Abstract
Background
Outpatient cardiac rehabilitation (OP-CR) is a highly beneficial program but vastly under utilized.
Methods
The efficacy of a text-messaging program was analyzed to determine if implementation could improve number of OP-CR sessions completed. All patients enrolled in OP-CR from July 2011 through December 2012 were invited to join a text-messaging program on their first visit. The program required that the patient possesses a cell phone with texting capabilities. Participants received three to five text-messages per week offering heart-healthy tips and requests for body weight, minutes of exercise, blood pressure, and medication adherence. Patients enrolled (n = 52) in the texting program (Tx) were compared with those who were not (n = 185) (NTx) in several clinical indices and were compared using matched pairs (same subjects), comparison of means and frequencies, chi-square statistics, t-tests, and the Wilcoxon Rank Sum test.
Results
Significantly more patients in the Tx group completed the OP-CR program (61.5% versus 50%, p = 0.01). For those completing OP-CR, subjects in the Tx group completed significantly more sessions (31.4) than the NTx group (25.3) (p = 0.01). Additionally, significantly more in the Tx group were younger than those in the Ntx group.
Conclusions
Patients enrolled in OP-CR who participated in a text-messaging program were younger, attended significantly more sessions and were significantly more likely to complete the program.
Keywords
Cardiac rehabilitation;Short message service (SMS);Text-messaging
1. Introduction
Cardiovascular disease, of which coronary artery disease is the major form, is the most common cause of death in the United States [1] and worldwide [2]. The annual direct and indirect cost of cardiovascular disease and stroke in the United States is estimated to be $315.4 billion [3]. It is also the leading cause of loss of disability-adjusted life years worldwide [4].
Outpatient cardiac rehabilitation (OP-CR) is an evidence-based, cost-effective, multidisciplinary program of individual patient risk factor assessment and management, exercise training, and psychosocial support for patients with heart disease. The primary goals of OP-CR include reduction of modifiable risk factors as well as increasing functional capacity and quality of life. Outpatient CR is recommended by the American Heart Association (AHA) and the American College of Cardiology Guidelines for a number of diagnoses including myocardial infarction (MI), percutaneous coronary intervention (PCI), and coronary artery bypass surgery (CABG) [5]; [6]; [7]; [8]; [9] ; [10]. In 2014, OP-CR services were approved for patients with systolic HF by the Center for Medicare and Medicaid Services [11]. Among the numerous benefits, evidence has demonstrated that OP-CR reduces mortality by 12% to 34% [5]; [6]; [7]; [9] ; [10].
While the benefits of OP-CR are well documented, certain challenges remain. Outpatient-CR is underutilized with estimates of eligible patients participating ranging from 14–31% [12] to 80.7% for patients with myocardial infarction [13]. Barriers to participation are numerous and include factors such as a patients difficulty in attending OP-CR sessions [14]. Long-term adherence to risk factor modification and a healthier lifestyle for those participating in OP-CR is also a challenge for a significant number of patients. Conversely, it is well documented that patients who complete more OP-CR sessions have better outcomes compared to those who complete fewer sessions [15]. This finding highlights the importance of continued communication and engagement with participating patients. Given the present OP-CR model struggles with certain issues including attendance and long-term compliance, consideration of a paradigm shift aimed at improving outcomes seems warranted. In fact, a recent AHA Presidential Advisory called for a reengineering of OP-CR to enhance access, adherence, and effectiveness [16]. The current study assesses the ability of mobile technology to improve compliance with healthy lifestyle behaviors in patients participating in OP-CR.
2. Methods
2.1. Participants
The current study is a retrospective analysis on all patients enrolled in the OP-CR at the University of Iowa from July 12, 2011 through December 31, 2012 (n = 237) comparing those who voluntarily enrolled (n = 52) (Tx) to those who declined to enroll (n = 185) (NTx) in a text-messaging program on admission to OP-CR. The Tx program required that participants have a cell phone with texting capabilities. The majority of patients were referred to the OP-CR program from the inpatient CR program at the University of Iowa, having been hospitalized prior to referral. The inpatient CR staff obtained physician referrals for all eligible patients.
