Abstract
Background
Buccinator-based myomucosal flaps can be used as a lining in oral cavity, pharyngeal, esophageal, and nasal reconstructions. Donor site morbidity is an important factor in selecting a flap, therefore, it was decided that donor site morbidity of this type of flap should be evaluated.
Method
In a retrospective study, patients for whom this flap had been used for oral, nasal, or pharyngeal reconstruction in 2008–2012 were recalled. Donor site morbidity including reduction in maximal interincisal opening (MIO), obliteration of the mandibular vestibule, injury to the Stensen duct, and vertical fibrous band in buccal mucosa were evaluated.
Results
Twenty-two buccinator-based myomucosal flaps (20 patients) had been used for oral, nasal, or oropharyngeal reconstruction. The most common flap used was the Facial Artery Musculomucosal (FAMM) flap (50%), and the commonest cause for flap use was the presence of a cleft lip/palate sequel in patients (45%). Four patients had developed complications (minimal reduction in MIO) related to the donor site.
Conclusion
Donor site morbidity associated with buccinator-based myomucosal flaps is low. However, minimal reduction of mouth opening occurred in 20% of the patients.
Keywords
buccinator;donor site;myomucosal flap
1. Introduction
Buccinator-based myomucosal flaps can be used as a lining in oral cavity, pharyngeal, esophageal, and nasal reconstructions.1; 2; 3 ; 4 The mucosal surface is better than skin for reconstruction of mucosal defects in these regions. Buccinator-based myomucosal flaps are thin flaps with the ability to secrete saliva; therefore, they are optimal for reconstruction of medium-sized defects of the oral cavity.5 These flaps are arterialized, based on the facial or maxillary arteries, which makes them very reliable. Donor site morbidity is an important factor to consider when selecting a flap; therefore, a decision was made to evaluate donor site morbidity in this group of flaps.
2. Materials and method
In a retrospective study, patients for whom this flap had been used for oral, nasal, or pharyngeal reconstruction in 2008–2012 were recalled. All the patients had been operated on by the same surgeon. Donor site morbidity including reduction in maximal interincisal opening (MIO), obliteration of the mandibular vestibule, injury to the Stensen duct, and vertical fibrous band in buccal mucosa were evaluated. Limitations in mouth opening were recorded as a decrease in MIO and classified based on the suggestion of Thomas et al6: severe (MIO < 15 mm), moderate (15 mm < MIO < 30 mm), minimal (30 mm < MIO < 35 mm), and no limitation in mouth opening when MIO was >35 mm. In edentulous patients the same measurements were made while removable complete dentures were in the mouth.
2.1. Flap raising techniques
Anterior incision was considered 1 cm behind the oral commissure. In Facial Artery Musculomucosal (FAMM) flaps the boundary of the flap was chosen anterior to the Stensen duct, however, in BUMIF (buccinator-based myomucosal island flap) flaps, superior incision was designed below the opening of the parotid salivary gland. Inferiorly based FAMM and BUMIF flaps followed the course of the facial artery. The paddle long axis was vertical in FAMM flaps, whereas it was horizontal in posteriorly-based buccinator myomucosal flaps. The paddle of inferiorly based BUMIF flaps has near-equal length and width.
