Abstract
Objective
To evaluate the clinical outcomes after total knee arthroplasty (TKA) using the Genesis II posterior stabilized prosthesis with a high-flex insert during the mid-term follow-up and to assess its effect on the Japanese lifestyle.
Materials and methods
Fifty-three consecutive patients (8 men and 45 women) underwent primary TKA. The mean follow-up time was 76 months (5–9 years). Clinical results were assessed with the Japanese Orthopedic Association osteoarthritis knee rating score (JOA knee score), range of motion, and lifestyle changes.
Results
The postoperative JOA knee score improved significantly compared to the preoperative JOA knee score. The mean preoperative flexion range improved from 112° to 123° postoperatively (p < 0.05). Additionally, our findings showed that 39% of patients enjoyed a floor-sitting life preoperatively, but only 30% of patients enjoyed floor-sitting life postoperatively.
Conclusion
The postoperative range of knee motion and JOA knee score improved after TKA using the Genesis II posterior stabilized prosthesis with a high-flex insert, but the number of patients who enjoyed floor-sitting life decreased from 39% to 30% because of feelings of fear and discomfort.
Level of Evidence : Level IV, Therapeutic study
Keywords
Knee ; Arthroplasty ; High flexion ; Genesis II ; Japanese lifestyle
Introduction
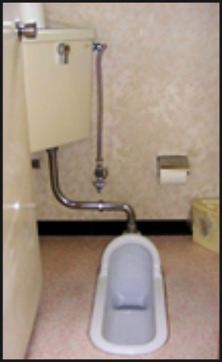
For Japanese people, a high-flexion knee posture is necessary to accommodate their traditional floor-sitting lifestyle.1 Seiza (sitting on the floor with the knees completely flexed) (Fig. 1 ), agura (sitting on the floor cross-legged) (Fig. 2 ), and yokosuwari (sitting on the floor with legs doubled back to one side) (Fig. 3 ) are typical Japanese sitting postures, and each posture requires high knee flexion. Additionally, eating on the floor at a low table, sleeping on a futon, using a Japanese style toilet (Fig. 4 ), and cycling (Fig. 5 ) also require a high knee flexion.
|
|
|
Fig. 1. Seiza. |
|
|
|
Fig. 2. Agura. |
|
|
|
Fig. 3. Yokosuwari. |
|
|
|
Fig. 4. A Japanese style toilet. |
|
|
|
Fig. 5. Cycling. |
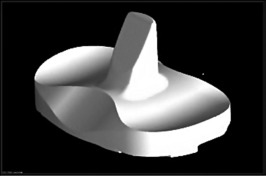
Many Japanese patients have difficulty performing their daily activities involving high flexion after undergoing total knee arthroplasty (TKA). In the last decade, many manufacturers have developed new designs of TKA implants that allow high knee flexion in patients postoperatively. These TKA implant designs ensure that Japanese patients' perform their daily activities and prayers satisfactorily. Genesis II Posterior Stabilized System (Smith & Nephew Inc., Memphis, TN, USA) with the high-flex insert (Fig. 6 ) is one of the TKA implants that permit high flexion motion of up to 155°.2
|
|
|
Fig. 6. The high-flex insert of the Genesis II, a total knee arthroplasty (TKA) implant permitting high flexion motion of up to 155°. |
We started using the Genesis II TKA implant with the high-flex insert since its introduction in Japan in 2004, because we thought that this high-flexion TKA system would be beneficial for all Japanese patients.
We investigated the benefits of using the Genesis II and the high-flex insert in Japanese patients at the mid-term follow-up after TKA.
Patients and methods
Written informed consent was obtained from all study patients; the study design was approved by the Institutional Ethics Review Board. Between June 2004 and June 2008, we prospectively evaluated 109 knees (73 patients; 12 men and 61 women) of patients who had undergone primary TKA. We followed-up 53 patients (8 men and 45 women) with 81 knees for >5 years. Twenty-eight patients had bilateral knee implants; 25 had unilateral knee implants. The other side of the knee had no severe pain and deformity in patients who underwent unilateral knee implants. Seven patients died; 10 were unable to visit our outpatient clinic due to complications, including dementia, cancer, spinal disease, and institutionalization. Two patients were excluded because they required implant revision due to late periarticular infection. The mean age at the primary operation was 71.4 years (57–93 years), mean body weight was 60.0 kg (41–102 kg), and mean body mass index was 25.9 kg/m2 (18.7–40.8 kg/m2 ). Osteoarthritis (OA) was diagnosed in 76 patients and osteonecrosis (ON) in 5 patients. The mean duration of postoperative follow-up was 6 years and 4 months (5–9 years) (Table 1 ).