Informed consent was obtained for each patient to participate in OP-CR, as well as those participating in the Tx program. Concerning informed consent for this study, the University of Iowa Institutional Review Board (IRB) determined that IRB review was not required, because the analysis of data from the de-identified JMP (version 8 SAS® Institute) database, into which all the data for this study were entered and later data transferred to Excel for analysis, does not meet the regulatory definition of research involving human subjects.
2.2. Testing, assessments, training, education
On the first session in OP-CR, all patients were evaluated individually with a diagnostic quality electrocardiographic (ECG) exercise test from which the exercise prescription was developed. All patients were administered the Patient Health Questionnaire (PHQ9) [17] assessments. All tests were repeated on the final session of OP-CR as well as at three-month follow-up. All patients were weighed on each visit with height checked on the first visit in order to determine the body mass index (BMI). All patients had lipids evaluated four to six weeks post event and as ordered throughout the OP-CR program. Patients were encouraged to complete 36 sessions. Indigent patients on a special state program were allowed only six sessions. All participants met with the registered dietitian and stress management counselor and were strongly encouraged to attend all patient education classes, offered before or after their exercise sessions, including stress management, dietary modification, medication and other treatment modalities, and pathophysiology of heart disease.
2.3. Text messaging program
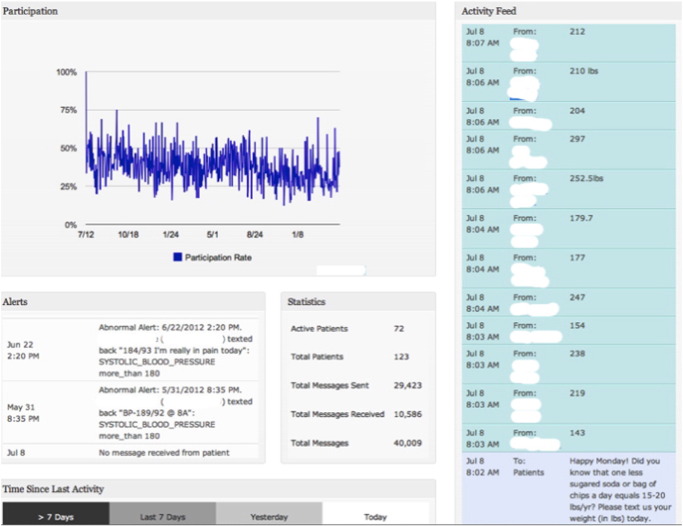
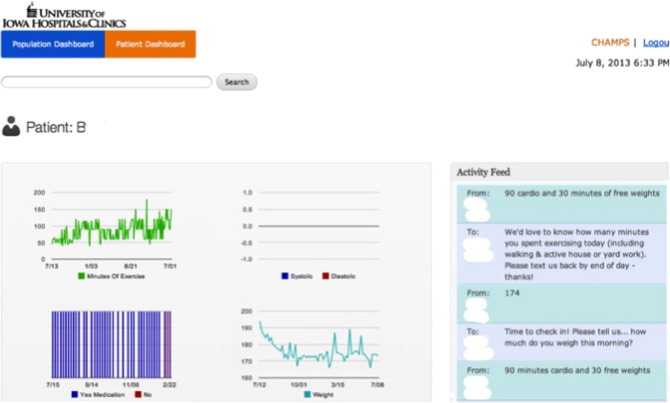
Text messages were sent three to five times per week and consisted of heart-healthy tips, requests for weight and BP input, minutes of exercise per day, and medication adherence. Participant responses were graphed and staff was notified of abnormal BP measurements and/or when a participant had not responded for 30 days. Fig. 1 illustrates data the OP-CR staff could observe online when logged in to the HealthCrowd site, which was password-protected. While messages are sent by the vendor, any staff member can interact with all patients or with individual patients as desired. Staff members of the OP-CR program were able to access the site as often as desired; at least one staff member did so at least twice per day. Individual patient data was accessible with name selecting his/her name (Fig. 2).
