Highlights
- Raised artery pulmonary pressure (PAP) is associated with increased mortality.
- We review the eight published echo techniques to assess PAP by echocardiography.
- Knowledge of all the echo techniques could avoid need for invasive tests.
- A scoring system combining various echo-derived measurements of PAP is needed.
Abstract
Pulmonary hypertension is a pathological haemodynamic condition defined as an increase in mean pulmonary arterial pressure ≥ 25 mmHg at rest, assessed using gold standard investigation by right heart catheterisation. Pulmonary hypertension could be a complication of cardiac or pulmonary disease, or a primary disorder of small pulmonary arteries. Elevated pulmonary pressure (PAP) is associated with increased mortality, irrespective of the aetiology. The gold standard for diagnosis is invasive right heart catheterisation, but this has its own inherent risks. In the past 30 years, immense technological improvements in echocardiography have increased its sensitivity for quantifying pulmonary artery pressure (PAP) and it is now recognised as a safe and readily available alternative to right heart catheterisation. In the future, scores combining various echo techniques can approach the gold standard in terms of sensitivity and accuracy, thereby reducing the need for repeated invasive assessments in these patients.
Keywords
Pulmonary hypertension by echo ; Pulmonary pressure by echocardiography ; Tricuspid Regurgitation Vmax ; Pulmonary acceleration time ; Pulmonary vascular resistance by echo
Pulmonary hypertension (PHT) is a pathological haemodynamic condition defined as an increase in mean pulmonary arterial pressure (mPAP) ≥ 25mmHg at rest, assessed using gold standard investigation by right heart catheterisation [1] . Pulmonary hypertension could be a complication of cardiac or pulmonary disease or a primary disorder of small pulmonary arteries. Transthoracic echocardiography (TTE) can be used to investigate and quantify pulmonary artery pressure (PAP). Elevated pulmonary pressure (PAP), measured by echocardiography, is associated with increased mortality, irrespective of the aetiology [2] . In addition, TTE can be used to assess the contribution of left ventricular systolic and diastolic dysfunction, valve function, and congenital lesions to the aetiology of PHT. Assessment can be challenging due to the complex pyramidal shape and retrosternal position of the right ventricle (RV) anatomy and load-dependent nature of the RV functional indices [3] and [4] . While TTE is not the gold standard, it is a readily available bedside technique accepted as the primary non-invasive tool in the assessment of PAP [5] . We present the common techniques currently in use, their advantages, disadvantages, and pitfalls in the echocardiographic measurement of pulmonary pressure.
1. Pulmonary artery systolic pressure by TR peak velocity
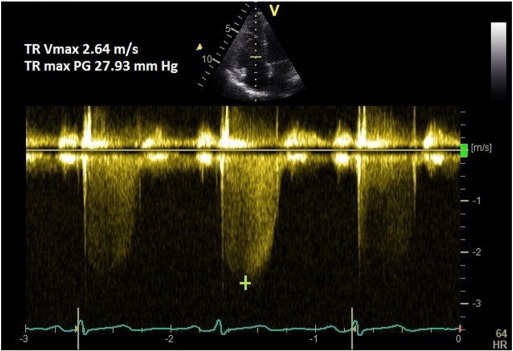
Continuous wave (CW) Doppler of the tricuspid regurgitation (TR) trace is used to measure the difference in pressures between the right ventricle and right atrium. The simplified Bernoulli equation (P = 4[TRmax]2 ) is used to calculate this pressure difference using peak TR velocity. This method correlates well with PASP on right heart catheterisation [6] and [7] . A peak TR velocity value of ≤ 2.8 m/s is considered normal.
