Abstract
Effective and sustainable prevention of work-related musculoskeletal disorders (WR-MSDs) remains a challenge for preventers and policy makers. Coordination of stakeholders involved in the prevention of WR-MSDs is a key factor that requires greater reflection on common knowledge and shared representation of workers' activities among stakeholders. Information on workers' strategies and operational leeway should be the core of common representations, because it places workers at the center of the “work situation system” considered by the intervention models. Participatory ergonomics permitting debates among stakeholders about workers' activity and strategies to cope with the work constraints in practice could help them to share representations of the “work situation system” and cooperate. Sharing representation therefore represents a useful tool for prevention, and preventers should provide sufficient space and time for dialogue and discussion of workers' activities among stakeholders during the conception, implementation, and management of integrated prevention programs.
Keywords
musculoskeletal disorders ; participatory ergonomics ; prevention ; representation ; work
Work-related musculoskeletal disorders (WR-MSDs) of the back (e.g., cervical and low back pain) and upper limbs (e.g., shoulder tendinopathy and carpal tunnel syndrome) are the main causes of work-related disorders and occupational diseases in most countries [1] and [2] . WR-MSDs are responsible for pain, difficulty performing work-related tasks, and long periods of absence from work and disability in the workforce. They engender high social and economic costs [1] and [2] and contribute to high levels of social inequality in health in many countries, as they mainly affect unskilled and poorly skilled workers. Such inequalities are partially avoidable, because a substantial proportion of WR-MSDs could be prevented by workplace interventions [1] and [3] .
Prevention of WR-MSDs remains a challenge despite the scientific knowledge accumulated for 2 decades [4] . These difficulties in preventing WR-MSDs can be explained by the complexity of their determinants, involving not only biomechanical overuse of the soft tissues but also psychosocial interactions and stress at work, and work organization at work situation and company levels. Moreover, the implementation of effective and sustainable programs of WR-MSDs remains a challenge for preventers and policy makers in ever-changing industrial environments, meaning that very few interventions are actually implemented in companies [4] , [5] and [6] .
In this paper, we focus on the need for sharing knowledge on WR-MSDs, workers' activities and prevention strategies among stakeholders (e.g., managers, trades unions, workers, preventers, physicians, insurers) in order to facilitate their cooperation and, finally, ameliorate the effectiveness of preventive interventions.
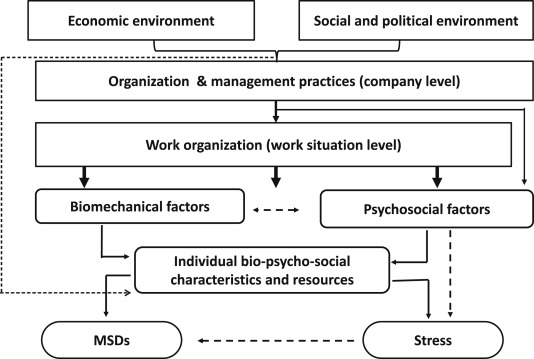
Several risk models for WR-MSDs have been proposed in the literature focusing on the biomechanical [7] , psychosocial [8] , and organizational dimensions of WR-MSDs [9] . In practice, these conceptualizations of WR-MSDs coexist among stakeholders in companies and institutions in charge of the prevention of occupational disorders. The classical biomechanical model is based on the imbalance between soft tissue strains, determined by exposure to high forces, awkward postures and repetitive movements, and the workers functional capacities [7] . Functional capacities are difficult to assess accurately, because the biomechanical constraints vary according to many factors, namely, posture, duration of exposure, and individual characteristics (age, previous MSDs, diabetes, etc.). The biopsychosocial and organizational risk models of WR-MSDs are more pertinent than the classical biomedical model for preventive purposes because they help preventers to take into account the complexity of their determinants. According to these models, the multifactorial nature of WR-MSDs justifies a multidimensional approach based on a global and systemic approach in assessment of the work situation in order to identify the various constraints and their determinants with reference to a multifactorial and multilevel model of WR-MSDs (Fig. 1 ). Indeed, such an integrated multidimensional and multilevel conceptual model of WR-MSDs takes into account not only biomechanical and psychosocial factors at the work situation level, as for the biopsychosocial risk models [1] , but also factors related to work organization at the work situation level. The latter factors determine the biomechanical and psychosocial factors of the work situation, and thus indirectly the working constraints with which the workers have to cope [10] . Factors related to the work organization and management practices have also to be assessed at the company level, as they, in turn, determine the organization at the work situation level and certain psychosocial risk factors. Finally, more general “macro ergonomic” risk factors related to the economic, social, and political environment at market and society levels should be evaluated. Such an integrated multidimensional and multilevel conceptual model suggests enlarging the scope of the assessment of risk factors: (1) biomechanical factors at the job station level; (2) psychosocial and stress factors at the job and work situation levels; (3) organizational factors at work situation and company levels; and (4) socioeconomic factors at the society level. Several ergonomic studies support such an integrated multidimensional conceptual model [9] , [10] and [11] , however, epidemiological findings are still sparse.