|
|
|
Fig. 1. Example of what the cardiac rehabilitation staff visualizes after logging in to HealthCrowd site. Top graph, left illustrates participation rate. “Alerts” (lower left) illustrates abnormal BP and notifications of patients who have not responded. “Statistics” (lower center) illustrates total messages sent to date, number of patients and number of messages received. The “Activity Feed” illustrates messages sent (lower right) and participants who have responded to the statement sent to all patients, “Happy Monday! Did you know that one less sugared soda or bag of chips a day equals 15–20 lbs/year? Please text us your weight (in lbs) today.” The responses for each patient are then graphed. |
|
|
|
Fig. 2. Example of an individual patient. In the top left graph, every time patient had entered minutes of exercise, it was graphed. The graph of blood pressure (BP) is not populated because the patient does not have a home BP unit. The lower left graph indicates that medications were taken (blue). In the second-to-last bar, which is red, indicates he did not take his medications. Text messages indicate that he had forgotten, but after being reminded, he took his medication. The lower right graph indicates his weight. The spikes in weight indicate when he was traveling and was the measures were questionable. In the text at right, messages to and from the patient are indicated. |
2.4. Statistical methods
Data from the two groups (Tx and NTx) were presented and compared in several ways. Categorical variables were presented as a number and percent of subjects and were compared using chi-square statistics. Continuous variables were displayed as mean, standard deviation, minimum and maximum. Normally distributed variables were compared using t-tests. Continuous variables that were not normally distributed were compared using the Wilcoxon Rank Sum test. The following were assessed: 1) gender, 2) age, 3) diagnoses, 4) days post event, 5) presence of diabetes mellitus (DM), 6) smoking status, 7) number of sessions completed, 8) whether or not the OP-CR program was completed, 9) risk stratification, 10) complications during exercise sessions, 11) whether or not the patient was indigent, 12) functional capacity, 13) PHQ9 depression inventory, and 14) SF-36v2®. Microsoft® Excel® for Mac 2011 (version 14.4.8) was used for all comparisons. All statistical tests with a p-value < 0.05 were considered significant.
3. Results
3.1. Significant differences
There were significant differences between the two groups in the following three categories:
- Age. The proportion of younger (< 70 years) subjects differed significantly between the two groups: 94.2% of the Tx group was < 70 years of age compared with 75.7% of the NTx group (p = 0.0033).
- Sessions completed. To assess the number of sessions completed by each group, the Wilcoxon Two-Sample Test was done; normal approximation (Z = 1.9219; two-sided Pr > [Z] = 0.0546). The number of sessions completed in the Tx group (mean: 20.9) trended toward statistical significance (p = 0.055) compared to the NTx group (mean 16.21). It is important to note that in the 17 months prior to this analysis, the mean number of sessions completed was 17.99 (n = 144) for all patients who completed the OP-CR program. For patients completing the program, see below.
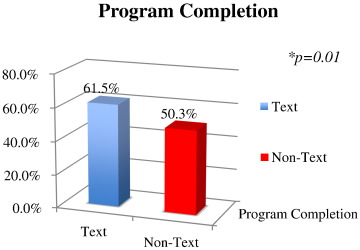
- Program completion. In the Tx group, 61.5% of patients completed the program, which was significantly more (p = 0.01) than the 50.27% in the NTx group who completed the program (Fig. 3). It is important to note that in the 17 months prior to the study only 46.5% of patients completed the program. For those patients < 70 years of age, only 44.9% completed the program in the 17 months prior to the study. Moreover, of those who completed the OP-CR program, as opposed to patients who quit the program, patients in the Tx group completed significantly more sessions (mean = 31.4) compared to the NTx (25.3) group (p = 0.01).
|
|
|
Fig. 3. Program completion. Significantly more patients in the texting program (61.54%) than non-texting (50.27%) completed the program. It should be noted that in the 17 months prior to the study, only 46.5% of all patients completed the program. For patients < 70 years of age, only 44.9% completed the program. |
The increase in number of sessions resulted in increased revenue and the return on investment was favorable at approximately 6:1 (Tx generated $108,680 in net income compared with NTx at $84,240 per year. The cost of the program was approximately $4400 per year).
