studies on the Scandinavian countries register show better results for cementless femoral stems both in young and in older patients with inflammatory arthritis.34 Some authors associate higher loosening rats in AS patients with the stiffness in spine and increased forces around the hip joint.19 Implant malposition as a result of pelvic deformities may also lead to early aseptic loosening in these patients.
In conclusion, patients with Dorrs type C are prone to femoral component loosening and patients who had HO are prone to acetabular loosening in AS. Revision incidence was similar in between ankylosed hips and hips had motion pre-operatively. Survival rates of implants were shorter in AS patients than reported survivals for primary THA in patients with non-inflammatory arthritis in the current literature. Complication rates are high but significant functional improvement can be achieve after THA in patients with AS.
Conflicts of interest
All authors certifies that he or she has no commercial associations that might pose a conflict of interest in connection with the submitted article.
References
- 1 B. Vander Cruyssen, E. Muñoz-Gomariz, P. Font, et al.; Hip involvement in ankylosing spondylitis: epidemiology and risk factors associated with hip replacement surgery; Rheumatology (Oxford), 49 (2010), pp. 73–81
- 2 R. Cooksey, S. Brophy, M.J. Husain, E. Irvine, H. Davies, S. Siebert; The information needs of people living with ankylosing spondylitis: a questionnaire survey; BMC Musculoskelet Disord, 13 (2012), p. 243
- 3 M. Guan, J. Wang, L. Zhao, J. Xiao, Z. Li, Z. Shi; Management of hip involvement in ankylosing spondylitis; Clin Rheumatol, 32 (2013), pp. 1115–1120
- 4 A. Joshi, T. Ilchmann, L. Markovic; Socket wear in bilateral simultaneous total hip arthroplasty; J Arthroplast, 16 (2001), pp. 117–120
- 5 C. Ulucay, T. Ozler, M. Güven, B. Akman, A.O. Kocadal, F. Altıntaş; Etiology of coxarthrosis in patients with total hip replacement; Acta Orthop Traumatol Turc, 47 (2013), pp. 330–333
- 6 J. Braun, I.E. van der Horst-Bruinsma, F. Huang, et al.; Clinical efficacy and safety of etanercept versus sulfasalazine in patients with ankylosing spondylitis: a randomized, double-blind trial; Arthritis Rheum, 63 (2011), pp. 1543–1551
- 7 J. Chen, M.M. Veras, C. Liu, J. Lin; Methotrexate for ankylosing spondylitis; Cochrane Database Syst Rev, 2 (2013), p. CD004524
- 8 S. Bhan, K.K. Eachempati, R. Malhotra; Primary cementless total hip arthroplasty for bony ankylosis in patients with ankylosing spondylitis; J Arthroplast, 23 (2008), pp. 859–866
- 9 L.D. Dorr, M.C. Faugere, A.M. Mackel, T.A. Gruen, B. Bognar, H.H. Malluche; Structural and cellular assessment of bone quality of proximal femur; Bone, 14 (1993), pp. 231–242
- 10 S. Van De Velde, R. Fillman, S. Yandow; The aetiology of protrusio acetabuli. Literature review from 1824 to 2006; Acta Orthop Belg, 72 (2006), pp. 524–529
- 11 A.F. Brooker, J.W. Bowerman, R.A. Robinson, L.H. Riley Jr.; Ectopic ossification following total hip replacement. Incidence and a method of classification; J Bone Jt Surg Am, 55 (1973), pp. 1629–1632
- 12 T.A. Gruen, G.M. McNeice, H.C. Amstutz; “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening; Clin Orthop Relat Res, 141 (1979), pp. 17–27
- 13 J. Charnley; Proceedings: the histology of loosening between acrylic cement and bone; J Bone Jt Surg Br, 57 (1975), p. 245
- 14 W.H. Harris; Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation; J Bone Jt Surg Am, 51 (1969), pp. 737–755
- 15 S. Garrett, T. Jenkinson, L.G. Kennedy, H. Whitelock, P. Gaisford, A. Calin; A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index; J Rheumatol, 21 (1994), pp. 2286–2291
