Summary
Colonic volvulus is a rare disease in children. Delayed diagnosis of the condition can often be fatal, especially in pediatric patients with mental retardation. We herein present the case of a female pediatric patient with colonic volvulus, prune belly syndrome, and mental retardation. Preoperative CT scans showed the characteristic signs of this disease. The volvulus occurred in the proximal colon of the colostomy. The release of the colonic volvulus and reconstruction of the colostomy were performed without the resection of the ischemic colon. The postoperative clinical course was uneventful.
Keywords
colonic volvulus;CT;prune belly syndrome
1. Introduction
Colonic volvulus is a rare disease of bowel obstruction in children and has the potential to be fatal if the diagnosis is delayed. A number of previous studies have indicated that pediatric patients with colonic volvulus also often have mental retardation.1; 2; 3 ; 4 Use of accurate and rapid imaging studies is important for the patient’s outcome. In general, the combination of plain X-ray film and contrast study is undertaken to make a diagnosis of colonic volvulus. Recently, CT scans have been reported to provide useful information for the diagnosis of colonic volvulus.5 However, there have been no reports regarding any colonic volvulus in the site proximal to the colostomy. Therefore, we herein report the case of a mentally retarded Japanese female pediatric patient with a colonic volvulus occurring in the site proximal to the colostomy. The disease was preoperatively diagnosed by both a contrast study and CT scans, thus resulting in the release of the ischemic colon without the need to perform a massive colonic resection.
2. Case report
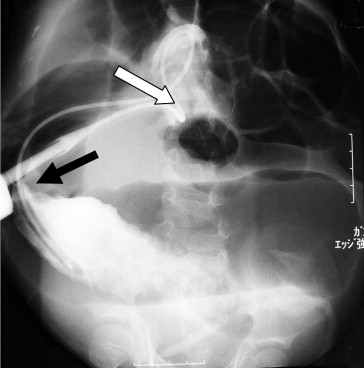
A 5-year-old female was admitted to our institution due to a marked abdominal distention and frequent vomiting. She had previously been diagnosed with prune belly syndrome with multiple congenital anomalies, including atresia ani, during the neonatal period. A transverse loop colostomy and cystotomy had been performed due to the atresia ani during the neonatal period. Mental retardation had also been diagnosed. An abdominal plain X-ray film showed a markedly distended intestine. A Nelaton catheter was inserted from the colostomy into the dilated intestine under fluoroscopic imaging, and a large amount of gas blew out through the tube, resulting in temporary improvement of her symptoms. However, her abdomen gradually became distended again later. A contrast study through the stoma showed a bird’s beak sign-like finding in the site proximal to the colostomy (Fig. 1), and the contrast CT scan revealed the whirl sign at the right upper abdomen near the colostomy (Fig. 2). An emergency laparotomy was performed because the CT scan findings suggested the presence of the volvulus, and the symptoms were recurrent in spite of deflation by means of a catheter. The surgical findings showed a nonrotation type of malrotation and that the total colon therefore was not fixed to the retroperitoneum. A volvulus of the colon existed, with ischemic changes at the site proximal to the colostomy. The dilation of the colon in the site proximal to the colostomy was also noticed. The release of the colonic volvulus led to the improvement of its ischemia. Therefore, a resection of the colon was not performed. The previous loop colostomy was divided into proximal site and distal site. The proximal site of the previous colostomy was fixed to the abdominal wall as a new end colostomy, while the distal site of the previous colostomy was completely closed. The patient’s postoperative course was uneventful, and she was discharged on the 16th day after the operation. During the 2-year follow-up period, no further symptoms of volvulus have been observed.
