Keywords
Chronic total occlusion;Percutaneous recanalization;Complications
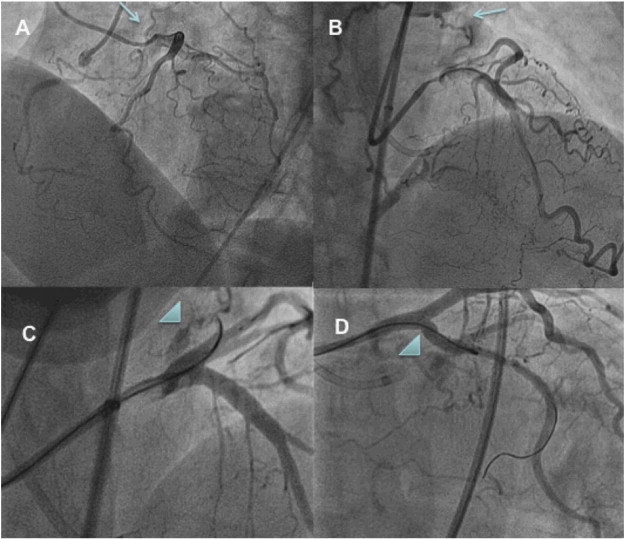
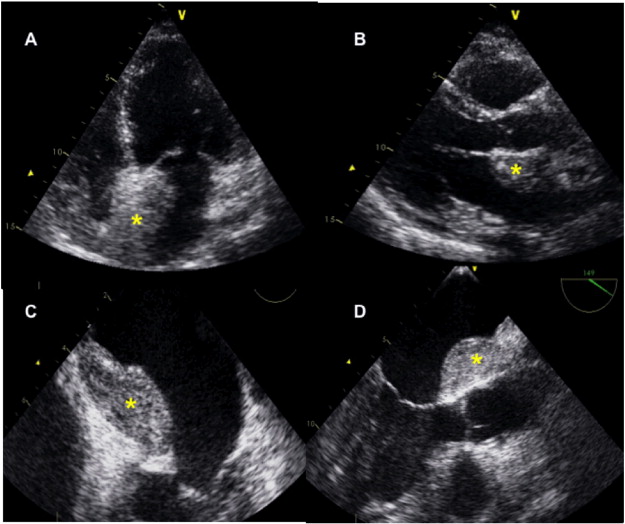
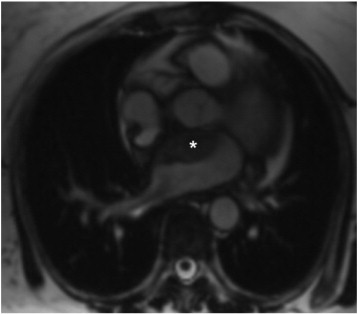
A 66 year-old female with previous history of diabetes mellitus was admitted to our institution due to a non-ST segment elevation myocardial infarction with inferior ischemic changes in the ECG. An echocardiogram performed upon arrival showed a non-dilated left ventricle (LV) with normal LV function. The patient was scheduled for a coronary angiogram that showed a patent left coronary artery and a complete occlusion of ostial right coronary artery (RCA). The RCA is opacified through collaterals from left coronary artery reaching the ostial stump. Collateral circulation is poor through septal connections but, notably, there is large albeit tortuous atrial collateral form left circumflex (LCX) connecting with the proximal RCA (Fig. 1, panels A and B). An attempt to recanalize RCA from an antegrade route failed due to the inability to cross the occlusion and place the wire in the true lumen. Subsequently, the patient was scheduled for a new attempt for recanalization of RCA via retrograde approach through the atrial collateral. The collateral could be wired with a Fielder XT coronary wire (Asahi Intecc Co., LTD) but the microcatheter (Corsair, Asahi Intecc Co., LTD) could not advance beyond the first significant bend of the artery. An angiographic control revealed thereafter a perforation of the collateral in its proximal segment with extravasation of contrast dye (Fig. 1, panels C and D). After excluding the presence of pericardial fluid the patient was given half dose of protamine, procedure was stopped and the patient was transferred to the coronary care unit. She remained asymptomatic and hemodynamically stable throughout the procedure. In the control echocardiogram performed two days after the procedure a hyperechoic mass could be seen in contact with left atrium (LA) (Fig. 2, panels A and B). Trasesophageal echocardiogram revealed that the mass was protruding in the LA and in close relationship with the interatrial septum and the left atrial appendage, but does not produce any interference with the mitral valve function or the drainage of the pulmonary veins (Fig. 2, panels C and D). Moreover, a small amount of pericardial fluid was observed as well as in the posterior LV wall (Fig. 2, panel B). With the suspicion of atrial hematoma following coronary collateral perforation a magnetic resonance imaging was performed. MRI confirmed the diagnosis of LA hematoma with extension to retroaortic fat (Fig. 3). The patient remained asymptomatic and she was managed conservatively.
|
|
|
Fig. 1. Panel A and B. Bilateral injection showing the atrial collateral channel connecting LCX with RCA (arrows). Panel C and D. Arrow-head shows the presence of contrast dye representing the collateral perforation. |
|
|
|
Fig. 2. Panels A and B. TTE image showing the presence of atrial hematoma in interatrial septum (asterisk). Panels C and D. TEE imaging showing the presence of LA hematoma (asterisk). |
|
|
|
Fig. 3. MRI showing atrial hematoma (asterisk) in contact with aortic root. |
LA hematomas are frequently related to complications of interventional cardiology procedures, either coronary or electrophysiological [1] ; [2]. Spontaneous hematomas may occasionally occur though are highly infrequent [3] ; [4]. Most of case patients remain asymptomatic but symptoms may develop as a consequence of functional alterations in mitral valve, pulmonary venous drainage or coexistence of pericardial fluid with hemodynamic instability and dyspnea. Diagnosis is usually performed by echocardiogram, CT scan or MRI. Differential diagnosis includes LA thrombus and intracardiac neoplasm. ([4] ; [5]). If symptoms develop, surgical drainage is mandatory but if the patient remains asymptomatic, conservative management and close clinical surveillance are adequate. ([4] ; [5]).
References
- [1] R. Sah, L.M. Epstein, R.Y. Kwong; Intramural atrial hematoma after catheter ablation for atrial tachyarrhythmias; Circulation, 115 (2007), pp. e446–e447
- [2] G.R. Barbeau, M. Senechal, P. Voisine; Delayed abrupt tamponade by isolated left atrial compression following coronary artery perforation during coronary angioplasty; Catheter Cardiovasc Interv, 66 (2005), pp. 562–565
- [3] a Lombardo, N. Luciani, V. Rizzello, L. Natale, F. Pennestri, R. Ricci, et al.; Spontaneous left atrial dissection and hematoma mimicking a cardiac tumor: findings from echocardiography, cardiac computed tomography, magnetic resonance imaging, and pathology; Circulation, 114 (2006), pp. e249–e250
- [4] Bautista-Hernández V, Velasco C, Fernández L, García-Monje MJ, Solla M, Bouzas B, Fojón S, Cuenca J. Spontaneous left atrial hematoma mimicking acute aortic síndrome. The utility of high resolution computed tomography. Circulation; 125:e1710-1712.
- [5] D. Tavano, M. Carlino, M. Pisani, A. Colombo; Conservative treatment of a left atrial hematoma and a localized tamponade occurring during treatment of coronary total occlusion; Circulation, 115 (2007), pp. e603–e606
Document information
Published on 19/05/17
Submitted on 19/05/17
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?