Summary
Ehlers–Danlos syndrome (EDS) is a group of well described connective tissue disorders in which collagen production is impaired. The surgical management of affected individuals remains challenging, with no general consensus. We report a case of spontaneous sigmoid perforation in a 17-year-old Eurasian male, in whom we subsequently established the diagnosis of EDS type IV (EDS-IV). We review the literature to discuss the clinical features and diagnosis, and the recommended therapeutic management.
Keywords
colectomy;COL3A1;Ehlers–Danlos syndrome type IV;sigmoid perforation;vascular
1. Introduction
Ehlers–Danlos syndrome (EDS) was first described by Edward Ehlers and was characterized by the triad of skin hyperelasticity, skin fragility and joint hypermobility by Henri-Alexandre Danlos.1 EDS patients exhibit a wide variety of features involving the skin and the vascular, gastrointestinal and uterine systems. Spontaneous gastrointestinal perforation is a particularly life-threatening complication.2 We describe a case of EDS type IV (EDS-IV) diagnosed in Singapore, and review the current literature on the diagnosis and management of EDS-IV.
2. Case report
A 17-year-old Eurasian male presented with acute peritonitis and high-grade fever. On examination he was tachycardiac but normotensive. There was lower abdominal tenderness and guarding. Total leukocyte count was elevated. A computed tomography (CT) scan of the abdomen and pelvis revealed small locules of extraluminal air and smooth peritoneal enhancement suggestive of perforation peritonitis.
At laparotomy, a 5-mm pinpoint sigmoid colonic perforation was found, with copious free intraperitoneal pus. The gastrointestinal tract and its mesentery were extremely friable. In view of the severe sepsis, metabolic acidosis and edematous bowel condition, the surgical decision was made to perform a sigmoid colectomy with end colostomy.
The patient’s recovery was complicated by left lung atelectasis secondary to mucus plugging, for which he underwent therapeutic bronchoscopy. A CT scan of the thorax showed a normal thoracic aorta with no root dilatation.
There was a past history of recurrent shoulder dislocations, and a spontaneous left pneumothorax that had been managed with thoracotomy and pleurodesis. The patient was noted to have the thin, translucent skin and facial dysmorphy characteristic of EDS-IV (see Table 1). There was no positive family history.
| Syndrome type | Inheritance | Major diagnostic criteria | Minor diagnostic criteria |
|---|---|---|---|
| Classic (type I and II) | Autosomal dominant | Skin hyperextensibility, wide atrophic scars, joint hypermobility | Smooth, velvety skin; easy bruising; molluscoid pseudotumors; subcutaneous spheroids; joint hypermobility; muscle hypotonia; postoperative complication (e.g., hernia); positive family history; manifestations of tissue fragility (e.g., hernia, prolapse) |
| Hypermobility (type II) | Autosomal dominant | Skin involvement (soft, smooth and velvety), joint hypermobility | Recurrent joint dislocation; chronic joint pain or limb pain, or both; positive family history |
| Vascular (type IV) | Autosomal dominant | Thin, translucent skin; arterial/ intestinal fragility or rupture; extensive bruising; characteristic facial appearance | Acrogeria, hypermobile small joints; tendon/muscle rupture; clubfoot; early–onset varicose veins; arteriovenous, carotid-cavernous sinus fistula; pneumothorax; gingival recession; positive family history; sudden death in close relative |
| Kyphoscoliosis (type VI) | Autosomal recessive | Joint laxity, severe hypotonia at birth, scoliosis, progressive scleral fragility or rupture of globe | Tissue fragility, easy bruising, arterial rupture, marfanoid, microcornea, osteopenia, positive family history |
| Arthrochalasia (type VII A & B) | Autosomal dominant | Congenital bilateral dislocated hips, severe joint hypermobility, recurrent subluxations | Skin hyperextensibility, tissue fragility with atrophic scars, muscle hypotonia, easy bruising, kyphoscoliosis, mild osteopenia |
| Dermatosparaxis (type VII C) | Autosomal recessive | Severe skin fragility; saggy, redundant skin | Soft, doughy skin; easy bruising; premature rupture of membranes; hernias (umbilical and inguinal) |
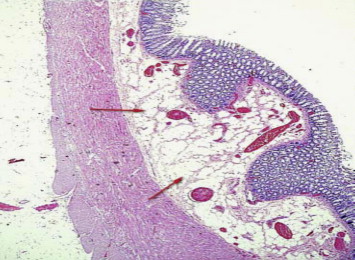
Histopathology of the resected sigmoid colon showed diffuse lipomatosis of the submucosa with focal discontinuation of muscularis mucosa at the site of perforation. There was disarray of smooth muscle fibers in the muscularis propria with associated neural hyperplasia (Figure 1). On the basis of the clinical findings with supporting histopathology and consultations with a genetic pediatrician colleague, we established a clinical diagnosis of EDS-IV in accordance with the Villefranche criteria.3
|
|
|
Figure 1. Histopathology of the resected sigmoid colon of a patient with Ehlers–Danlos syndrome type IV who experienced perforation of the colon; immunohistochemical stain (calretinin) under medium-power magnification. Note the pathological lipomatous hyperplasia (red arrows) of the submucosal layers. |
3. Discussion
The clinical spectrum of EDS is wide. The syndrome arises from inherited genetic mutations that disrupt collagen production.3 Of the six EDS subtypes, the vascular subtype (type IV) is the most serious. It reduces life expectancy, and 70% of sufferers present with vascular or gastrointestinal rupture; of these, 25% experience their first major complication by the age of 20 years.4
The Villefranche diagnostic criteria3 endorsed by the Ehlers–Danlos National Foundation (USA) and Ehlers–Danlos Support Group (UK) remains empirical to the characterization of EDS (Table 1).