|
|
|
Figure 1. The contrast enema image demonstrates a tapering of the contrast column (black arrow), which resembles a “bird’s beak sign.” The white arrow shows the position of the colostomy. |
|
|
|
Figure 2. CT demonstrated the “whirl sign” (arrows), with a twisted mesocolon encircling the mesocolic vascular pedicle serving the affected segment of the colon. |
3. Discussion
Intestinal obstruction during the neonatal period mostly results from various complications of congenital anomalies, such as atresia ani, Hirschsprung disease, and jejunoileal atresia/stenosis.6 In addition, intussusception and incarcerated hernia have been reported as common causes of intestinal obstruction in pediatric patients.6; 7 ; 8 Colonic volvulus is an uncommon cause of intestinal obstruction. Only 3% of bowel obstruction cases are secondary to colonic volvulus in adult patients.1 In the pediatric population, the occurrence rate of bowel obstruction caused by colonic volvulus is lower than that in the adult population.1
Several risk factors regarding colonic volvulus have previously been reported, including chronic constipation, postoperative intra-abdominal adhesions, bowel distension, and malrotation.2; 3 ; 9 Colonic volvulus is known to be more common in children with neurological impairment because these children usually have constipation and megacolon. In our case, the patient had multiple risk factors contributing to the development of colonic volvulus, including a previous surgical history, malrotation, mental retardation, and prune belly syndrome. In addition, the location of torsion in our case was unique. Colonic volvulus is usually reported to occur in the sigmoid colon, and less often in the cecum. The transverse colon is rarely involved.1 In our case, the colon in the site proximal to the colostomy was twisted. Torsion of this site has never been reported in the English literature. The bowel hypoperistalsis related to her mental retardation produced a severely dilated colon in the site proximal to the colostomy, which was freely mobile because of malrotation. This dilated and freely mobile colon contributed to the formation of the volvulus around the colostomy, which was loosely sustained by the fragile abdominal wall caused by the patient’s prune belly syndrome.
Early accurate diagnosis is important for pediatric patients with colonic volvulus, especially those with associated neurological impairment, because the clinical symptoms of the condition are often nonspecific, and such children cannot describe their symptoms.3 Jancar et al10 reported that fatal intestinal obstruction often occurred in mentally handicapped patients because these people cannot present their symptoms and often showed deceptively minimal signs and symptoms related to the disease. Therefore, imaging examinations play an important role in making an early diagnosis. The abdominal plain X-ray film is often the first approach.3 In the plain X-ray films of patients with cecal volvulus, the following findings are important for detecting the colonic volvulus: an abnormal position of the dilated cecum, a dilation of the small bowel lying to the right of the distended cecum, and an air–fluid level in the dilated cecum and small bowel.11 However, Anderson et al8 summarized their experience of seven cases with large bowel volvulus in children and concluded that radiological plain film findings were often not characteristic, but were equivocal in the majority of cases. Therefore, contrast enema is thought to be a more reliable diagnostic imaging study and useful for confirming this disease in children.3 The bird’s beak appearance has been described as a typical and important finding in contrast enema studies,3 ; 4 as we observed in our case. However, contrast studies are not always routinely performed in the emergency setting.
A CT scan, therefore, is recommended when a contrast study is not helpful in making a diagnosis. CT scans are considered to be the best diagnostic modality for the evaluation of an acute abdomen, particularly for the diagnosis of the cause and complications of bowel obstructions.12 While both “coffee bean” and “bird’s beak” signs have been reported as CT findings indicating acute colonic volvulus,13 the “whirl” sign is also well known to be a specific sign for colonic volvulus.14 Moreover, CT scanning is helpful not only in making the diagnosis, but also in detecting extraluminal abnormal findings such as fluid collections, abscesses, masses, adenopathy, or wall thickening, in addition to the ability to detect closed-loop obstruction and strangulation.13 Because this kind of information is valuable for surgery, Hashimoto et al5 suggested that prompt abdominal CT is recommended for all patients with intestinal obstructions of unclear etiology. In our case, although the patient had risk factors for a colonic volvulus, the diagnosis had been delayed due to the mental retardation and difficult verbal communication. Findings of the abdominal CT enabled a prompt and accurate diagnosis of colonic volvulus, and its subsequent successful treatment.
Both nonsurgical and surgical procedures have been used for the treatment of colonic volvulus. In the literature, barium and saline enemas, and flexible endoscopic reduction have been reported as nonsurgical treatments.15; 16 ; 17 According to a recent review, endoscopic reduction with or without rectal tube insertion was often recommended for nonsurgical treatment.15 Although some studies have reported the success rate using the endoscopic procedure to range from 78% to 81%, the recurrence rate was quite high, namely from 40% to 60%.15; 16 ; 17 Because of this high recurrence rate after successful endoscopic reduction, elective surgical treatment is generally recommended for high-risk patients.15 ; 16
When nonsurgical treatment is unsuccessful or progressive ischemic changes of the bowel are suspected clinically, surgical treatment should immediately be performed. Resection of the affected colon with simple anastomosis or colostomy should be performed if the affected colon shows severe ischemic changes.3 ; 18 When the colon is viable, the recommended surgical treatment remains controversial in the literature.18 Recurrence rates for nonresectional procedures, such as simple detorsion, detorsion with colopexy, and detorsion with colostomy, have been reported to be 13–14%.18 In addition, detorsion with the resection of a redundant colon has been advocated because of the risk that the volvulus of the redundant colon will occur.18 Therefore, in our case, surgical treatment was chosen because of the rapid recurrence of symptoms after the nonsurgical treatment using decompression by means of a catheter inserted from the colostomy. Since the surgery, the clinical course of our patient has been good without any recurrence.