3. Results
Table 1 shows demographic data of the patients who received a buccinator-based myomucosal flap for oral, nasal, or oropharyngeal reconstruction. In total, 22 buccinator-based myomucosal flaps (20 patients) were used for oral, nasal, and oropharyngeal reconstruction. Variants of this flap were mostly used for oral cavity reconstruction (90%). The mean age of the patients was 35.7 ±2.25 years, with a male/female ratio of 11; 9. Various forms of these flaps were used including: FAMM flap (superiorly or inferiorly pedicled), posteriorly based flap (Pribaz flap), BUMIF, and finally the anteriorly based flap. The most commonly used flap was the FAMM flap (50%), and the commonest indication for flap use was late sequelae of cleft lip/palate repair (45%).Other usage in our series included treatment of neoplastic lesions or malignant lesions (35%), and traumatic events (20%). Four patients experienced postoperative radiotherapy, and minimum follow up was 1 year. The donor site had been closed by direct closure in 59% of events. Buccal fat pad mobilization had been used to cover the donor site in 36% of cases. In one case, it had proved impossible to herniate the buccal fat pad into the surgical field; as a result, the superiorly based masseter muscle flap had been used to cover the buccal donor site. Choosing between direct closure and buccal fat pad mobilization to manage donor site was done according to Ferrari et al7 recommendations. Donor sites (width ≥ 3 cm) were covered by buccal fat pads.7
| No. | Age (y) | Sex | Type of buccinator-based flap used | Flap size (cm) | Diagnosis/defect | Complication | Donor site closure | Follow up (y) | Radiotherapy |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 12 | M | FAMM (Sup based) | 2.5 × 4 | Edentulous atrophic Premaxilla | — | DC | 3 | — |
| 2 | 22 | F | Posterior BUMIF (Bilateral) | 3.5 × 4 3.5 × 4 | Palatal fistula | Limitation in MIO (32 mm) | BFP | 3 | — |
| 3 | 14 | M | FAMM (Sup based) | 2.5 × 4 | Unilateral wide AC | — | DC | 1 | — |
| 4 | 35 | F | FAMM (Sup based) | 1.5 × 3 | Anterior mandibular vestibule | — | DC | 1 | — |
| 5 | 40 | F | Inf BUMIF | 5 × 5 | Tongue SCC | Limitation in MIO (31 mm) | BFP | 4 | + |
| 6 | 18 | F | FAMM (Sup based) | 2.5 × 4 | Edentulous atrophic Premaxilla | — | DC | 3 | — |
| 7 | 87 | M | Inf BUMIF | 4.5 × 4.5 | Floor of mouth SCC | — | BFP | 2 | + |
| 8 | 13 | F | Pribaz flap | 2 × 4 | Palatal schwannoma | — | DC | 4 | — |
| 9 | 70 | M | FAMM (Inf based) | 2 × 4.5 | Mandibular vestibule (Trauma) | — | DC | 1 | — |
| 10 | 60 | M | Pribaz flap | 2.5 × 5 | Traumatic palatal fistula | — | DC | 2 | — |
| 11 | 18 | M | FAMM (Sup based) | 2 × 5 | Nasal lining (Trauma) | — | DC | 1 | — |
| 12 | 15 | F | FAMM (Sup based) | 2.5 × 4 | Edentulous atrophic Premaxilla | Limitation in MIO (32 mm) | DC | 2 | — |
| 13 | 35 | M | Sup BUMIF | 3 × 4 | Large palatal fistula | — | Masseter flap | 2 | — |
| 14 | 45 | M | Inf BUMIF | 4 × 4 | Oropharynx (Adenoid cystic carcinoma) | — | BFP | 2 | + |
| 15 | 25 | F | FAMM (Sup based) | 2.5 × 4 | Edentulous atrophic Premaxilla | — | DC | 2 | — |
| 16 | 62 | M | Inf BUMIF | 4 × 5 | Contra lateral mandibular vestibule (Ameloblastoma) | — | BFP | 1 | — |
| 17 | 68 | M | Anteriorly based | 1.5 × 5 | Lower lip vermilion (SCC) | — | DC | 2 | — |
| 18 | 18 | F | FAMM (Sup based) | 3.5 × 5 | Large palatal fistula | Limitation in MIO (33 mm) | BFP | 2 | — |
| 19 | 22 | F | FAMM (Sup based) | 3.5 × 4 | Large palatal fistula | — | BFP | 1 | — |
| 20 | 35 | M | FAMM (Sup based) bilateral | 2.5 × 4 | Anterior maxillary melanoma | — | DC | 4 | + |
AC = alveolar cleft; BFP = buccal fat pad; BUMIF = buccinator based myomucosal island flap; DC = direct closure; F = female; FAMM = facial artery myomucosal flap; Inf = inferior; M = male; MIO = maximal interincisal opening; SCC = squamous cell carcinoma; Sup = superior.