1.1. Method
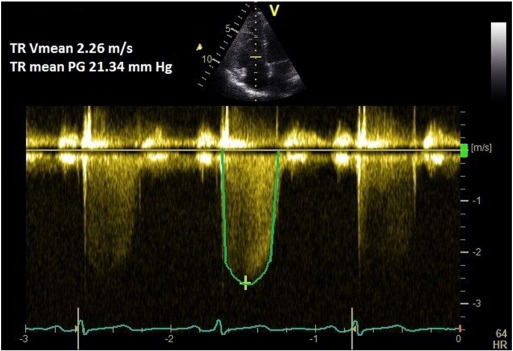
A coaxial TR jet is identified in parasternal long axis (RV inflow), parasternal short axis, or apical 4-chamber view with the help of colour Doppler. CW Doppler is used with a sweep speed of 100 mm/s to achieve a satisfactory envelope (Fig. 1 ). The peak velocity of the envelope is then measured (TRmax ). A value of ≤ 2.8 m/s suggests low probability, a value of 2.9–3.4 m/s indicates intermediate probability, and a value > 3.4 m/s suggests a high probability for pulmonary hypertension [1] . Traditionally, right atrial pressure (RAP) is assumed by the size and distensibility of inferior vena cava (IVC) during inspiration at rest and during forced inhalation, and this value is added to the peak TR velocity [8] . However, recent ESC guidelines suggest just using the TRmax without additional RAP, as IVC assessment is error prone [1] . Mean PAP can be approximated from the systolic PAP (SPAP) using the following formula: mPAP = 0.61*SPAP + 2 mmHg [9] .
|
|
|
Fig. 1. TR Vmax method for measuring PASP. |
If there is marked sinus arrhythmia, the trace should be obtained at expiratory apnoea. If the patient is in atrial fibrillation, then 8 consecutive TR velocities are averaged to give the best estimate [7] . In case of pulmonary valve or right ventricular outflow tract (RVOT) stenosis, this method overestimates the PASP; then the peak pressure gradient across the valve or RVOT should be subtracted from the measured PASP.
1.2. Common pitfalls
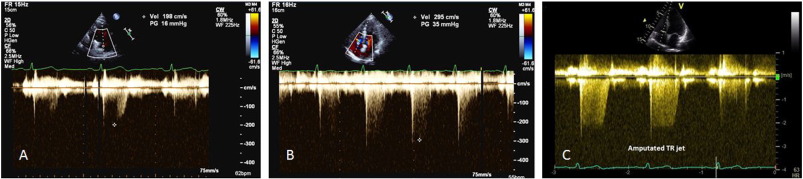
A lesser degree of TR may occur in a compensated right ventricle (due to elevated ventricular pressure) and this could lead to underestimation of PASP. Similarly, severe TR could cause equalisation of right atrial and ventricular pressures which may cause the TR Doppler envelope to be cut short, leading to underestimation of PASP (Fig. 2 -C) [8] . RAP is often overestimated if IVC measurement is used, leading to overestimation of PASP [10] . Calculations using the TR trace assume that there is no pulmonary valve stenosis and may be inaccurate in the presence of RV systolic dysfunction. TR signal could be poor in a good proportion of patients with lung disease, and TRmax measurement should be avoided in the absence of a good Doppler envelope (Fig. 2 ) [11] .
|
|
|
Fig. 2. Pitfalls in TR peak measurement. A, B—Peak TR measurement with incomplete trace could lead to underestimation. C—Amputated jet could occur in severe TR that could lead to underestimation. |
1.3. Tricks
- The best TR signal is often “off-axis,” in-between parasternal and apical windows. An RV-focussed or fore shortened 4-chamber view might give the best signal [12] . Sometimes, subcostal long and short axis windows provide the optimal signal and incident angle.
- The frame rate should be optimised to ≥ 20 Hz with colour Doppler.
- The faster the heart rate, the higher the frame rate needed to assess regurgitant jets.
- If the TR signal is poor, consider intravenous agitated saline.
2. Mean pulmonary artery pressure from peak PR Doppler signal
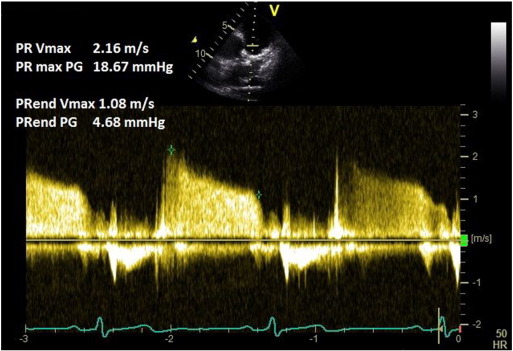
2.1. Method
A pulmonary regurgitation (PR) signal is obtained in the parasternal short axis view using colour Doppler. CW Doppler at a sweep speed of 100 mm/s is used to measure the peak PR velocity (Fig. 3 ). Peak pressure difference (measured by the Bernoulli equation) is then added to the RAP. This method has been validated against gold standard catheter-measurements [13] and [14] . Mean PAP can be approximated from the peak PR Doppler signal using the following formula: mPAP = 4(PRpeak velocity)2 + RAP.