In conclusion, although colonic volvulus is rare in children, this disease should be suspected when children with mental retardation have symptoms related to bowel obstruction because of the high occurrence of this disease in such patients. In addition, clinicians treating children with mental retardation should use CT scans in cases with nonspecific abdominal symptoms that make an accurate diagnosis difficult.
References
- 1 M.G. Mercado-Deane, E.M. Burton, C.G. Howell; Transverse colon volvulus in pediatric patients; Pediatr Radiol, 25 (1995), pp. 111–112
- 2 T. Kohei, Y. Hamada, M. Sato, et al.; Cecal volvulus in children with mental disability; Pediatr Surg Int, 23 (2007), pp. 1011–1014
- 3 N.J. Vo, S.M. O’Hara, M.H. Alonso; Cecal volvulus: a rare cause of bowel obstruction in a pediatric patient diagnosed pre-operatively by conventional imaging studies; Pediatr Radiol, 35 (2005), pp. 1128–1131
- 4 K. Masumoto, T. Izaki, T. Arima; Cornelia de Lange syndrome associated with cecal volvulus: report of a case; Acta Pediatr, 90 (2001), pp. 701–703
- 5 Y. Hashimoto, S. Shigemoto, A. Nakashima, Y. Murakami, T. Sueda; Successful preoperative diagnosis of a rare bowel obstruction: cecal volvulus; J Gastrointest Surg, 12 (2008), pp. 201–204
- 6 H.C. Filston; Other causes of intestinal obstruction; K.J. Welch, J.G. Randolph, M.M. Ravitch, J.A. O’Neill Jr., M.I. Rowe (Eds.), Pediatric Surgery (4th ed.), Year Book Medical Publishers, Chicago (1986), pp. 895–900
- 7 J.S. Janik, S.H. Ein, R.M. Filler, B. Shandling, J.S. Simpson, C.A. Stephens; An assessment of the surgical treatment of adhesive small bowel obstruction in infants and children; J Pediatr Surg, 16 (1981), pp. 225–235
- 8 J.F. Anderson, O. Eklöf, B. Thomasson; Large bowel volvulus in children—review of a case material and the literature; Pediatr Radiol, 11 (1981), pp. 129–138
- 9 L.B. Chirdan, E.A. Ameh; Sigmoid volvulus and ileosigmoid knotting in children; Pediatr Surg Int, 17 (2001), pp. 636–637
- 10 J. Jancar, C.J. Speller; Fatal intestinal obstruction in the mentally handicapped; J Intellect Disabil Res, 38 (1994), pp. 413–422
- 11 J.P. McGraw, A.J. Kremen, L.G. Right; The Roentgen diagnosis of volvulus of the cecum; Surgery, 24 (1948), pp. 793–804
- 12 E. Delabroousse, P. Sarlieve, N. Sailley; Cecal volvulus: CT findings and correlation with pathophysiology; Emerg Radiol, 14 (2007), pp. 411–415
- 13 A.A. Jabra, E.K. Fishman; Small bowel obstruction in the pediatric patient: CT evaluation; Abdom Imaging, 22 (1997), pp. 466–470
- 14 A. Pinto, F. Pinto, M. Scaglione, R. Grassi, L. Romano; Transverse colon volvulus: appearance on computed tomography; Emerg Radiol, 8 (2001), pp. 227–229
- 15 D. Ören, S.S. Atamanalp, B. Aydinli, et al.; An algorithm for the management of sigmoid colon volvulus and the safety of primary resection: experience with 827 cases; Dis Colon Rectum, 50 (2007), pp. 489–497
- 16 ASGE Standards of Practice Committee, M.E. Harrison, M.A. Anderson, et al.; The role of endoscopy in the management of patients with known and suspected colonic obstruction and pseudo-obstruction; Gastrointest Endosc, 71 (2010), pp. 669–679
- 17 P. Renzulli, C.A. Murer, P. Netzer, M.W. Büchler; Preoperative colonoscopic derotation is beneficial in acute colonic volvulus; Dig Surg, 19 (2002), pp. 223–229
- 18 J. Majeski; Operative therapy for cecal volvulus combining resection with colopexy; Am J Surg, 189 (2005), pp. 211–213
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?