Summary
Background
Radioembolization with yttrium microspheres is an established therapeutic modality for primary and secondary hepatic malignancies, with studies demonstrating improved overall survival. There remains a paucity of data on cholecystitis as a complication of radioembolization. We describe a small series of patients who developed cholecystitis as a result of radioembolization.
Methods
Patients who had developed cholecystitis as a complication of radioembolization in our institution between 2001 and 2012 were retrospectively reviewed. Patient demographics, cancer details including treatment history, and procedural details of radioembolization and complications of cholecystitis were collected.
Results
Of 74 patients who underwent radioembolization using yttrium-90emitting microspheres, four (5.4%) presented with acute cholecystitis as a result of their treatment. All patients presented over 4 weeks following radioembolization and did not settle with conservative treatment. At surgery, the gallbladder was fibrotic and contracted in all cases making surgery difficult.
Conclusion
The incidence of symptomatic radiation cholecystitis after radioembolization is low, and prophylactic cholecystectomy is not routinely recommended for patients undergoing radioembolization. Radiation cholecystitis should be suspected in patients presenting with symptoms of biliary colic or cholecystitis following radioembolization. Early cholecystectomy can be considered in patients undergoing surgery for other indications, especially in high-risk surgical patients in whom there is a high likelihood of radioembolization in the future as they do not respond to conservative treatment.
Keywords
cholecystectomy;gallbladder;interventional oncology;radioembolization;yttrium-90
1. Introduction
Radioembolization with yttrium-90 (90Y)-emitting microspheres used alone or in combination with systemic chemotherapy is increasingly recognized as an effective therapy for both primary and secondary hepatic malignancies.1 Several studies have suggested an improved overall survival with the addition of radioembolization to chemotherapy.2 ; 3 The aim of pretherapeutic assessment is to establish that safe and effective delivery of the microspheres is possible. This involves radiological assessment of tumoral and nontumoral volumes, portal vein patency, and identification of extrahepatic disease.4 ; 5
Gastrointestinal complications commonly associated with the use of radioembolization include abdominal pain, nausea, vomiting, diarrhea, and transient change in liver function tests. Major complications reported include radiation induced hepatitis, radiation gastritis and gastric ulceration, radiation pneumonitis, and radiation-induced cirrhosis.6 ; 7 There is a paucity of data on cholecystitis as a complication of radioembolization, and the pathogenesis of radiation cholecystitis remains unclear. The incidence of biliary complications postradioembolization is < 10%, of these < 1% require intervention.8
We describe a small series of patients who developed cholecystitis as a result of radioembolization and discuss the role of elective prophylactic cholecystectomy in high-risk surgical patients who may develop symptomatic radiation cholecystits.
2. Methodology
A retrospective review of patients who underwent radioembolization using 90Y-emitting microspheres at The Canberra Hospital from 2001 to 2012 was undertaken to identify cases of cholecystitis. Patient demographics, cancer details including treatment history, and procedural details of radioembolization and complications of cholecystitis were collected.
Approval for the study was obtained from the Australian Capital Territory (ACT) Human Research Ethics Committee, The Canberra Hospital and the requirement for informed consent was waived as the study did not involve an intervention and there was no breach of privacy or anonymity.
3. Results
Of 74 patients who underwent radioembolization using 90Y-emitting microspheres, four (5.4%) presented with acute cholecystitis as a result of their treatment.
3.1. Case 1
A 77-year-old woman presented to hospital with acute large bowel obstruction due to an obstructing cancer in the sigmoid colon and underwent a Hartmans procedure. Post operatively, she was commenced on adjuvant three-times weekly oral capecitabine and received a total of eight cycles. One month postcompletion of adjuvant therapy, she presented with metastatic disease involving segments IVb and V of the liver, a pelvic node and the left ovary. She underwent metastectomy of two pelvic metastatic deposits and resection of the two liver metastases. Histopathology confirmed metastatic adenocarcinoma from a bowel primary with complete margins of excision. She was commenced on further adjuvant therapy with the XELOX protocol of oxaliplatin in combination with capecitabine, completing six cycles. Follow-up imaging showed several new unresectable metastases involving both lobes of the liver. Her chemotherapy regimen was changed to FOLFIRI (5-fluorouracil with irinotecan and leucovorin) with bevacizumab, and was referred for consideration of radioembolization of the liver. Angiography prior to implantation showed a prominent right gastric artery, which was embolized prior to treatment. A total of 1.36 GBq of 90Y microspheres was implanted into the liver with 0.27 GBq and 1.09 GBq being delivered to the left and right lobes respectively. The procedure was well tolerated with no immediate complications. Six weeks postprocedure, the patient was admitted to hospital, with acute right upper quadrant pain and fever. Ultrasound showed features consistent with cholecystitis. Despite prolonged treatment with intravenous antibiotics, she remained symptomatic and underwent a laparoscopic cholecystectomy. Histopathology showed chronic cholecystitis, with cholelithiasis, as well as 90Y resin spheres in the gallbladder wall. She made an uneventful recovery.