| No. of patients | 54 |
| No. of total knee arthroplasties | 81 |
| Sex (Male/Female) | (9/45) |
| Mean age at the time of operation (years) | 71.4 (57–93) |
| Mean body weight (kg) | 60.0 (41–102) |
| Mean body mass index (kg/m2 ) | 25.9 (18.7–40.8) |
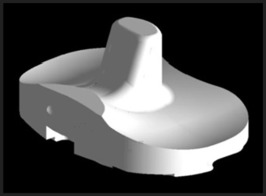
The Genesis II posterior stabilized knee prosthesis (Smith & Nephew Inc., Memphis, TN, USA) and the high-flex insert was used in all patients. This high-flexion system was designed so that the conventional insert was changed to the insert design without changing the femoral implant design, which permitted high knee flexion up to 155°. The Genesis II with the high-flex insert (Fig. 7 ) was designed to be safe during high flexion compared to the conventional insert (Fig. 8 ) because the anterior insert and post are chamfered. These chamfers relieve tension on the patellar tendon, allowing a more natural angle of the patella to facilitate deeper flexion while reducing the potential for anterior knee pain during high flexion and reducing fatigue stress to the post. The modified posterior articulation lowers the posterior lip of the insert, reducing contact stress while avoiding edge loading in deep flexion, which maintains the collateral ligament tension in deep flexion and moves the flexion contact point anteriorly and distally from the proximal edge of the posterior condyles. All patellae were replaced with the Biconvex inset patella (Smith & Nephew Inc.). The first author (single surgeon) performed all the TKA procedures. A straight mid-line incision was made; the parapatellar approach or mid-vastus approach was used. Osteotomies were performed using the measured resection technique. The extension gap was approximately equal, but the flexion gap was a trapezoidal space because of the built-in external rotation of the femoral component. Osteophytes at the posterior condyle were completely resected. All implants were cemented simultaneously; while closing the arthrotomy site and skin, all knees were deeply flexed as much as possible.
|
|
|
Fig. 7. The high-flex insert of the Genesis II. |
|
|
|
Fig. 8. The conventional insert of the Genesis II. |
Follow-up was performed by the first author. The range of motion (ROM), Japanese Orthopedic Association osteoarthritis knee rating score3 (JOA knee score) and radiological findings were evaluated. Additionally, all patients were asked about their lifestyle changes before and after the operation every year during the outpatient clinic visits.
The ROM, especially the maximum passive extension and flexion, was assessed using a goniometer (Tsutsumi Co., Ltd., Chiba Prefecture, Japan) with the patients' arms aligned along the axes of the femur and tibia on the lateral side of their knee joints.
Preoperative and postoperative clinical evaluations were performed using the JOA knee score. Pain during walking, pain while ascending and descending the stairs, ROM, and joint effusion were rated for patients with OA and ON with maximum scores of 30, 25, 35, and 10 points, respectively. Radiographic evaluations were obtained from the electronic medical record using the rating score from the Knee Society criteria.4
The following questions were asked to assess changes in the patients' Japanese lifestyle, and these questions were selected because of the typical movement of high flexion knee motion, which is necessary in the traditional Japanese lifestyle: 1) Do you enjoy sitting in seiza?, 2) Do you enjoy sitting in a cross-legged position or with your leg doubled back to one side?, 3) Do you use a Japanese style toilet?, 4) Do you eat meals on the floor at a low table?, 5) Do you sleep on a futon?, 6) Do you ride a bicycle?, and 7) Do you enjoy gardening?
Mann–Whitneys U-test was used to compare the preoperative and postoperative JOA knee scores and ROM as well as to compare the clinical data between patients who underwent bilateral TKA and those who underwent unilateral TKA. The number of preoperative and postoperative lifestyle changes was compared using a 2 × 2 chi-square test. P < 0.05 was considered statistically significant. For all statistical analyses, Microsoft Excel (Microsoft Corp., Redmond, WA, USA) was used.