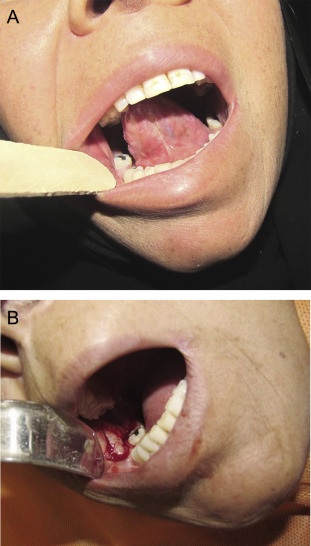
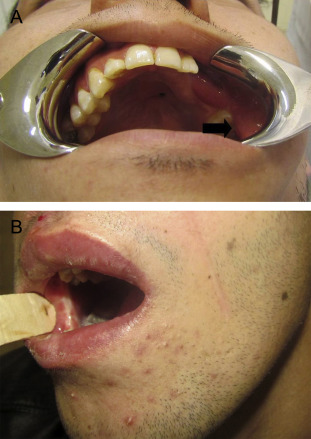
Four patients developed complications (minimal reduction in MIO) related to the donor site. In one patient, a vertical mucosal band in the line of primary closure of the superiorly based FAMM flap occurred, and was overcome by a multiple z plasty. It was the same case in which the donor site had been managed by direct approximation (Figure 1). In another patient, the obliteration of the mandibular buccal vestibule and tight tissue in the donor site (buccal) caused complications; vestibuloplasty with the aid of alloderm was used to solve this problem (Figure 2). Two other patients, who had buccal mucosal scarring, did not agree to further surgical intervention (Figure 3).
|
|
|
Figure 1. (A) Vertical scar band in buccal mucosa. (B) Multiple z-plasty flaps. (C) Result 3 months after operation. |
|
|
|
Figure 2. (A) Obliteration of the mandibular vestibule. (B) Alloderm is used for covering the raw surface of the deepened buccal vestibule. |
|
|
|
Figure 3. Scar in buccal mucosa related to the superiorly-based FAMM flap. (A) Left side. (B) Right side. FAMM, facial artery musculomucosal. |
4. Discussion
Buccinator-based myomucosal flaps are axial-pattern flaps. Structurally, these flaps contain buccal mucosa, part of the buccinator muscle in full thickness, and an axial vessel. If the nourishing vessel is the buccal branch of the maxillary artery, the flap is called the posteriorly based flap. In the other variants, the dominant nutrient vessels are the facial artery and vein.
The donor site in FAMM flaps is closed by primary closure if the width of the defect is considered <2.5 cm.8 In larger defects, it is recommended to cover the defect by mobilizing the buccal fat pad.9
In Ferrari et als10 research on donor site morbidity of buccinator-based myomucosal flaps in 15 patients, no complications were reported. However, in our series, the rate of donor site complications was 20% with minimum limitation in mouth opening. Despite the fact that primary direct closure was the most commonly used method for management of the donor site, the complication rate was lower (8%) in comparison with the buccal fat pad group (43%). This shows the fact that if more mucosa is harvested, the complications will increase. It is accepted that postoperative radiotherapy with the masticatory muscles in the field of radiation has a negative effect in mouth opening.11 In the present study, four patients had such condition and only one of them experienced a decrease in MIO. In this case, MIO limitation occurs before the radiotherapy. Postoperative radiotherapy may have a cumulative negative effect on mouth opening. There was no case of sialocele formation due to Stensen duct injury. This fact showed that the surgeon strictly adhered to the principles of FAMM flap elevation. The location of the paddle in the FAMM flap was anterior to the Stensen duct and in the island variants superior incision was performed 2–5 mm bellow the parotid duct opening.12 ; 13
Obliteration of the mandibular vestibule indicated that the surgeon had harvested the mucosa using inferior incision to the depth of the lower vestibule. Therefore, when the defect is covered by the buccal fat pad, the wound contracture during the secondary epithelialization process leads to obliteration of the vestibule. To prevent this problem, the suggested technique involves retaining the mandibular vestibular mucosa while the underlying buccinator muscle is included in the flap.Using this strategy, the maximum paddle size is obtained and the mandibular vestibular depth remains undisturbed.