3.2. Case 2
A 31-year-old woman with no significant medical history, underwent a wide local resection with lymph node clearance for multifocal node positive breast cancer. She was treated with adjuvant chemotherapy plus radiotherapy and continued on hormonal therapy for 5 years. She presented with an acute episode of right upper quadrant pain, which led to the discovery of liver and bony metastases. She was commenced on palliative chemotherapy with docetaxel and capecitabine, and referred for radioembolization. Preprocedure angiography displayed normal hepatic vascular anatomy. Liver tumor load was estimated at 20%. A prominent cystic artery was embolized using coils preimplantation of the spheres. A total of 1.39 GBq of 90Y microspheres was implanted proximal to the cystic artery origin, with 0.42 GBq and 0.97 GBq being delivered to left and right lobes, respectively. Chemotherapy was not given concurrently with the implantation. Four months postimplantation, she presented with severe right upper quadrant pain. Ultrasound showed thickening of the gallbladder wall consistent with chronic gallbladder pathology and she underwent laparoscopic cholecystectomy. Operative findings showed a thick walled gallbladder with multiple metastatic deposits on the gallbladder. Histopathology showed chronic cholecystitis with microsphere deposition, as well as metastatic breast carcinoma infiltration into the subserosa and lymphovascular invasion. The patient made a good postoperative recovery.
3.3. Case 3
A 59-year-old man initially presented with a 3 month history of unresolving right neck swelling and ear ache. Microlaryngoscopy revealed a tumor of the right piriform fossa involving the medial and lateral walls and extending down towards the apex. Biopsies confirmed moderately differentiated squamous cell carcinoma. Given the extent and complexity of surgery, the patient was treated with radical radiotherapy with concurrent cisplatin chemotherapy. Five months after completion of treatment a single liver metastasis was seen on surveillance CT. At operation, however, he was found to have metastatic abdominal lymphadenopathy and liver metastectomy was abandoned. He was planned for radioembolization. Angiography showed the hepatic artery arising from the coeliac axis and this was selectively catheterized to allow delivery to the right lobe. The metastatic disease was entirely within the right lobe, with an estimated tumor load of 10%. A total dose of 2.45 GBq of 90Y microspheres was implanted into the right lobe of the liver without complication. However, at the time of implantation there was intense enhancement of the gallbladder during the time of angiography.
Seven weeks postprocedure he developed increasing right upper quadrant pain associated with a low-grade fever. Ultrasound showed a diffusely inflamed gallbladder with a thickened wall. He was commenced on intravenous antibiotics, but as symptoms did not resolve, open cholecystectomy was performed. At operation the gallbladder was found contracted and adherent to liver and ascending colon. Histology showed extensive areas of mucosal and mural infarction, with numerous spheres present. He had an uneventful postoperative recovery.
3.4. Case 4
A 51-year-old man presented with painless obstructive jaundice. Computed tomography of the abdomen revealed a cecal mass with multiple liver metastases involving both lobes and abdominal lymphadenopathy (porta hepatis, para-aortic, and left gastric). At endoscopic retrograde cholangiopancreatography, a biliary stent was inserted. Colonoscopy confirmed the cecal primary and histopathology showed moderately differentiated adenocarcinoma. He was treated with FOLFOX6 protocol of 5-fluorouracil with leucovorin and oxaliplatin, followed by right hemicolectomy.
After initial treatment he was referred for radioembolization. Hepatic angiography did not reveal any aberrant hepatic anatomy but the right gastric artery was embolized to protect the gastric mucosa during radioembolization. A total of 1.78 GBq of 90Y microspheres was implanted into the liver, which had an estimated tumor load of 20%. No complications were recorded during the procedure. Four weeks postradioembolization; he developed fever, rigors, and back pain. Blood cultures grew Escherichia coli, and ultrasound showed extrahepatic biliary dilation and gallbladder wall thickening. He was commenced on intravenous antibiotics, and referred for endoscopic retrograde cholangiopancreatography to replace his biliary stent. Laparoscopic cholecystectomy was performed with histopathology of gallbladder showing thickening of the gallbladder wall with smooth muscle hypertrophy and patchy chronic inflammation consistent with chronic cholecystitis. Resin microspheres were seen within blood vessels.