|
|
|
Fig. 3. Pulmonary regurgitation method for measuring mean and diastolic pulmonary artery pressure. |
2.2. Common pitfalls
The PR signal may be poor or parallel alignment of the Doppler signal may not be possible. In the presence of constrictive or restrictive RV physiology, PR Doppler signals could provide a valuable clue towards the diagnosis but may be unreliable in the calculation of pulmonary artery pressure [15] . In constrictive physiology, there is dissociation of intracardiac from intrathoracic pressure, resulting in early equalisation of PA and RV pressures with inspiration. This results in shorter and steeper PR signal [16] .
2.3. Tricks
- Use multiple views to obtain the PR signal.
- PR is present in most patients with pulmonary hypertension although the converse is not true [14] .
- Agitated saline can improve PR signal.
3. Pulmonary artery diastolic pressure measured by PR-end velocity
3.1. Method
A PR signal is obtained as above. End PR velocity is measured in multiple (non-continuous) traces and averaged. Pulmonary artery diastolic pressure (PADP) is calculated from the following equation: 4(PR-end velocity)2 + RAP. Mean pulmonary artery pressure can be calculated from systolic (by TRmax method) and diastolic (by PR-end velocity method) pulmonary artery pressures:
|
|
3.2. Common pitfalls
In severe pulmonary regurgitation, due to a rapid deceleration slope, PR-end velocity may underestimate the pulmonary artery diastolic pressure [14] . As mentioned earlier, this technique may not be useful in the presence constrictive or restrictive physiology [15] and [16] .
3.3. Tricks
- Use the mean of several measurements.
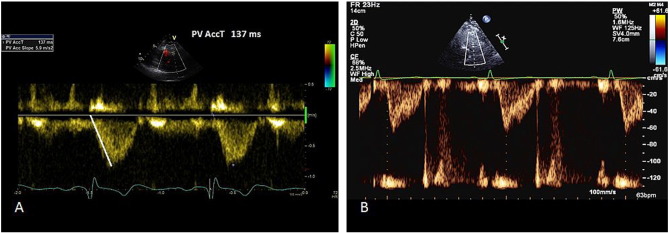
4. Mean pulmonary artery pressure from right ventricular outflow tract (RVOT) acceleration time
Pulse wave of RVOT normally produces a dome shape, but in patients with pulmonary hypertension, there is rapid rise to peak, resulting in shorter acceleration time [17] . A mid-systolic notching could also indicate pulmonary hypertension [17] .
4.1. Method
A pulse wave signal of pulmonic forward flow is obtained at end expiration, just proximal to the pulmonary valve in the parasternal short axis view. The Doppler sample is placed in such a way that the obtained signal has a closing snap but not an opening snap. The quality of the signal is very important and maximum sweep speed must be used to increase accuracy. Furthermore, there should not be spectral broadening.
Right ventricular outflow tract (RVOT) acceleration time is measured from the beginning of the flow to the peak flow velocity (Fig. 4 ). It is important that the marker is placed at the peak first and then tracked back to the onset of flow, as the aim is to measure time taken to peak velocity and not the propagation. A value of > 130 ms is normal, while < 100 ms is highly suggestive of pulmonary hypertension [18] . Mean pulmonary pressure is calculated by the formula: mPAP = 90 − (0.62*ATRVOT ). For example, if the ATRVOT is 80 ms, the mPAP = 90 −(0.62*80), that is 40.4 mmHg (normal < 25 mmHg). On the other hand, if the ATRVOT is 137 ms (as in Fig. 4 ), then the calculated mPAP is 90 −(0.62*137) = 5.06 mmHg.
|
|
|
Fig. 4. RVOT acceleration time method for assessing pulmonary pressure. A—Pulmonary acceleration time measurement. B—Rapid rise and mid-systolic notching suggesting elevated pulmonary pressure. |
4.2. Common pitfalls
Heart rates outside of the normal range (< 60 or > 100 bpm) may reduce the accuracy of this technique. However, when the mean PAP exceeds 25 mmHg, RVOT acceleration time is accurate even in tachycardia [19] and [20] . More often, the slope of the pulse wave Doppler trace is measured, rather than the time taken from onset to peak velocity. This usually leads to underestimation of the RVOT acceleration time.