|
|
|
Fig. 1. Integrated multidimensional conceptual model of work-related musculoskeletal disorders (MSDs). |
According to the World Health Organization, “Workers' health global plan of action 2008–2017” [12] and systematic reviews [5] , [13] , [14] and [15] , prevention programs must combine simultaneous interventions at three levels of prevention: (1) primary prevention, to limit the incidence of WR-MSDs by risk reduction at the source; (2) secondary prevention, to avoid worsening pain and difficulties at work; and (3) tertiary prevention, to facilitate remaining at work and/or early return to work of workers experiencing chronic pain and disability. The combined three-level intervention is expected to increase overall preventive efficacy because, even when primary interventions on work situations remain ineffective, the severity of disorders can be reduced and their prognosis in terms of work ability improved by interventions at any stage (from acute to chronic) of WR-MSDs. Evidence-based multidimensional interventions combine workers' training sessions, physical and organizational ergonomics, and physical exercise programs [5] , [13] , [14] and [15] . They produce both short- and long-term effects by coordinating actions with different time frames in order to increase the sustainability of the preventive effects. For example, technical improvement of job stations will decrease biomechanical strains and enhance short-term preventive effects, whereas health promotion should modify workers' behavior in the long term. From a conceptual point of view, various risk models for WR-MSDs should be combined when designing such integrated prevention programs: (1) a biomechanical model; (2) a biopsychosocial model; and (3) an ergonomic organizational model. On the one hand, the technical approach of prevention, such as ergonomics of workstations and equipment, aiming to decrease biomechanical exposure, is based on a biomechanical model of WR-MSDs. On the other hand, the psychological approach, such as interventions regarding social relationships and stress factors and return-to-work interventions involving physical and psychological reconditioning, is based on a biopsychosocial model of the disorders and related incapacity. Finally, the systemic approach of prevention, such as participatory ergonomics, with intervention regarding workstations, work organization, management practices, and individual/collective empowerment, is mainly based on an ergonomic organizational model of WR-MSDs and their determinants. Such prevention programs involve a large number of stakeholders both within and outside the company, all with various backgrounds and differences in professional practice. They need, therefore, to be well coordinated [16] and [17] .
The effectiveness of preventive interventions relies not only on their theoretical efficacy, but also on the quality of their implementation. In practice, implementing such complex interventions encounters many obstacles depending on the features of the local context (company, regulation, quality of occupational health and safety services, etc.) [16] , [17] and [18] . Moreover, few multidimensional integrated prevention programs have been implemented or well coordinated [5] . This can be explained by the difficulties in coordinating and integrating such complex interventions, even when companies have the financial and technical means. These interventions require concerted action, and thus involve effective cooperation of all stakeholders involved in occupational risk prevention (workers, social partners, public authorities, occupational health services, etc.), health promotion, treatment, and rehabilitation medicine [5] and [17] . Cooperation requires: (1) consensus on the conceptual model of the intervention and of the implementation strategy; (2) planning of preventive actions; and (3) coordination to avoid the counterproductive effects of uncoordinated interventions [18] and [19] . This underlines the importance of promoting a shared representation among stakeholders to achieve integrated prevention of WR-MSDs.
Promoting more effective cooperation among stakeholders is therefore a key issue in improving the efficacy of WR-MSD prevention. Collective development of common representation of both WR-MSDs and their relationships with workers' activities among stakeholders reinforces cooperation by overcoming the differences in professional practice of most stakeholders and facilitating general agreement on a strategy of prevention [16] , [18] and [20] . Above all, this underpins the consistency of all combined technical, biomedical, psychosocial, and organizational interventions, which is a key factor in concerted action on work situations and integration of the three-level preventive approach [5] , [17] and [18] . Indeed, this is a Sisyphean task because the variety of stakeholders and their professional backgrounds can easily lead to conflict between their representations of the causation of WR-MSDs and ways of prevention. For example, the levels of prevention to be integrated are based on different theoretical models (from engineering to ergonomics), differences in logic of risk assessment (analytical vs. systemic approaches), and intervention models (from technical to participatory intervention). Finally, they are based on different theoretical representations of the causation of WR-MSDs (biomedical model vs. biopsychosocial or organizational models). Such diversity of points of view can lead to conflict regarding the logic of the action used, leading to disorganization of the intervention planning and lack of coordination of action leading to lower effectiveness [18] .