Results
Preoperative extension ROM (mean, −13.8° [−30.0]) compared to postoperative ROM (mean, −0.5° [−5.0]) was significantly improved; the preoperative flexion ROM (mean, 112.4° [20.155]) compared to the postoperative ROM (123.4° [85.155]) was also significantly improved (Table 2 ).
| Preoperation | Postoperation | p value | |
|---|---|---|---|
| Mean extension angle | mean −13.8 (−30–0) | mean −0.5 (−5–0) | p < 0.05 |
| Mean flexion angle | mean 112.4 (20–155) | mean 123.4 (85–155) | p < 0.05 |
| Mean Japanese Orthopedic Association score | Mean 52.8 (25–80) | Mean 84.6 (60–95) | p < 0.05 |
| Seiza | 9% (5) | 3.7% (2) | p = 0.24 |
| Agura or Yokosuwari | 39% (21) | 30% (16) | p = 0.31 |
| Low table | 20% (11) | 11% (6) | p = 0.18 |
| Futon | 30% (16) | 22% (12) | p = 0.31 |
| Cycling | 48% (26) | 31% (17) | p = 0.07 |
| Japanese toilet | 20% (11) | 22% (12) | p = 0.81 |
| Gardening | 39% (21) | 43% (23) | p = 0.70 |
The radiographic alignment using the Knee Society criteria and the femoro-tibial angle (FTA) are shown in Table 2 . With regard to the JOA knee score, there was a significant improvement preoperatively (mean, 52.8 [25.80]) to postoperatively (mean, 84.6 [60.95]).
From the results of the questionnaires about the Japanese lifestyle changes, the percentage of patients who could sit in seiza reduced from 9% (5 patients) preoperatively to 3.7% (2 patients) postoperatively. The percentage of patients who could sit in agura or yokosuwari reduced from 39% (21 patients) preoperatively to 30% (16 patients) postoperatively. All patients used a Western style toilet at their residence, but the percentage of patients who could use a Japanese style toilet outside their residence increased from 20% (11 patients) preoperatively to 22% (12 patients) postoperatively. The percentage of patients who could eat at a low table reduced from 20% (11 patients) preoperatively to 11% (6 patients) postoperatively. Conversely, the percentage of patients using a Western style table while eating increased from 80% (43 patients) preoperatively to 89% (48 patients) postoperatively. The number of patients who usually slept on a futon reduced from 30% (16 patients) preoperatively to 22% (12 patients) postoperatively. Conversely, the percentage of patients who usually slept on the bed increased from 70% (38 patients) preoperatively to 78% (42 patients) postoperatively. The percentage of patients who could ride a bicycle reduced from 48% (26 patients) preoperatively to 31% (17 patients) postoperatively. Lastly, the percentage of patients who enjoyed gardening increased slightly from 39% (21 patients) preoperatively to 43% (23 patients) postoperatively (Table 3 ).
| Mean α angle | 94.4 ± 3.0 |
| Mean β angle | 89.3 ± 2.5 |
| Mean γ angle | 0.5 ± 4.3 |
| Mean δ angle | 87.3 ± 2.5 |
| Preoperative femur-tibia angle (FTA) | 183.8 ± 8.2 |
| Postoperative FTA | 175.8 ± 7.4 |
Among patients who underwent bilateral TKA or unilateral TKA, no significant differences were found in age, BMI, or follow-up duration. Additionally, preoperative and postoperative ROM, JOA score, and changes in the Japanese lifestyle had no significant difference between patients who underwent bilateral TKA and those who underwent unilateral TKA (Table 4 ).
| Unilateral | Bilateral | p-value | |
|---|---|---|---|
| Age (years) | 72 ± 7 | 73 ± 6 | 0.197 |
| BMI (kg/m2 ) | 27 ± 4 | 26 ± 4 | 0.336 |
| Preoperative JOA | 54 ± 11 | 52 ± 11 | 0.341 |
| Postoperative JOA | 85 ± 9 | 83 ± 11 | 0.197 |
| Preoperative extension | −12 ± 11° | −14 ± 9° | 0.456 |
| Postoperative extension | −1 ± 5° | 0 ± 1° | 0.805 |
| Preoperative flexion | 114 ± 21° | 112 ± 27° | 0.612 |
| Postoperative flexion | 123 ± 25° | 123 ± 17° | 0.917 |
| Duration (month) | 59 ± 24 | 63 ± 24 | 0.432 |
No revision surgeries were performed due to post-fracture or wear of the insert because of their Japanese lifestyle.