4.3. Tricks
- Start from the peak of the envelope and measure the time to the onset. Starting from the onset could lead to measurement of the slope and consequently underestimate the time duration.
- During scanning, an easy estimate of mean pulmonary pressure could be made using the formula mPAP = 80 − (0.5*ATRVOT ); this can be used to corroborate the calculated value. For example if ATRVOT = 120 ms, it will be easy to work out mPAP = 80 − 60, i.e. 20 mmHg.
- Mid-systolic notching may also suggest increased pulmonary vascular resistance [21] .
5. Mean pulmonary artery pressure from TR velocity-time integral
5.1. Method
In this fairly new technique, CW Doppler of the TR jet is traced and the mean pressure difference is measured from the velocity-time integral (VTI) (Fig. 5 ). RAP is then added to calculate the mPAP. Mean PAP measured by this method correlates closely with catheter-measured mPAP [22] . The mPAP from TR VTI can be calculated using the following formula: mPAP = meanΔP + RAP.
|
|
|
Fig. 5. Tricuspid regurgitation velocity-time integral method for measuring mPAP. |
5.2. Common pitfalls
A complete TR envelope may not be possible in all patients. Inaccurate RA pressure measurement leads to over or underestimation of mPAP.
5.3. Tricks
- Use agitated saline to improve CW Doppler signal.
6. RV free wall strain Sm , Sm VTI
6.1. Method
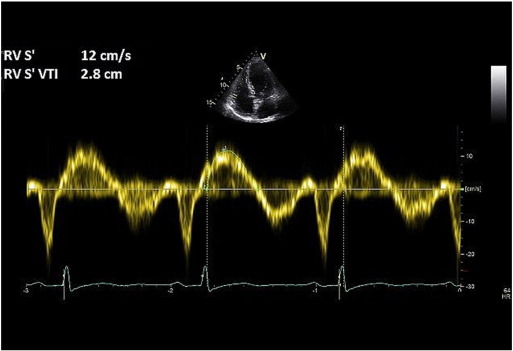
Tissue Doppler imaging (TDI) is used on the RV free wall in the apical 4-chamber view, and tricuspid annular systolic myocardial (Sm ) velocity is recorded. The maximal Sm velocity and the Sm VTI are then measured (Fig. 6 ). Sm velocity < 12 cm/s and Sm VTI < 2.5 are highly suggestive of elevated PASP [23] .
|
|
|
Fig. 6. RV tissue Doppler method for assessing pulmonary pressure. |
6.2. Common pitfalls
This method correlates well with TR measured PASP but is yet to be fully validated against the gold standard-invasive right heart catheterisation [23] and [24] . Although the technique helps to identify patients with pulmonary hypertension, it cannot accurately quantify pulmonary artery pressure.
6.3. Tricks
- Obtain maximum TDI frame rate by narrowing the sector width.
- An RV-focussed apical 4-chamber view might reduce the incident angle on the tissue Doppler.
- A larger pulse gate might provide a complete signal, by capturing some of the myocardium throughout annular descent.
7. Right ventricular isovolumic relaxation time (r IVRT)
7.1. Method
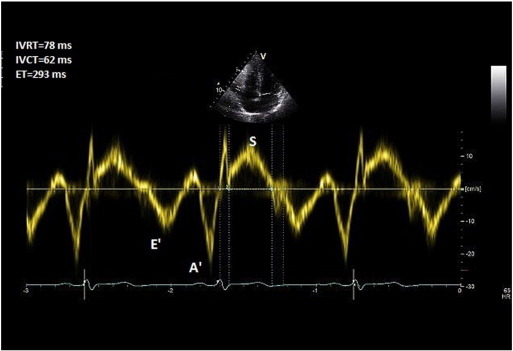
TDI is deployed at the lateral tricuspid annulus with a sweep speed of 100 mm/s. Pulse wave (PW) Doppler with a 6 mm sample window is obtained. Right ventricular isovolemic relaxation time (r IVRT) is measured from the offset of the S′ wave to the onset of the E’ wave (Fig. 7 ). r IVRT of > 75 ms reliably predicts pulmonary hypertension while an r IVRT of < 40 ms has a high negative predictive value for pulmonary hypertension [25] and [26] .
