Summary
Tracheoesophageal fistula (TEF) is a serious complication associated with impaired quality of life. However, a successful TEF closure is difficult owing to the high incidence of recurrence. We utilized a prefabricated deltopectoral (DP) flap for closure of a TEF that occurred after an extended total thyroidectomy. Prefabrication of the inner soft tissue lining the DP flap with a split skin graft was performed prior to surgical closure of a TEF. Esophageal and tracheal mucosa were sutured to the split thickness side and full thickness side of the prefabricated DP flap, respectively. A successful closure of the fistula was achieved with this procedure. Prefabricated DP flap is a useful procedure for the surgical treatment of TEF.
Keywords
deltopectoral flap;prefabricated;skin graft;total thyroidectomy;tracheoesophageal fistula
1. Introduction
Tracheoesophageal fistula (TEF) is a rare but life-threatening condition that promotes chronic aspiration, pneumonia, and tracheal stenosis.1 Causes of acquired TEF include ventilatory cuff injury, local infection, caustic or foreign body ingestion, penetrating or nonpenetrating trauma, tracheal or esophageal malignancy, and iatrogenic surgical injury. Although various surgical approaches have been described, a successful TEF closure remains difficult owing to the high incidence of recurrence.2 We utilized a prefabricated deltopectoral (DP) flap for closure of a TEF that occurred after an extended total thyroidectomy.
2. Case report
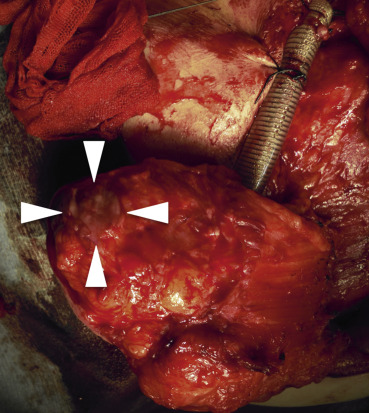
A 65-year-old female patient was diagnosed with thyroid papillary carcinoma T4aN0M1 invading the trachea. A total thyroidectomy with partial tracheal resection followed by creation of a tracheocutaneous fistula (TCF) was performed. However, leakage of saliva from the esophagus was observed after the surgery. Several procedures, including a direct closure and a pedicled myoperiosteal flap of the sternocleidomastoid muscle, were attempted to close the fistula. However, these procedures failed, resulting in a TEF measuring 1 cm in diameter at the left posterior wall of the trachea while the TCF still existed (Fig. 1). A two-stage operation was planned 92 days after the initial surgery.
|
|
|
Figure 1. Tracheoesophageal fistula on the posterior wall of the trachea was observed through the tracheocutaneous fistula. |
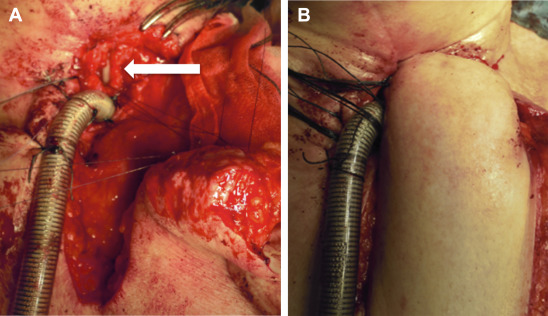
The distal part of the DP flap was first elevated. At the same time, a 5 × 4 cm split skin graft was taken from the patients left upper leg. Then the split skin graft was sutured to the inner soft tissue lining of the elevated DP flap using dissolvable sutures. The second procedure to close the TEF was performed 3–4 weeks later. First, an incision was made at the mucocutaneous junction along the unilateral edge of the TCF. The posterior wall of trachea was undermined and separated from the esophagus. When a severe scar formation prevented the tracheal wall from being undermined and separated from the esophagus, a circumferential excision of esophageal mucosa around the TEF including the dense scar tissue was performed. Subsequently, the prefabricated DP flap with well-healed skin graft was completely raised. The skin graft was de-epithelialized for a suitable size (Fig. 2). Esophageal mucosa was sutured around the split thickness side of the DP flap skin island to cover the esophageal defect (Fig. 3A). Tracheal mucosa was sutured to the full thickness side of the prefabricated DP flap to create a new TCF (Fig. 3B).
|
|
|
Figure 2. Prefabricated skin graft was de-epithelialized for 2.5 cm in diameter. |
|
|
|
Figure 3. (A) Esophageal mucosa was sutured around the split thickness side of the deltopectoral flap skin island to cover the esophageal defect. (B) Tracheal mucosa was sutured to the full thickness side of the prefabricated deltopectoral flap to create a new TCF. |
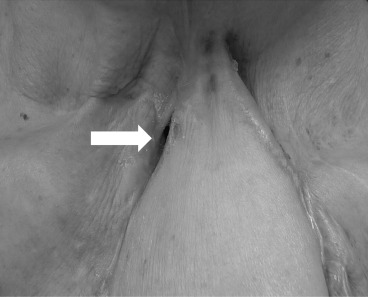
Videofluorography performed on the 36th day after the surgery did not demonstrate either leakage from the esophagus or laryngeal penetration, restoring the patients ability to ingest a normal oral diet. Furthermore, the suitable volume of the DP flap allowed the TCF to become slender like a slit, which allowed excellent and fluent speech to develop without covering the TCF with her finger (Fig. 4). Moreover, the patient reported that there was no severe inconvenience during speech or food intake. Finally, closure of the TCF was then completed.
|
|
|
Figure 4. The suitable volume of the deltopectoral flap allowed the tracheocutaneous fistula to become slender and slit-like. |
3. Discussion
The traditional surgical closure of a TEF includes fistula tract division and three-layer closure of the esophageal and tracheal linings with or without interposition of a pedicled regional skin or muscle flap.3 In this case, an alternative to the traditional procedure was required because of a dense scar formation around the TEF.