Improving cooperation among stakeholders requires more promotion of a collective development of common understanding and representation of WR-MSDs (causation, risk model, etc.), of workers' activities (“work” representation), and, more generally, of the “Man at work.” In view of the content to be shared, several studies have examined the construction of shared representations of WR-MSDs for physicians and disabled workers [20] , but very few have examined how to share common representations of workers' activities among interventionists. The latter is a major issue, because integrated WR-MSD prevention is founded on several theoretical models of “Man at work” differing according to the level of prevention. Primary prevention is based mainly on the biomedical model of WR-MSDs, attributing a predominant role to biomechanical constraints [1] and [7] . In this model, workers are “isolated” from the social context of the company without possibility of influencing their tasks. Secondary and tertiary preventions are mainly founded on the biopsychosocial model of WR-MSDs, taking into account the psychological and social components of WR-MSDs [1] and [8] . In this model, operators interact with the social context of the company with little possibility of having influence on their tasks. Secondary and tertiary prevention are sometimes based on the systemic organizational model of WR-MSDs, in which workers are integrated in the companys social context and are able to influence their tasks [1] , [9] and [11] . In the latter case, this risk model introduces the concept of “workers' development” based on their ability to perform operating adjustments, depending on task variability and the extent of operational leeway, in order to achieve production targets while avoiding negative effects on health. Operational leeway is a particularly important concept in the systemic organizational model of WR-MSDs, emphasizing the dynamic nature of workplaces and the active roles played by workers. Operational leeway is defined by “space of freedom” available or constructed by workers to develop alternative strategies and ways of working according to their skills, knowledge, and values in order to achieve production targets, while reducing psychological, mental, and physical strains and avoiding negative health effects [9] . Two types of operational leeway can be distinguished: those provided by work organization and those created by the worker alone or with his/her colleagues [9] , [11] and [19] . Various types of operational leeway may therefore be present in the company, i.e., organizational, spatial, temporal, and collective. Their preventive nature depends not only on their real existence (objective, observable), but also on the workers' capacity to use this operational leeway in real work activities. This depends on workers' understanding of the work environment and their ability to perceive variations of the workplace directly and to proceed to regular operating adjustments. Work organization, therefore, plays a major role and can be either a resource or a constraint, depending on whether it allows operational leeway and development of technical skills and professional know-how.
Work analysis, from a participatory ergonomic perspective, shows how workers actively cope with their tasks in the real environment [9] , [11] and [19] . Questionnaires, checklists, and above all observations and interviews are useful to analyze, understand, and share workers' strategies in real working situations. Such information on workers' strategies should be the core of common representations, because it places workers in the center of the “work situation system” considered by the risk and intervention models, and therefore makes it possible to take into consideration all their dimensions. Participatory ergonomics permitting debates among stakeholders about real workers' activities could help them share representations of the “work situation system” and integrate the broad spectrum of knowledge mobilized for each level of prevention. This makes the transfer of knowledge from theory to practice possible, and facilitates the cooperation and capacity of stakeholders to coordinate and integrate the whole prevention program. Sharing representation therefore represents a level of efficacy for preventers and policy makers, and preventers should provide sufficient space and time for dialogue and discussion of workers' activities among stakeholders during the conception, implementation, and management of integrated prevention programs.
The best way to integrate the multilevel prevention of WR-MSDs and to coordinate stakeholders at the level of the workplace remains a challenge for preventers and constitutes an important field of research in occupational health. This requires greater reflection on the theoretical models of WR-MSDs, and work activities and their representations among stakeholders. Helping to share common representations is a key issue to improve the effectiveness of prevention when designing and implementing integrated prevention programs for WR-MSDs and, more generally, occupational diseases.
Conflicts of interests
None to declare.
Acknowledgments
The French National Research Program for Environmental and Occupational Health of Anses (grant related to the project “Partag-Repre-Tr,” 2012/2/007); The French Institute for Public Health Surveillance (Surveillance Program of Musculoskeletal Disorders) (Grant 9/25/2002-5 ).