|
|
|
Fig. 7. Right ventricular isovolemic relaxation time measurement. |
7.2. Common pitfalls
Coaxial tricuspid TDI is may not be possible in all patients and incident angle should be no more than 15°. The technique may become unreliable in hypertrophic cardiomyopathy, right bundle branch block and right ventricular dysfunction because the r IVRT is prolonged for other reasons. On the other hand, r IVRT is pseudo-normalised in the presence of elevated RAP and significant TR [27] .
7.3. Tricks
- When the heart rate is high, use the rate corrected r IVRT (r r IVRT’; which i.e. r IVRT/√RR interval on ECG) [20] .
- Increase the pulse gate as mentioned earlier, to obtain a complete signal
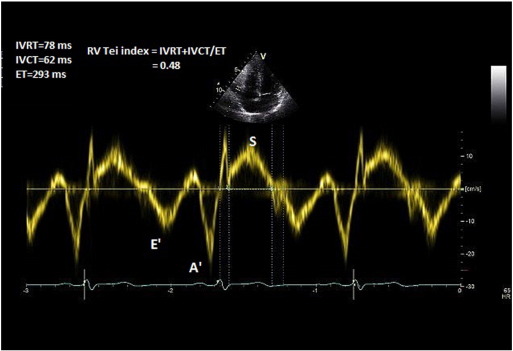
8. Tei index and TR measured PASP
Tei index was introduced in 1990s as a Doppler-derived marker of ventricular function. Vonk et al. showed that combining TR-measured PASP (≥ 35 mmHg) with Tei index (> 36) improves echocardiographic sensitivity for the diagnosis of pulmonary hypertension [28] .
8.1. Method
In the apical 4-chamber view, TDI is deployed on the RV free wall and a 3–5 mm pulse wave Doppler is obtained approximately 1 cm from the tricuspid annulus. Isovolemic contraction time (IVCT), isovolemic relaxation time (IVRT), and ejection time (ET) of the RV are then measured (Fig. 8 ). Alternatively, these measures could be obtained from CW Doppler across the RV inflow/TR jet. Tei index is measured by the formula: Tei Index (RV) = IVRT + IVCT/ET.
|
|
|
Fig. 8. Measurement of Tei index. |
8.2. Common pitfalls
The method was studied in small groups of patients and has not yet been validated in larger sample sizes [28] and [29] . Tei index is, however, proven to prognosticate patients with pulmonary hypertension [30] .
9. Pulmonary vascular resistance
An elevated pulmonary vascular resistance (PVR) in a patient with PHT suggests that the primary pathology to be the pulmonary vasculature rather than the left heart. A value of > 3 Wood units measured by gold standard technique-right heart catherisation (RHC) indicates raised PVR [1] . While RHC should be performed for conclusive diagnosis, ratio of Peak TR velocity to VTIRVOT measured by echocardiography could provide a valuable clue in PVR assessment.
9.1. Method
A TR trace (CW Doppler) is obtained from several views. If needed, agitated saline is administered intravenously to improve the envelope and the maximal TR velocity is measured. A 1–2 cm PW Doppler is then placed in the RVOT (parasternal short axis view), just within the pulmonary valve. The sample volume is placed so that only the closing click of the pulmonary valve is visualised, and the VTI of the RVOT (VTIRVOT ) Doppler signal is measured. A ratio of Peak TR velocity to VTIRVOT of ≤ 0.15 is considered normal. Pulmonary vascular resistance (PVR) is measured by the formula: PVR = (Peak TR velocity (m/s)/VTIRVOT (cm)*10) + 0.16 [32] . TTE measurement of PVR is not fully validated to initiate or monitor treatment of PHT [33] . This method should not replace invasive measurement by right heart catherisation.