4. Discussion
Several studies have demonstrated the efficacy of yttrium-90 radioembolization in the treatment of primary and secondary unresectable hepatic metastases. A large prospective study looking at radiation cholecystitis as a consequence of 90Y radioembolization reported an incidence of 10.1% on radiological findings and an overall incidence of 0.6% requiring cholecystectomy for symptomatic radiation cholecystitis.8 Other studies have shown the incidence of symptomatic radiation cholecystitis after radioembolization to be about 2%.3 ; 4 The spectrum of biliary complications from 90Y radioembolization includes biliary wall thickening and hyperenhancement, development of pericholecystic fluid, gallstones, bile duct injury, and cholecystitis.9
Often, the diagnosis of cholecystitis is clinical, as radiological findings do not always correlate with symptoms and signs.
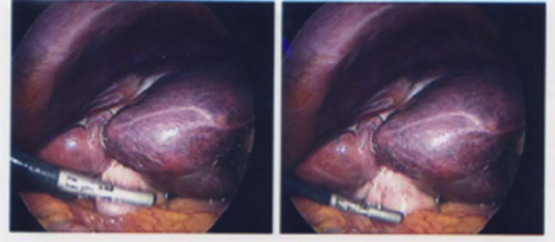
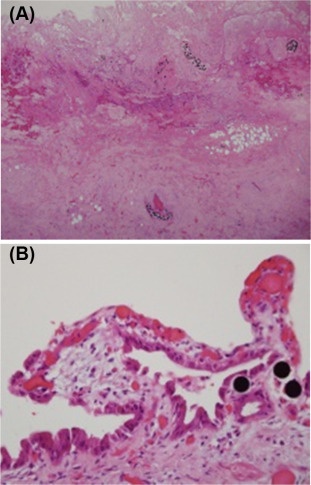
All patients in our series had extensive preprocedural work up with clinical and radiological screening. Review of single-photon emission computed tomography imaging performed following macroaggregated albumin workup and post sphere implantation did not reveal increased radioisotope uptake in the gallbladder although such uptake is difficult to perceive in a hollow viscus such as the gallbladder. In only one case (Case 3) was there intense contrast enhancement of the gallbladder on angiography during the implantation that raised the possibility that the patient might be at risk of radioembolization related cholecystitis. All patients had adequate pretreatment hematologic, hepatic, and renal function. Careful angiographic assessment of the arterial anatomy was carried out in all patients and embolization of any aberrant vessels or any prominent cystic artery as was performed in Case 2. All our patients presented with abdominal pain between 1 month and 4 months of sphere implantation. All patients required cholecystectomy as the symptoms did not resolve with analgesia and antibiotics. Intraoperatively, the gallbladders were found to be fibrotic and contracted (Figure 1). The temporal relationship with radioembolization, fibrosis and inflammation and the presence of microspheres within the gallbladder wall strongly suggested radiation induced cholecystitis (Figure 2). The patients in this series had thick walled contracted gallbladders and livers were stiff due to the effects of chemotherapy and 90Y microspheres making the cholecystectomy particularly difficult.
|
|
|
Figure 1. Intraoperative laparoscopic view of gallbladder. |
|
|
|
Figure 2. (A) Microscopy of infarcted gallbladder wall with spheres in lymphovascular spaces (×100 hematoxylin and eosin). (B) Microscopy of gallbladder mucosa with spheres and atypia (×400 hematoxylin and eosin). |
The pathogenesis of radiation cholecystitis is still unclear. The gallbladder may receive radiation from particles in the gallbladder wall as a consequence of inadvertent injection into the cystic artery or capillaries from the adjacent liver. This radiation alone may be enough to cause serious mucosal damage with subsequent inflammation and fibrosis.10 In a literature review by Riaz et al11 patients with metastatic disease who have received multiple lines of systemic chemotherapy were found to be at higher risk of developing biliary complications. Acute ischemia simply as a result of microspheres occluding circulation in the cystic artery could be a contributing cause. It may be a combination of these factors that is responsible for incidence of radiation cholecystitis associated with radioembolization.