Discussion
In this study, we evaluated the clinical results of the high-flexion TKA system Genesis II TKA implant with a high-flex insert and its effect on the Japanese lifestyle.
Laskin reported on the clinical results of the Genesis II and the high-flex insert compared to the conventional insert.2 For the conventional insert group, the preoperative mean flexion range did not change significantly postoperatively. However, for the high-flex insert group, the preoperative mean flexion range changed remarkably from 117° to 133° postoperatively. In our study, we used the high-flex insert in all cases; therefore, we could not compare the results between the high-flex insert and the conventional insert. We treated many patients with a highly limited flexion knee range; therefore, the preoperative mean flexion range was 112° (lower than that in Laskins study). However, the postoperative flexion range remarkably improved to 123°. Laskin reported on the number of patients who could flex their knee >125° (21 knees preoperatively and 19 knees postoperatively in the conventional insert group). In the high-flex insert group, the number of knees that could flex >125° included 24 knees preoperatively and 36 knees postoperatively. Additionally, in our study, the number of knees that could flex >125° increased (30 knees preoperatively and 47 knees postoperatively).
Asano et al showed the range of motion of the knee in the traditional Japanese lifestyle after TKA. An appropriate flexion range is needed during floor-related activities in some postures after bi-surface knee TKA. They reported a 150 ± 5° of flexion for seiza, 132 ± 11° for the leg doubled back to one side, and 120 ± 11° for the cross-legged position.1 In our study, 148 ± 11° of flexion was needed for seiza, 138 ± 11° for the leg doubled back to one side, and 138 ± 11° for the cross-legged position. Our findings were similar to those of Asano et al.’s study for seiza and the leg doubled back to one side, but the flexion range for the cross-legged position was different. We surmise that the implant design influenced the differences in ROM for the posture in the cross-legged positions.
However, the mean JOA knee score improved from 52.8 to 84.6 postoperatively; the mean flexion range improved from 112.4° to 123.4° postoperatively; and the number of patients who enjoyed floor life in seiza, cross-legged, or leg doubled back to one side decreased from 39% to 30% postoperatively. Patients who enjoyed floor life before TKA but who gave up sitting on the floor after TKA complained of fear or discomfort in their knee after TKA. After they experienced the Western lifestyle (bed and table) during their hospital stay, they felt that the Western life style was more comfortable than the traditional Japanese lifestyle; therefore, they changed their lifestyle in their house after discharge. One patient gave up sitting on the floor because of decreased knee flexion range after TKA. Some patients had already changed their lifestyle from Japanese to Western style preoperatively, because they could not continue the traditional Japanese lifestyle with knee pain and the limited range of knee motion.
The bicycle is a very important vehicle for Japanese seniors, especially for patients who experience knee pain. They usually ride bicycles with a lower seat for safety; therefore, a high flexion knee motion is needed. The percentage of our patients who rode bicycles decreased from 45% to 27% postoperatively. Patients who gave up cycling postoperatively complained of fear of falling and experienced opposition from their family because of safety concerns. Thomsen et al. reported that even though they used high-flexion TKA designed implants, the increased flexion range of the knee after TKA did not reflect patient-derived parameters such as pain, satisfaction, and feel of the knee.5
Mechanoreceptors at the nerve endings were noted in the meniscus and the cruciate ligament.6 During the TKA operation, many nerve endings were sacrificed, resulting in a lack of proprioception at the knee joint after TKA. The patients' feeling of fear and discomfort after TKA while taking postures on the floor or while cycling were considered to be related to these neurological deficiencies. Although some TKA implants permitted high flexion, the kinematics between the normal and TKA implanted knees differed.7 This type of kinematic difference was also thought to be related to the patients fear and discomfort after implantation. Victor et al reported on the use of the Journey BCS TKA implant (Smith & Nephew Inc.), which has a more anatomical design than conventional TKA designs; in all patients, they confirmed a normal kinematic pattern of femoral rollback during flexion and axial rotation for 95% of the patients.8 As this type of implant has a more anatomical design and allows for normal kinematic movement, it was expected to decrease the patients' feelings of fear and discomfort.
The percentage of patients who enjoyed gardening was 41%; this number did not change after TKA.