10. Other observations on TTE during assessment of pulmonary hypertension
Table 1 shows the other echo observations that are useful in assessing patients for pulmonary pressure.
| Observation | Inference |
|---|---|
| RVH and dilationRA dilationdecreased deceleration time of early mitral inflow | RV pressure overload |
| Systolic flattening of the IVSD-shaped LV with reduced diastolic and systolic volumes with preserved systolic function | RV pressure overload |
| Coronary sinus dilation | Elevated RA pressure |
| IVC (hepatic vein dilation) with reduced or absent collapse on sniff | Elevated RA pressure |
| Pericardial effusion | Impaired lymphatic drainage, secondary to elevated right ventricular pressure |
| Large TR | RV enlargement and tethering of the leaflets towards the apex. |
| Raised RV myocardial performance index (Tei index) | RV dysfunction |
11. PAP measurement during exercise
Bourlag et al. and Nagel et al. showed that pulmonary artery pressure rises significantly during exercise in patients with latent PHT compared to healthy subjects [34] and [35] . This increase occurs early during loaded exercise making it amenable to measurement. TR Vmax measured PASP of > 45 mmHg or a rise of > 20 mmHg during low-intensity exercise (while not exceeding a cardiac output of 10 l/min) is diagnostic for latent PHT with moderate sensitivity and specificity [35] and [36] . However, this cut-off should not be applied to athletes and the elderly who may reach a PASP of 55-60 mmHg on exercise [3] .
Talreja et al. demonstrated that elevated mitral E/E′ during exercise as another non-invasive measure of elevated left atrial and thereby pulmonary capillary wedge pressure (PCWP) [37] . An E/E′ value of > 15 during exercise predicted an elevated catheter-measured PCWP. Ha et al. also showed that exercise mitral E/E′ is a reliable measure in predicting indolent PHT due to left heart disease in patients with normal resting pulmonary pressure [38] . Other methods are not validated for the evaluation of pulmonary pressure during exercise.
12. Conclusion
Echocardiography can be used to diagnose pulmonary hypertension with good accuracy. With recent advances in the field, it is of paramount importance that the cardiologist is aware of the nuances in the echo measurement of pulmonary artery pressure. In future, a scoring system combining various echo-derived measurements of PAP in conjunction with exercise testing, might more accurately identify and assess progress of PHT in patients, and reduce the need for invasive assessments.
Conflict of interest
The authors certify that they have no affiliations with or involvement in any organisation or entity with any financial interest in the subject matter or materials discussed in this manuscript.
References
- [1] N. Galiè, M. Humbert, J.-L. Vachiery, et al.; 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension; Eur. Heart J., 29 (August 2015) http://dx.doi.org/10.1093/eurheartj/ehv317 (published online)
- [2] G. Strange, D. Playford, S. Stewart, et al.; Pulmonary hypertension: prevalence and mortality in the Armadale echocardiography cohort; Heart, 98 (24) (2012), pp. 1805–1811
- [3] E. Bossone, A. D'Andrea, M. D'Alto, et al.; Echocardiography in pulmonary arterial hypertension: from diagnosis to prognosis; J. Am. Soc. Echocardiogr., 26 (1) (2013), pp. 1–14
- [4] F. Haddad, S.A. Hunt, D.N. Rosenthal, et al.; Right ventricular function in cardiovascular disease, part I: anatomy, physiology, aging, and functional assessment of the right ventricle; Circulation, 117 (11) (2008), pp. 1436–1448