In one patient, it was not possible to herniate the buccal fat pad into the surgical field after incising the buccopharyngeal fascia. This might occur in thin-faced patients, and the surgeon should have an alternative plan to solve this problem. In such cases the masseter muscle flap is a good option.14
5. Conclusion
Donor site morbidity related to buccinator-based myomucosal flaps is low. However, minimal reduction of mouth opening occurred in 20% of patients.
Acknowledgments
This study was supported by a grant from the Vice Chancellor of Research of Mashhad University of Medical Sciences (920847), Mashhad, Iran.
References
- 1 A. Rahpeyma, S. Khajehahmadi, H.N. Rezvani; Pedicle length in the inferiorly based buccinator myomucosal island flap: a cadaveric study; Int J Oral Maxillofac Surg, 43 (2014), pp. 173–176
- 2 K. Khan, V. Hinckley, O. Cassell, P. Silva, S. Winter, M. Potter; A novel use of the facial artery based buccinator musculo-mucosal island flap for reconstruction of the oropharynx; J Plast Reconstr Aesthet Surg, 66 (2013), pp. 1365–1368
- 3 T.M. Sasaki, B.A. Standage, H.W. Baker, D.B. McConnell, R.M. Vetto; The island cheek flap: repair of cervical esophageal stricture and new extended indications; Am J Surg, 147 (1984), pp. 650–653
- 4 J.B. Heller, J.S. Gabbay, A. Trussler, M.M. Heller, J.P. Bradley; Repair of large nasal septal perforations using facial artery musculomucosal (FAMM) flap; Ann Plast Surg, 55 (2005), pp. 456–459
- 5 A. Rahpeyma, S. Khajehahmadi; Buccinator-based myomucosal flaps in intraoral reconstruction: a review and new classification; Natl J Maxillofac Surg, 4 (2013), pp. 25–32
- 6 F. Thomas, F. Ozanne, G. Mamelle, P. Wibault, F. Eschwege; Radiotherapy alone for oropharyngeal carcinomas: the role of fraction size (2 Gy vs 2.5 Gy) on local control and early and late complications; Int J Radiat Oncol Biol Phys, 15 (1988), pp. 1097–1102
- 7 S. Ferrari, A. Balestreri, B. Bianchi, A. Multinu, A. Ferri, E. Sesenna; Buccinator myomucosal island flap for reconstruction of the floor of the mouth; J Oral Maxillofac Surg, 66 (2008), pp. 394–400
- 8 P. O'Leary, T. Bundgaard; Good results in patients with defects after intraoral tumour excision using facial artery musculo-mucosal flap; Dan Med Bull, 58 (2011), p. A4264
- 9 C. Szeto, J. Yoo, G.M. Busato, J. Franklin, K. Fung, A. Nichols; The buccinator flap: a review of current clinical applications; Curr Opin Otolaryngol Head Neck Surg, 19 (2011), pp. 257–262
- 10 S. Ferrari, A. Ferri, B. Bianchi, C. Copelli, P. Boni, E. Sesenna; Donor site morbidity using the buccinator myomucosal island flap; Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 111 (2011), pp. 306–311
- 11 R. Lee, N. Slevin, B. Musgrove, R. Swindell, A. Molassiotis; Prediction of post-treatment trismus in head and neck cancer patients; Br J Oral Maxillofac Surg, 50 (2012), pp. 328–332
- 12 A. Rahpeyma, A.H. Jafarian, S. Khajeh Ahmadi, J. Sarabadani; A schwannoma of the soft palate in a child: histological and immunohistochemical features and surgical method; Iran J Otorhinolaryngol, 24 (2012), pp. 95–99
- 13 J. Pribaz, W. Stephens, L. Crespo, G. Gifford; A new intraoral flap: facial artery musculomucosal (FAMM) flap; Plast Reconstr Surg, 90 (1992), pp. 421–429
- 14 L.H. Marinho, D.A. Shanahan, J.D. Langdon, C.S. Sinnatamby; The inferiorly based masseter muscle flap: anatomical basis for its use in head and neck reconstructive surgery; Int J Oral Maxillofac Surg, 20 (1991), pp. 100–105
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?