TKA implants that allow for a high flexion knee motion also allow for an increased range of motion, but some risks are suspected in high flexion knee motion after TKA. Mauerhan reported a risk of post-fracture in high-flexion knee motion for PS-type inserts.9 Pulosky suggested that polyethylene wear should increase after overload to the post in high-flexion knee motion.10 Currently, how TKA implants affect high-flexion knee motion in the long-term is unclear; thus, careful follow-up, especially for complications, is needed.
Fortunately, we have not experienced implant failure thus far and revision surgery after implantation of high-flexion TKA in the mid-term follow-up. Pre- and postoperatively, we recommend upper arm support to patients while standing from the floor to avoid more load on the operated knee.
This study has some limitations. First, the study was small and included only 53 patients. The mean age of all patients at the time of operation was 73 years, which is higher than the mean age in Laskins study (67.5 years)11 and in Bournes study (68 years).12 In our study, 36 patients were aged >75 years at the time of operation. Therefore, it was difficult to follow-up all patients who underwent primary TKA at the mid-term follow-up. Second, we only used a posterior-stabilized type of TKA implant; therefore, the results of a cruciate-retaining TKA and its effect on the Japanese lifestyle could not be determined.
Conclusions
The range of knee motion, JOA knee score, and radiographic findings significantly improved in patients who underwent TKA using the Genesis II with the high-flex insert. Although these results improved, patients who could sit on the floor decreased from 39% preoperatively to 30% after TKA because of feelings of fear and discomfort. The new TKA implant design can achieve near normal kinematics, and it may decrease patients' feelings of fear and discomfort about the traditional Japanese floor-sitting lifestyle.
References
- 1 T. Asano, H. Takagi, K. Takatsuka, S. Nakamura; TKA kinematics in deep knee flexion for Japanese floor life; J Jpn Knee Soc, 32 (2007), pp. 1–4
- 2 R.S. Laskin; The effect of a high-flex implant on postoperative flexion after primary total knee arthroplasty; Orthopedics, 30 (2007), pp. 86–88
- 3 The Japanese Orthopaedic Association; Japanese Knee Society: Assessment Criteria for Knee Diseases and Treatments; Kanehara, Tokyo (1994)
- 4 F.C. Ewald; The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system; Clin Orthop Relat Res, 248 (1989), pp. 9–12
- 5 M.G. Thomsen, H. Husted, K.S. Otte, G. Holm, A. Troelsen; Do patients care about higher flexion in total knee arthroplasty? A randomized, controlled, double-blinded trial; BMC Musculoskelet Disord, 14 (2012), p. 127
- 6 J.C. Kennedy, I.J. Alexander, K.C. Hayes; Nerve supply of the human knee and its functional importance; Am J Sports Med, 10 (1982), pp. 329–335
- 7 S.J. Incavo, B.D. Beynnon, C.C. Johnson, D.L. Churchill; Knee kinematics in genesis total knee arthroplasty. A comparison of different tibial designs with and without posterior cruciate substitution in cadaveric specimens; Am J Knee Surg, 10 (1997), pp. 209–215
- 8 J. Victor, J.K. Mueller, R.D. Komistek, A. Sharma, M.C. Nadaud, J. Bellemans; In vivo kinematics after a cruciate-substituting TKA; Clin Orthop Relat Res, 468 (2010), pp. 807–814
- 9 D.R. Mauerhan; Fracture of the polyethylene tibial post in a posterior cruciate-substituting total knee arthroplasty mimicking patellar clunk syndrome: a report of 5 cases; J Arthroplasty, 18 (2003), pp. 942–945
- 10 S.K. Puloski, R.W. McCalden, S.J. MacDonald, C.H. Rorabeck, R.B. Bourne; Tibial post wear in posterior stabilized total knee arthroplasty. An unrecognized source of polyethylene debris; J Bone Jt Surg Am, 83-A (2001), pp. 390–397
- 11 R.S. Laskin, J. Davis; Total knee replacement using the Genesis II prosthesis: a 5-year follow up study of the first 100 consecutive cases; Knee, 12 (2005), pp. 163–167
- 12 R.B. Bourne, R.W. McCalden, S.J. MacDonald, L. Mokete, J. Guerin; Influence of patient factors on TKA outcomes at 5 to 11 years followup; Clin Orthop Relat Res, 464 (2007), pp. 27–31
Document information
Published on 31/03/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?