- [5] S. Lafitte, X. Pillois, P. Reant, et al.; Estimation of pulmonary pressures and diagnosis of pulmonary hypertension by Doppler echocardiography: a retrospective comparison of routine echocardiography and invasive hemodynamics; J. Am. Soc. Echocardiogr., 26 (5) (2013), pp. 457–463
- [6] P.J. Currie, J.B. Seward, K.L. Chan, et al.; Continuous wave Doppler determination of right ventricular pressure: a simultaneous Doppler-catheterization study in 127 patients; J. Am. Coll. Cardiol., 6 (4) (1985), pp. 750–756
- [7] P.G. Yock, R.L. Popp; Noninvasive estimation of right ventricular systolic pressure by Doppler ultrasound in patients with tricuspid regurgitation; Circulation, 70 (4) (1984), pp. 657–662
- [8] L.G. Rudski, W.W. Lai, J. Afilalo, et al.; Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography; J. Am. Soc. Echocardiogr., 23 (7) (2010), pp. 685–713
- [9] D. Chemla, V. Castelain, M. Humbert, et al.; New formula for predicting mean pulmonary artery pressure using systolic pulmonary artery pressure*; Chest, 126 (4) (2004), pp. 1313–1317
- [10] M.R. Fisher, P.R. Forfia, E. Chamera, et al.; Accuracy of Doppler echocardiography in the hemodynamic assessment of pulmonary hypertension; Am. J. Respir. Crit. Care Med., 179 (7) (2009), pp. 615–621
- [11] M. Taleb, S. Khuder, J. Tinkel, et al.; The diagnostic accuracy of Doppler echocardiography in assessment of pulmonary artery systolic pressure: a meta-analysis; Echocardiography, 30 (3) (2013), pp. 258–265
- [12] K. Addetia, M. Yamat, A. Mediratta, et al.; Comprehensive two-dimensional interrogation of the tricuspid valve using knowledge derived from three-dimensional echocardiography; J. Am. Soc. Echocardiogr., 29 (1) (2016), pp. 74–82
- [13] A.E. Abbas, F.D. Fortuin, N.B. Schiller, et al.; Echocardiographic determination of mean pulmonary artery pressure; Am. J. Cardiol., 92 (11) (2003), pp. 1373–1376
- [14] T. Masuyama, K. Kodama, A. Kitabatake, et al.; Continuous-wave Doppler echocardiographic detection of pulmonary regurgitation and its application to noninvasive estimation of pulmonary artery pressure; Circulation, 74 (3) (1986), pp. 484–492
- [15] S. Kaga, T. Mikami, Y. Takamatsu, et al.; Quantitative and pattern analyses of continuous-wave Doppler–derived pulmonary regurgitant flow velocity for the diagnosis of constrictive pericarditis; J. Am. Soc. Echocardiogr., 27 (11) (2014), pp. 1223–1229
- [16] G. Gilman, S.R. Ommen, W.H. Hansen, et al.; Doppler echocardiographic evaluation of pulmonary regurgitation facilitates the diagnosis of constrictive pericarditis; J. Am. Soc. Echocardiogr., 18 (9) (2005), pp. 892–895
- [17] A. Kitabatake, M. Inoue, M. Asao, et al.; Noninvasive evaluation of pulmonary hypertension by a pulsed Doppler technique; Circulation, 68 (2) (1983), pp. 302–309
- [18] A. Dabestani, G. Mahan, J.M. Gardin, et al.; Evaluation of pulmonary artery pressure and resistance by pulsed Doppler echocardiography; Am. J. Cardiol., 59 (6) (1987), pp. 662–668
- [19] A. Milan, C. Magnino, F. Veglio; Echocardiographic Indexes for the Non-Invasive Evaluation of Pulmonary Hemodynamics; J. Am. Soc. Echocardiogr., 23 ((3) (2010), pp. 225–239
- [20] J.A. Mallery, J.M. Gardin, S.W. King, et al.; Effects of heart rate and pulmonary artery pressure on Doppler pulmonary artery acceleration time in experimental acute pulmonary hypertension; Chest, 100 (2) (1991), pp. 470–473
- [21] J.S. Arkles, A.R. Opotowsky, J. Ojeda, et al.; Shape of the right ventricular Doppler envelope predicts hemodynamics and right heart function in pulmonary hypertension; Am. J. Respir. Crit. Care Med., 183 (2) (2011), pp. 268–276
- [22] J.F. Aduen, R. Castello, M.M. Lozano, et al.; An alternative echocardiographic method to estimate mean pulmonary artery pressure: diagnostic and clinical implications; J. Am. Soc. Echocardiogr., 22 (7) (2009), pp. 814–819