However, given the heterogeneity of EDS-IV, surgeons are unlikely to encounter the condition except in the event of catastrophic arterial or gastrointestinal perforation. Multiple complications may ensue if the diagnosis goes unrecognized,5 hence there needs to be a high index of suspicion when a young adult presents with spontaneous colonic rupture in the absence of typical causes.6
A definitive diagnosis can be achieved by means of cultured dermal fibroblasts showing abnormalities of type III procollagen production, or molecular genetic testing of COL3A1.2 However, our patient declined these specialized tests because of financial concerns.
Although colonic perforation is well reported in EDS-IV, there remains a lack of consensus on its surgical management.7 This is compounded by the frequency with which complications related to tissue and vessel friability arise during or after surgery; these complications include recurrent gastrointestinal or arterial perforations, fistula formation, poor wound healing and wound dehiscence.8
Subtotal colectomy has been proposed as a reasonable treatment for spontaneous colonic perforations in EDS-IV.5 ; 7 To avoid future complications, the more radical approach of total abdominal colectomy (TAC) with end ileostomy, as opposed to primary resection and anastomosis with diversion, has been adopted for initial7 and repeated perforations.8 Re-establishing colonic continuity in EDS-IV, while anecdotally possible, is unwise in view of the high rate of reperforation.7 ; 9Surgeons must remain vigilant for repeat colonic ruptures, even in patients in whom the colon has been diverted; such ruptures typically occur proximal to a colostomy, with no accurate prediction offered by sentinel events.10
4. Conclusions
There remains a lack of consensus on the surgical management of spontaneous colonic rupture in EDS-IV patients. It is difficult to make a comparison between TAC with ileorectal anastomosis and end ileostomy without randomized, prospective studies. In this case, after counseling, our patient opted for a conservative approach with no further surgical intervention. Nevertheless, he will require lifelong follow-up. An holistic, multidisciplinary management regimen, including genetic counseling and family planning, is vital for such patients if they are to maintain an optimal quality of life.
References
- 1 P. Beighton; The Ehlers–Danlos syndrome; Heinemann Medical, London (1970)
- 2 D.P. Germain; Ehlers–Danlos syndrome type IV; Orphanet J Rare Dis, 2 (2007), p. 32
- 3 P. Beighton, A. De Paepe, B. Steinmann, et al.; Ehlers–Danlos syndromes: revised nosology, Villefranche, 1997. Ehlers–Danlos National Foundation (USA) and Ehlers–Danlos Support Group (UK); Am J Med Genet, 77 (1998), pp. 31–37
- 4 S.B. Maltz, R.J. Fantus, M.M. Mellett, et al.; Surgical complications of Ehlers–Danlos syndrome type IV: case report and review of the literature; J Trauma, 51 (2001), pp. 387–390
- 5 T. Berney, G. La Scala, D. Vettorel, et al.; Surgical pitfalls in a patient with type IV Ehlers–Danlos syndrome and pontaneous colonic rupture: report of a case; Dis Colon Rectum, 37 (1994), pp. 1038–1042
- 6 J.R. Fuchs, S.J. Fishman; Management of spontaneous colonic perforation in Ehlers–Danlos syndrome type IV; J Pediatr Surg, 39 (2004), pp. e1–e3
- 7 M. Pepin, U. Schwarze, A. Superti-Furga, P.H. Byers; Clinical and genetic features of Ehlers–Danlos syndrome type IV, the vascular type; N Engl J Med, 342 (2000), pp. 673–680
- 8 R.K. Freeman, J. Swegle, M.J. Sise; The surgical complications of Ehlers–Danlos syndrome; Am Surg, 62 (1996), pp. 869–873
- 9 P. Soucy, L. Eidus, F. Keeley; Perforation of the colon in a 15-year-old girl with Ehlers–Danlos syndrome type IV; J Pediatr Surg, 25 (1990), pp. 1180–1182
- 10 A.E. Stillman, R. Painter, D.W. Hollister; Ehlers–Danlos syndrome type IV: diagnosis and therapy of associated bowel perforation; Am J Gastroenterol, 86 (1991), pp. 360–362
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?