Although several free flaps including radial forearm flap and rectus abdominis flap and pedicled extracervical flaps including DP flap and pectoralis major myocutaneous flap have been reported to be useful for reconstruction of the pharynx and esophagus,4; 5; 6 ; 7 we chose a DP flap with modification for closure of a relatively small TEF in this case. The removal of dense scarring around the TEF caused a mucosal defect not only in the esophagus, but also in the trachea. Therefore, a two-sided epithelial coverage of the TEF was preferred to close the esophageal leak and to create a new TCF as well as to circumvent possible postoperative issues of re-epithelialization compromise.
The procedure of grafting split-thickness skin onto the soft tissue side to create a bilaminar cervical flap has mainly been used for full-thickness cheek reconstruction including oral mucosa and facial skin.8 The only report describing the closure of a TEF with skin-grafted bilaminar flap is a radial forearm free flap.9 The size of the TEF in the report was relatively large, at 2 × 4 cm; therefore, using a wide thin well-vascularized flap appeared to be optimal. The surgeons sutured the full thickness skin side of the flap to the esophageal mucosa, and the split thickness side to the tracheal mucosa. In the present case, we utilized the DP flap as a skin-grafted bilaminar flap. We sutured the full thickness skin side of the flap to the tracheal mucosa, and split thickness side to the esophageal mucosa.
The present procedure has several advantages. First, twisting the DP flap upside-down to put the skin side into the inner aspect of the esophagus is not required. Therefore, blood flow in the area is not affected by twisting. Second, a sufficient amount at the distal site of the DP flap is available not only to achieve closure of the esophagus, but also to create a new TCF. Thus, prefabrication of a DP flap using a split skin graft is a useful procedure for closure of TEFs. However, there exists an issue regarding cosmetic appearance when using this flap.
There is a report evaluating skin blood flow in the distal part of the DP flap by the Xenon-133 clearance rate.10 In that report, five types of delayed procedures for DP flap were analyzed. Group I was a “U-shaped, raised DP flap”, Group II was a “U-shaped, raised deltoid flap”, Group III was a “DP flap lined with a split-skin graft”, Group IV was a “Tubed, raised DP flap”, and Group V was a “Bipedicled, raised DP flap”. Interestingly, the recovery of the peripheral blood flow was fastest and greatest in Group III among those five groups. Group III was similar to the procedures performed in the present case. Therefore, the skin-grafted prefabrication of a DP flap also has the advantage of facilitating increased recovery of blood flow after the elevation of the flap.
In the present case, the prefabricated DP flap was a useful procedure for the surgical treatment of TEF. Two-sided eplithelialization has the advantage of allowing the simultaneous closure of both the esophageal and tracheal mucosa.
References
- 1 P. Dartevelle, P. Macchiarini; Management of acquired tracheoesophageal fistula; Chest Surg Clin N Am, 6 (1996), pp. 819–836
- 2 P. Macchiarini, J.P. Verhoye, A. Chapelier, E. Fadel, P. Dartevelle; Evaluation and outcome of different surgical techniques for postintubation tracheoesophageal fistulas; J Thorac Cardiovasc Surg, 119 (2000), pp. 268–276
- 3 A.A. Annyas, J.R. Escajadillo; Closure of tracheoesophageal fistula after removal of the voice prosthesis; Laryngoscope, 94 (1984), pp. 1244–1245
- 4 W. Muhlbauer, E. Herndl, W. Stock; The forearm flap; Plast Reconstr Surg, 70 (1982), pp. 336–344
- 5 M.L. Urken, J.B. Turk, H. Weinberg, C. Vickery, H.F. Biller; The rectus abdominis free flap in head and neck reconstruction; Arch Otolaryngol Head Neck Surg, 117 (1991), pp. 857–866
- 6 V.Y. Bakamijian; A two-stage method for pharyngoesophageal reconstruction with a primary pectoral skin flap; Plast Reconstr Surg, 36 (1965), pp. 173–182
- 7 S. Ariyan; The pectoralis major myocutaneous flap: a versatile flap for reconstruction in the head and neck; Plast Reconstr Surg, 63 (1979), pp. 73–81
- 8 N. Owens; A compound neck pedicle designed for the repair of massive facial defects: formation, development and application; Plast Reconstr Surg, 15 (1955), pp. 369–389
- 9 V.B. Wreesmann, L. Smeele, F.J.M. Hilgers, P.J.F.M. Lohuis; Closure of tracheoesophageal fistula with prefabricated revascularized bilaminar radial forearm free flap; Head Neck, 31 (2009), pp. 838–842
- 10 Y. Tsuchida, A. Tsuya, M. Uchida, S. Kamata; The delay phenomenon in types of deltopectoral flap studied by Xenon-133; Plast Reconstr Surg, 67 (1981), pp. 34–41
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?