- 16 M.R. Brinker, A.G. Rosenberg, L. Kull, D.D. Cox; Primary noncemented total hip arthroplasty in patients with ankylosing spondylitis. Clinical and radiographic results at an average follow-up period of 6 years; J Arthroplast, 11 (1996), pp. 802–812
- 17 L.G. Walker, C.B. Sledge; Total hip arthroplasty in ankylosing spondylitis; Clin Orthop Relat Res, 262 (1991), pp. 198–204
- 18 A.H. Wilde, H.R. Collins, A.H. Mackenzie; Reankylosis of the hip joint in ankylosing spondylitis after total hip replacement; Arthritis Rheum, 15 (1972), pp. 493–496
- 19 R.S. Bisla, C.S. Ranawat, A.E. Inglis; Total hip replacement in patients with ankylosing spondylitis with involvement of the hip; J Bone Jt Surg Am, 58 (1976), pp. 233–238
- 20 D.J. Kilgus, R.S. Namba, J.E. Gorek, A. Cracchiolo 3rd, H.C. Amstutz; Total hip replacement for patients who have ankylosing spondylitis. The importance of the formation of heterotopic bone and of the durability of fixation of cemented components; J Bone Jt Surg Am, 72 (1990), pp. 834–839
- 21 Y.H. Kim, S.H. Oh, J.S. Kim, S.H. Lee; Total hip arthroplasty for the treatment of osseous ankylosed hips; Clin Orthop Relat Res, 414 (2003), pp. 136–148
- 22 W.L. Healy, T.C. Lo, D.J. Covall, B.A. Pfeifer, S.A. Wasilewski; Single-dose radiation therapy for prevention of heterotopic ossification after total hip arthroplasty; J Arthroplast, 5 (1990), pp. 369–375
- 23 S. Sweeney, R. Gupta, G. Taylor, A. Calin; Total hip arthroplasty in ankylosing spondylitis: outcome in 340 patients; J Rheumatol, 28 (2001), pp. 1862–1866
- 24 W.M. Tang, K.Y. Chiu; Primary total hip arthroplasty in patients with ankylosing spondylitis; J Arthroplast, 15 (2000), pp. 52–58
- 25 D.H. Sochart, M.L. Porter; Long-term results of total hip replacement in young patients who had ankylosing spondylitis. Eighteen to thirty-year results with survivorship analysis; J Bone Jt Surg Am, 79 (1997), pp. 1181–1189
- 26 P. Yang, C.S. Wang, K.Z. Wang, Z.B. Shi, F.L. Gong; Selection of femoral prosthesis in total hip replacement for ankylosing spondylitis; Di Yi Jun Yi Da Xue Xue Bao, 25 (2005), pp. 1468–1473
- 27 J.R. McLaughlin, K.R. Lee; Total hip arthroplasty with an uncemented tapered femoral component in patients younger than 50 years; J Arthroplast, 26 (2011), pp. 9–15
- 28 M. Tannast, T.M. Ecker, S.B. Murphy; Second-generation uncemented stems: excellent 5-13-year results; Arch Orthop Trauma Surg, 129 (2009), pp. 1691–1700
- 29 J.H. Goosen, A.J. Kums, B.J. Kollen, C.C. Verheyen; Porous-coated femoral components with or without hydroxyapatite in primary uncemented total hip arthroplasty: a systematic review of randomized controlled trials; Arch Orthop Trauma Surg, 129 (2009), pp. 1165–1169
- 30 J.B. Meding, M.R. Galley, M.A. Ritter; High survival of uncemented proximally porous-coated titanium alloy femoral stems in osteoporotic bone; Clin Orthop Relat Res, 468 (2010), pp. 441–447
- 31 W. Nash, A. Harris; The Dorr type and cortical thickness index of the proximal femur for predicting peri-operative complications during hemiarthroplasty; J Orthop Surg (Hong Kong), 22 (2014), pp. 92–95
- 32 O. Korkmaz, F.S. Bozkuş, U.S. Aykut, H.C. Caki, M.A. Kaygusuz; The effect of component position on clinical outcomes in resurfacing hip arthroplasty; Acta Orthop Traumatol Turc, 46 (2012), pp. 13–16
- 33 U.G. Leichtle, C.I. Leichtle, F. Taslaci, P. Reize, M. Wünschel; Dislocation after total hip arthroplasty: risk factors and treatment options; Acta Orthop Traumatol Turc, 47 (2013), pp. 96–103
- 34 R.E. Zwartele, S. Witjes, H.C. Doets, T. Stijnen, R.G. Pöll; Cementless total hip arthroplasty in rheumatoid arthritis: a systematic review of the literature; Arch Orthop Trauma Surg, 132 (2012), pp. 535–546
Document information
Published on 31/03/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?