- [23] M. Melek, O. Esen, A.M. Esen, et al.; Tissue Doppler evaluation of tricuspid annulus for estimation of pulmonary artery pressure in patients with COPD; Lung, 184 (3) (2006), pp. 121–131
- [24] T. Constantinescu, S.L. Magda, R. Niculescu, et al.; New echocardiographic techniques in pulmonary arterial hypertension vs. right heart catheterization – a pilot study; Maedica, 8 (2) (2013), pp. 116–123
- [25] D. Dawson, J. Grapsa, P. Nihoyannopoulos, et al.; Protocol for the assessment of patients with suspected pulmonary hypertension; British Society of Echocardiography (2011) (Online article, URL- http://www.bsecho.org/guideline-protocol-for-assessment-of-patients-with-suspected-pulmonary-hypertension/ )
- [26] S.Z.M. Ojaghi Haghighi, M. Karvandi, F. Noohi, et al.; Evaluation of correlation between isovolumic relaxation time and pulmonary artery pressure by tissue Doppler imaging; Eur. Heart J. Cardiovasc. Img., 6 (Suppl. 1) (2005), pp. S32–S33
- [27] N. Bréchot, L. Gambotti, S. Lafitte, et al.; Usefulness of right ventricular isovolumic relaxation time in predicting systolic pulmonary artery pressure; Eur. Heart J. Cardiovasc. Img., 9 (4) (2008), pp. 547–554
- [28] M.C. Vonk, M.H. Sander, F.H.J. Van Den Hoogen, et al.; Right ventricle Tei-index: a tool to increase the accuracy of non-invasive detection of pulmonary arterial hypertension in connective tissue diseases; Eur. Heart J. Cardiovasc. Img., 8 (5) (2007), pp. 317–321
- [29] D.G. Blanchard, P.J. Malouf, S.V. Gurudevan, et al.; Utility of right ventricular Tei index in the noninvasive evaluation of chronic thromboembolic pulmonary hypertension before and after pulmonary Thromboendarterectomy; J. Am. Coll. Cardiol. Img., 2 (2) (2009), pp. 143–149
- [30] J.A. Lakoumentas, F.K. Panou, V.K. Kotseroglou, et al.; The Tei index of myocardial performance: applications in cardiology; Hell. J. Cardiol., 46 (1) (2005), pp. 52–58
- [32] A.E. Abbas, F.D. Fortuin, N.B. Schiller, et al.; A simple method for noninvasive estimation of pulmonary vascular resistance; J. Am. Coll. Cardiol., 41 (6) (2003), pp. 1021–1027
- [33] N. Rajagopalan, M.A. Simon, M.S. Suffoletto, et al.; Noninvasive estimation of pulmonary vascular resistance in pulmonary hypertension; Echocardiography, 26 (5) (2009), pp. 489–494
- [34] B.A. Borlaug, R.A. Nishimura, P. Sorajja, et al.; Exercise hemodynamics enhance diagnosis of early heart failure with preserved ejection fraction; Circ. Heart Fail., 3 (5) (2010), pp. 588–595
- [35] C. Nagel, P. Henn, N. Ehlken, et al.; Stress Doppler echocardiography for early detection of systemic sclerosis-associated pulmonary arterial hypertension; Arthritis Res. Ther., 17 (1) (2015), p. 165
- [36] V. Steen, M. Chou, V. Shanmugam, et al.; Exercise-induced pulmonary arterial hypertension in patients with systemic sclerosis; Chest, 134 (1) (2008), pp. 146–151
- [37] D.R. Talreja, R.A. Nishimura, J.K. Oh; Estimation of left ventricular filling pressure with exercise by Doppler echocardiography in patients with normal systolic function: a simultaneous echocardiographic–cardiac catheterization study; J. Am. Soc. Echocardiogr., 20 (5) (2007), pp. 477–479
- [38] J.-W. Ha, J.K. Oh, P.A. Pellikka, et al.; Diastolic stress echocardiography: a novel noninvasive diagnostic test for diastolic dysfunction using supine bicycle exercise Doppler echocardiography; J. Am. Soc. Echocardiogr., 18 (1) (2005), pp. 63–68
Document information
Published on 19/07/16
Licence: CC BY-NC-SA license
Share this document
Keywords
claim authorship
Are you one of the authors of this document?