3.2. Non-significant differences
There were non-significant differences between the two groups in the following six categories:
- Gender. The proportions of females were significantly fewer in both groups: 26.9% of the Tx group and 29.2 of the NTx group. The difference between the two groups was not significant (p = 0.7496).
- Smokers. The rate of current smokers did not differ significantly between the two groups: 21.6% of the Tx group was current smokers compared with 25.0% of the NTx group (p = 0.6129).
- Diagnoses. Analysis of patients by diagnoses revealed no significant differences with any of the diagnoses (for all, degree of freedom = 1). For patients with a confirmed diagnosis of an MI (n = 83), 28.85% and 36.76% were in the Tx and NTx groups, respectively. This was not statistically significant (chi-square = 1.1162, p = 0.2907). Patients who underwent a PCI without MI or CABG (n = 111) did not differ in the Tx and NTx groups (44.23% vs. 47.57%; chi-square 0.1815, p = 0.6701). Patients who underwent CABG without MI or PCI (n = 40) did not differ in the Tx and NTx groups (13.46% vs. 17.84%; chi-square 0.5541, p = 0.4566). Those patients with a diagnosis of stable angina, without MI, PCI, or CABG (n = 29) did not differ in the Tx and NTx groups (17.31% vs. 10.81%; chi-square 1.5954, p = 0.2066).
- Return for follow-up: There was no difference in the percentage of patients who returned for follow-up evaluations in the two groups; only 11.54% of the Tx group and 9.73% of the NTx group returned for follow-up evaluations (Chi-Square: degree of freedom 1; 0.1459; p = 0.7025).
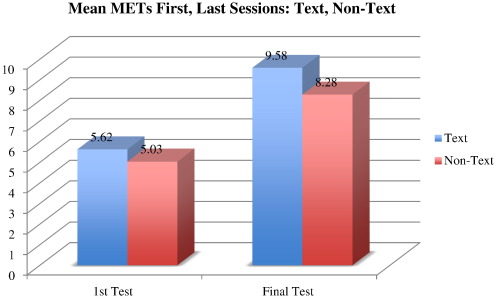
- Improvement in metabolic equivalent units (METs): Only patients who finish the OP-CR program undergo a final exercise test. Of those who completed the program, both the Tx and NTx groups had significant increases in peak METs. The Tx group increased from 5.62 METs (n = 52) to 9.58 METs (n = 30), a 70% increase. The NTx group increased from 5.03 METs (n = 184) to 8.28 (n = 92), a 65% increase in METs (Fig. 4).
|
|
|
Fig. 4. Mean METs achieved on the first and final sessions. Both Tx and NTx had significant increases in peak METs on first and final sessions (p = 0.0001). The Tx group increased 70%, from 5.62 METs (n = 52) to 9.58 METs (n = 30), whereas the NTx group increased 65%, from 5.03 (n = 184) to 8.28 METs (n = 92). Wilcoxon scores (rank sums) for variable METs were classified by variable, Tx. Average scores were used for ties. For the first test, normal approximation: Z 2.2889; two-sided Pr > [Z] 0.0221. METs for the final test: Z 1.8894; two-sided Pr > [Z] 0.0588. |
- Decrease in depression. The PHQ9 depression inventory indicated that both Tx and NTx had a significant decrease in scores, but there was not a significant difference between the Tx and NTx groups. Tx group (n = 51) on admission had a mean score of 6.57, while the NTx (n = 176) had a mean score of 7.12. On completion, Tx (n = 30) had a mean score of 3.3 while the NTx (n = 86) had a mean score of 3.09.