References
- [1] National Research Council; Musculoskeletal disorders and the workplace: low back and upper extremity musculoskeletal disorders; National Academy Press, Washington (DC) (2001) 492 p
- [2] A. Parent-Thirion, G. Vermeylen, G. Van Houten, M. Lily-Yrjänäinen, I. Billeta, J. Cabreta; Eurofound. Fifth European Working Conditions Survey. Overview report; Eurofound, Dublin(Ireland) (2012) Report No.: EF1182. 160 p
- [3] Y. Roquelaure, C. Ha, N. Fouquet, A. Descatha, A. Leclerc, M. Goldberg, E. Imbernon; Attributable risk of carpal tunnel syndrome in the general population: implications for intervention programs in the workplace; Scand J Work Environ Health, 35 (2009), pp. 342–348
- [4] R. Wells; Why have we not solved the MSD problem?; Work, 34 (2009), pp. 117–121
- [5] C.A. Kennedy, B.C. Amick 3rd, J.T. Dennerlein, S. Brewer, S. Catli, R. Williams, C. Serra, F. Gerr, E. Irvin, Q. Mahood, A. Franzblau, D. Van Eerd, B. Evanoff, D. Rempel; Systematic review of the role of occupational health and safety interventions in the prevention of upper extremity musculoskeletal symptoms, signs, disorders, injuries, claims and lost time; J Occup Rehabil, 20 (2010), pp. 127–162
- [6] R.H. Westgaard, J. Winkel; Occupational musculoskeletal and mental health: significance of rationalization and opportunities to create sustainable production systems. A systematic review; Appl Ergon, 42 (2011), pp. 261–296
- [7] A. Freivalds; Biomechanics of the upper limbs: mechanics, modeling, and musculoskeletal injuries; (2nd ed.)CRC Press, Boca Raton (FL) (2011) 564 p
- [8] G. Waddell, M. Aylward; Models of sickness and disability applied to common health problems; Royal Society of Medicine Press, London (UK) (2010) 58 p
- [9] M. St-Vincent, N. Vezina, M. Bellemare, D. Denis, E. Ledoux, D. Imbeau; Ergonomics intervention; IRSST Éditions, Montréal (Canada) (2014) 632 p
- [10] S.S. Bao, J.M. Kapellusch, A.S. Merryweather, M.S. Thiese, A. Garg, K.T. Hegmann, B.A. Silverstein; Relationships between job organizational factors, biomechanical and psychosocial exposures; Ergonomics, 23 (2015), pp. 1–26
- [11] S. Caroly, F. Coutarel, A. Landry, I. Mary-Cheray; Sustainable MSD prevention: management for continuous improvement between prevention and production. Ergonomic intervention in two assembly line companies; Appl Ergon, 4 (2010), pp. 591–599
- [12] World Health Organization (WHO); Workers' health: global plan of action. 60th world health assembly; WHO, Geneva (Switzerland) (2007), p. 44 Report No.: WHA 60.26
- [13] I. Rivilis, D. Van Eerd, K. Cullen, D.C. Cole, E. Irvin, J. Tyson, Q. Mahood; Effectiveness of participatory ergonomic interventions on health outcomes: a systematic review; Appl Ergon, 39 (2008), pp. 342–358
- [14] M.T. Driessen, K.I. Proper, M.W. van Tulder, J.R. Anema, P.M. Bongers, A.J. van der Beek; The effectiveness of physical and organizational ergonomic interventions on low back pain and neck pain: a systematic review; Occup Environ Med, 67 (2010), pp. 277–285
- [15] V.C. Hoe, D.M. Urquhart, H.L. Kelsal, M.R. Sim; Ergonomic design and training for preventing work-related musculoskeletal disorders of the upper limb and neck in adults; Cochrane Database Syst Rev, 8 (2012), p. CD008570
- [16] M.J. Durand, N. Vézina, P. Loisel, R. Baril, M.C. Richard, B. Diallo; Workplace interventions for workers with musculoskeletal disabilities: a descriptive review of content; J Occup Rehab, 17 (2007), pp. 123–136
- [17] W. Shaw, Q.N. Hong, G. Pransky, P. Loisel; A literature review describing the role of return-to-work coordinators in trial programs and interventions designed to prevent workplace disability; J Occup Rehabil, 18 (2008), pp. 2–15
- [18] D. Berthelette, N. Leduc, H. Bilodeau, M.J. Durand, C. Faye; Evaluation of the implementation fidelity of an ergonomic training program designed to prevent back pain; Appl Ergon, 43 (2012), pp. 239–245
- [19] M.J. Durand, N. Vézina, R. Baril, P. Loisel, M.C. Richard, S. Ngomo; Margin of manoeuvre indicators in the workplace during the rehabilitation process: a qualitative analysis; J Occup Rehab, 19 (2009), pp. 194–202
- [20] M.F. Coutu, R. Baril, M.J. Durand, D. Côté, A. Rouleau; Representations: an important key to understanding workers' coping behaviours during rehabilitation and the return-to-work process; J Occup Rehabil, 17 (2007), pp. 522–544
Document information
Published on 07/10/16
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?