The cystic artery is an end artery that most commonly arises from the right hepatic artery; however, there is variation in the arterial anatomy with the common hepatic, left hepatic, gastroduodenal, and superior mesenteric arteries being possible variant sites of origin. This variation in anatomy may be helpful or a hindrance to the delivery of 90Y avoiding the cystic artery.12 It has been suggested that infusing the 90Ymicrospheres distal to the cystic artery may reduce the incidence of radiation cholecystitis4; however, this may be technically challenging and also result in uneven downstream delivery of microspheres. Temporary occlusion of the cystic artery with a second catheter or cystic artery infusion with saline during implantation has also been suggested, but these techniques have not been tried. In a study by McWilliams et al,13 embolization of the cystic artery using Gelfoam pledgets or coils was evaluated pre-90Y implantation. Despite showing acceptable outcomes cystic artery perforation, recanalisation of the cystic artery, gallbladder toxicity, and technical difficulties using Gelfoam pledgets have been reported with this approach.
The incidence of symptomatic radiation cholecystitis after radioembolization is low, and prophylactic cholecystectomy is not routinely recommended for patients undergoing radioembolization. However, prophylactic cholecystectomy can be considered in patients undergoing surgery for other indications especially in high risk surgical patients in whom there is a high likelihood of radioembolization in the future. Radiation cholecystitis presents 4 weeks or longer following radioembolization and may not resolve with conservative management. All the patients in our experience required surgery with the surgery being difficult due to an adherent and fibrotic gallbladder.
References
- 1 K.M. Sjoquist, D. Goldstein, L. Bester; A serious complication of selected internal radiation therapy: case report and literature review; Oncologist, 15 (2010), pp. 830–835
- 2 A. Saxena, T. Chua, B. Meteling, D. Morris, L. Bester (Eds.), Radioembolization with yttrium-90 microspheres is associated with a significantly improved survival compared to conservative therapy after treatment of unresectable hepatic tumors: a large single center experience of 537 patients. Annals of Surgical Oncology, Springer, New York (2012)
- 3 L. Bester, B. Meteling, N. Pocock, et al.; Radioembolization versus standard care of hepatic metastases: comparative retrospective cohort study of survival outcomes and adverse events in salvage patients; J Vasc Interv Radiol, 23 (2012), pp. 96–105
- 4 R. Murthy, D.B. Brown, R. Salem, et al.; Gastrointestinal complications associated with hepatic arterial yttrium-90 microsphere therapy; J Vasc Interv Radiol, 18 (2007), pp. 553–561
- 5 R. Salem, R.J. Lewandowski, M.F. Mulcahy, et al.; Radioembolization for hepatocellular carcinoma using Yttrium-90 microspheres: a comprehensive report of long-term outcomes; Gastroenterology, 138 (2010), pp. 52–64
- 6 SIRTeX Production information: Available at: http://www.sirtex.com.au/au/clinicians/package-insert/ Accessed 01.12.14.
- 7 J.P. Kuebler; Radioembolization of liver metastases in patients with colorectal cancer: a nonsurgical treatment with combined modality potential; J Clin Oncol, 27 (2009), pp. 4041–4042
- 8 B. Atassi, A.K. Bangash, R.J. Lewandowski, et al.; Biliary sequelae following radioembolization with Yttrium-90 microspheres; J Vasc Interv Radiol, 19 (2008), pp. 691–697
- 9 A.A. Sag, M.A. Savin, N.R. Lal, R.R. Mehta; Yttrium-90 radioembolization of malignant tumors of the liver: gallbladder effects; AJR Am J Roentgenol, 202 (2014), pp. 1130–1135
- 10 A. Kennedy, D. Coldwell, B. Sangro, H. Wasan, R. Salem; Radioembolization for the treatment of liver tumors: general principles; Am J Clin Oncol, 35 (2012), pp. 91–99
- 11 A. Riaz, R.J. Lewandowski, L.M. Kulik, et al.; Complications following radioembolization with yttrium-90 microspheres: a comprehensive literature review; J Vasc Interv Radiol, 20 (2009), pp. 1121–1130
- 12 R. Hickey, R.J. Lewandowski (Eds.), Hepatic radioembolization complicated by radiation cholecystitis. Seminars in Interventional Radiology, Thieme Medical Publishers, Stuttgart (2011)
- 13 J.P. McWilliams, S.T. Kee, C.T. Loh, E.W. Lee, D.M. Liu; Prophylactic embolization of the cystic artery before radioembolization: feasibility, safety, and outcomes; Cardiovasc Intervent Radiol, 34 (2011), pp. 786–792
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?