4. Discussion
The results of the present study indicate that the addition of text messaging program is cost-effective and significantly improves outcomes and compliance in conjunction with a traditional OP-CR program. Currently, little is known regarding the use of mobile applications to improve outcomes from and compliance with OP-CR [18]. Beatty, et al. [18] reviewed three published studies [19]; [20] ; [21] involving the use of mobile phone technology for the delivery of OP-CR. These studies evaluated health outcomes in patients with ischemia heart disease and supported the feasibility and acceptability of the use of mobile technology for patients in OP-CR [18]. They concluded that new strategies for promoting participation in OP-CR are necessary and that initial evidence supports the use of mobile technology for patients in OP-CR with ischemic heart disease [18].
Mobile technologies have the potential to overcome barriers associated with OP-CR, serving as a useful tool for increasing participation as well as long-term compliance [18] ; [22]. Mobile phones are the most commonly used form of technology worldwide and have the potential to influence large populations [23]. In many high-income countries, the number of mobile phone subscriptions outstrips the population [24]. In low-income countries, mobile communication is the fastest growing sector of the communication network and the coverage, geographically, is high [25]; [26]; [27] ; [28]. Moreover, in recent years, the world has experienced a significant expansion of internet availability and use, becoming a popular means of delivering interventions useful in health promotion as well as the treatment of non-communicable diseases [29]. The use of these technologies is able to influence health behaviors in real time [30] to a wide segment of the population [18] ; [31].
The impact of a mobile application on health outcomes must include participation in OP-CR sessions [32] ; [33], physical activity, exercise capacity, cardiovascular risk factors, patient-reported health status [18], and other factors. OP-CR is a mode of disease management and several studies have investigated the use of mobile technologies in disease management, but not specifically OP-CR. A meta-analysis of 59 trials investigating the use of mobile technologies to improve disease management and 26 trials that investigated the use of mobile technologies to change health behaviors found that text messaging interventions increased adherence to smoking cessation and antiretroviral therapy. All trials were conducted in high-income countries. Seventeen trials aimed to increase physical activity and/or reduce caloric intake [34]. Optimal treatment of chronic disease requires involvement of patients in managing their disease and their deciding whether to adhere to prescribed treatment and when to seek healthcare [35]. The mobile technologies are a means of providing this individualized support to patients to increase healthy behavior and improve disease management [34].
To our knowledge, no studies to date have been reported on the use of mobile technology exclusively for patients with coronary heart disease, which generally encompass an older population. Furthermore, no research has been published to date about mobile health interventions to promote medication adherence among acutely ill patients who were recruited from a hospital setting. The potential for mobile phone use in health care is currently being defined and remains a significant opportunity for research. We are not suggesting that mobile applications replace traditional OP-CR services. Rather, the impact of a mobile application on health outcomes enhances outcomes and compliance associated with participation in traditional OP-CR [18]; [32] ; [33].
5. Limitations
The current study was a retrospective analysis of a cohort undergoing standard clinical care. Thus, subjects were not randomized, creating a potential concern for self-selection bias. Future research is needed to examine the value of text messaging programs using a prospective, randomized design.
Moreover, this study did not examine the role that texting in OP-CR has on decreasing subsequent hospitalization due to improved disease management and risk factor modification. Following patients for longer periods will allow this assessment.
6. Conclusion
Patients who participate in a text-messaging program in OP-CR are younger, attend more sessions, and are more likely to complete OP-CR than patients who do not participate in texting.
Conflict of interest
There is no conflict of interest in this study.
Acknowledgements
Bern Shen, MD and Neng Bing Doh, MBA for their kind, generous, and unfailing help.
References
- [1] M. Heron; Deaths: leading causes for 2009; Natl Vital Stat Rep, 61 (2012), pp. 1–96
- [2] World Health Organization; The atlas of heart disease and stroke; http://www.who.int/int/cardiovascular_diseases/resources/atlas/en/ (2014)
- [3] A.S. Go, D. Mozaffarian, V.L. Roger, E.J. Benjamin, J.D. Berry, M.J. Blaha, et al.; Heart disease and stroke statistics — 2014 update: a report from the American Heart Association; Circulation, 129 (2014), pp. e28–e292
- [4] World Health Organization; Adherence to long-term therapies: evidence for action; http://www.who.int/chp/knowledge/publications/adherence_report/en/index.html (2003)
- [5] G.J. Balady, M.A. Williams, P.A. Ades, V. Bittner, P. Comoss, J.M. Foody, et al.; Core components of cardiac rehabilitation/secondary prevention programs: 2007 update; Circulation, 115 (2007), pp. 2675–2682
- [6] B.S. Heran, J.M. Chen, S. Ebrahim, T. Moxham, N. Oldridge, K. Rees, et al.; Exercise-based cardiac rehabilitation for coronary heart disease; Cochrane Database Syst Rev, 6 (7) (Jul. 2011), p. CD001800 https://doi.org/10.1002/14651858.CD001800.pub2
- [7] M.F. Piepoli, U. Corra, W. Benzer, B. Bjarnason-Wehrens, P. Dendale, D. Gaita, et al.; Secondary prevention through cardiac rehabilitation: from knowledge to implementation. A position paper from the Cardiac Rehabilitation Section of the European Association of Cardiovascular Prevention and Rehabilitation; Eur J Cardiovasc Prev Rehabil, 17 (1) (2010), pp. 1–17
- [8] S.C. Smith Jr., E.J. Benjamin, R.O. Bonow, L.T. Braun, M.A. Creager, B.A. Franklin, et al.; World Heart F, the Preventive Cardiovascular Nurses A. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation; Circulation, 124 (2011), pp. 2458–2473
- [9] R.S. Taylor, H. Dalal, K. Jolly, T. Moxham, A. Zawada; Home-based versus centre-based cardiac rehabilitation; Cochrane Database Syst Rev, 1 (2010), p. CD007130 https://doi.org/10.1002/14651858.CD007130.pub2
- [10] W.P. Wong, J. Feng, K.H. Pwee, J. Lim; A systematic review of economic evaluations of cardiac rehabilitation; BMC Health Serv Res, 12 (2012), p. 243
- [11] Centers for Medicare and Medicaid Services; Decision memo for cardiac rehabilitation; http://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=270 (2014)
- [12] J.A. Suaya, D.S. Shepard, S.L. Normand, P.A. Ades, J. Prottas, W.B. Stason; Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery; Circulation, 116 (15) (2007), pp. 1653–1662
- [13] A.L. Beatty, L. Shuang, T. Laine, E.A. Amsterdam, K.P. Alexander, M.A. Whooley; Trends in referral to cardiac rehabilitation after myocardial infarction: data from the National Cardiovascular Data Registry 2007–2012; J Am Coll Cardiol, 63 (23) (2014), pp. 2582–2583 https://doi.org/10.1016/j.jacc.2014.03.030
- [14] L. Jackson, J. Leclerc, Y. Erskine, W. Linden; Getting the most out of cardiac rehabilitation: a review of referral and adherence predictors; Heart, 91 (2005), pp. 10–14
- [15] P.A. Heidenreich, J.G. Trogdon, O.A. Khavjou, J. Butler, K. Dracup, M.D. Ezekowitz; Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association; Circulation, 123 (8) (2011), pp. 933–944
- [16] G.J. Balady, P.A. Ades, V.A. Bittner; American Heart Association Science A, Coordinating C. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association; Circulation, 124 (2011), pp. 2951–2960
- [17] K. Kroenke, R.L. Spitzer, J.B.W. Williams; The PHQ-9; J Gen Intern Med, 16 (9) (2001), pp. 606–613
- [18] A.L. Beatty, Y. Fukuoka, M.W. Whooley; Using mobile technology for cardiac rehabilitation: a review and framework for development and evaluation; J Am Heart Assoc, 2 (2013), p. e000568 https://doi.org/10.116/HAHA.113.000568
- [19] A. Blasco, M. Carmona, I. Fernandez-Lozano, M. Pascual, P.G. Sagredo, R. Somolinos, et al.; Evaluation of a telemedicine service for the secondary prevention of coronary artery disease; J Cardiopulm Rehabil Prev, 32 (2012), pp. 25–31
- [20] I. Korzeniowska-Kubacka, B. Dobraszkiewicz-Wasilewska, M. Bilinska, E. Rydzewska, R. Piotrowicz; Two models of early cardiac rehabilitation in male patients after myocardial infarction with preserved left ventricular function: comparison of standard out-patient versus hybrid training programmes; Kardiol Pol, 69 (2011), pp. 220–226
- [21] C. Worringham, A. Rojek, I. Stewart; Development and feasibility of a smartphone, ECG and GPS based system for remotely monitoring exercise in cardiac rehabilitation; PLoS One, 6 (2011), p. e14669
- [22] P. Lounsbury, E.E.I. Gordon, D. Gylten, J. Bunning; Text-messaging program improves outcomes in cardiovascular rehabilitation; Poster P266, World Congress of Cardiology, Dubai, April 18–21 (2012) [url: https://b-com.mci-group.com/EventPortal/Information/EventProgramme.aspx?EventInformationPageCode=POSTERPROGRAMME&EventCode=WCC2012]
- [23] International Telecommunication Union; The world in 2011: ICT facts and figures; http://www.itu.int/ITUD/ict/facts/2011/material/ICTFactsFigures2011.pdf (2011)
- [24] Ofcom; The consumer experience: telecoms, internet, and digital broadcasting 2009; Evaluation Report (2009)
- [25] K. Banks, R. Burge; Mobile phones: an appropriate tool for conservation and development?; (2004) [Cambridge, UK]
- [26] J. Donner; Research approaches to mobile use in the developing world: a review of the literature; Inf Soc, 24 (2008), pp. 140–159
- [27] V. Feldmann; Mobile overtakes fixed: implications for policy and regulation; ITU, Geneva (2003)
- [28] G. Sciadas, P. Guigue're, L. Adarn; From the digital divide to digital opportunities; Measuring infostates for development, Orbicom International Secretariat (2005)
- [29] K. Antypas, S.C. Wangberg; Combining users' needs with health behavior models in designing an internet- and mobile-based intervention for physical activity in cardiac rehabilitation; JMIR Res Protoc, 3 (1) (2014), p. e4 https://doi.org/10.2196/resprot.2725
- [30] W.T. Riley, D.E. Rivera, A.A. Atienza, W. Nilsen, S.M. Allison, R. Mermelstein; Health behavior models in the age of mobile interventions: are our theories up to the task?; Trans Behav Med, 1 (2011), pp. 53–71
- [31] A. Smith; Smartphone ownership 2013; Available from http://pewinternet.org/Reports/2013/Smartphone-Ownership-2013.aspx (Sep. 24 2013)
- [32] B.G. Hammill, L.H. Curtis, K.A. Schulman, D.J. Whellan; Relationship between cardiac rehabilitation and long-term risks of death and myocardial infarction among elderly Medicare beneficiaries; Circulation, 121 (2010), pp. 63–70
- [33] J.A. Suaya, W.B. Stason, P.A. Ades, S.T. Normand, D.S. Shepard; Cardiac rehabilitation and survival in older coronary patients; J Am Coll Cardiol, 54 (1) (2009), pp. 25–33
- [34] C. Free, G. Phillips, L. Galli; The effectiveness of mobile-health technology-based health behavior change or disease management interventions for health care consumers: a systematic review; PLoS Med, 10 (1) (2013), p. e1001362 https://doi.org/10.137/journal.pmed.1001362
- [35] L.K. Newby, N.M. LaPointe, A.Y. Chen, J.M. Kramer, B.G. Hammill, E.R. DeLong, et al.; Long-term adherence to evidence-based secondary prevention therapies in coronary artery disease; Circulation, 113 (2006), pp. 203–212
Document information
Published on 19/05/17
Submitted on 19/05/17
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?