Abstract
In this issue of the Biomedical Journal, we highlight a review revealing that the effect of autophagy, reactive oxygen species, and antioxidants in cancer may be a question of timing and context. We also discuss original research showing that the prevalence of cleft lip with or without palate in Taiwan has declined over the past 20 years, and what this might mean in terms of trends in abortion. Finally, we also learn about risk factors for recurrent hospital-acquired infection with multi-drug resistant bacteria, and the value of dental screening for patients with tinnitus.
Keywords
ROS; Antioxidants; Autophagy; Cancer; Cleft lip/palate; Prenatal diagnosis
Spotlight on reviews
The dual role of ROS, antioxidants and autophagy in cancer
Reactive oxygen species (ROS), including peroxides, superoxide and hydroxyl radicals, are a by-product of normal cell metabolism and important cell signaling molecules; yet, they are perhaps more infamously known for the role in ageing [1] and disease [2]. In excess, these molecules can cause irreversible damage to lipids, DNA and proteins. If ROS wreak havoc, cells can ‘clean up’ the mess they create through autophagy, in which damaged cellular components are degraded in lysosomes. Although these quality control pathways are generally thought to protect cells against the harmful effects of ROS, this view might not be so clear cut as explained by Hjelmeland and Zhang [3] in this issue of the Biomedical Journal.
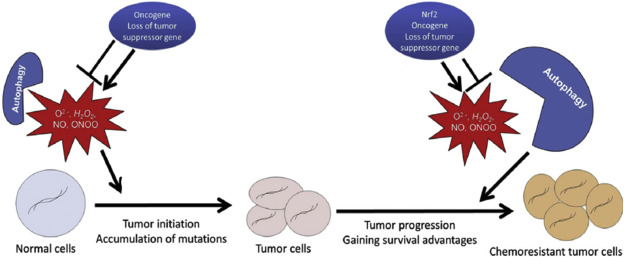
The link between ROS and cancer initiation is a long-standing one. Besides the high levels of ROS in obvious environmental carcinogens such as cigarette smoke [4], ROS have been shown to be critical for the transformation of cells mediated by oncogenes or loss of tumor suppressors. For example, the downregulation of p53 leads to increased ROS levels and antioxidant-related drugs inhibit tumor formation in mice lacking this gene [5]. However, every tumor is unique, and the role of ROS and antioxidants can differ depending on the genetic, epigenetic, and microenvironmental variation present. Indeed, mouse embryonic fibroblasts expressing mutant G12V K-Ras have low levels of ROS [6], and in another model, high levels of antioxidant production through mechanisms such as the upregulation of Nrf2 offers a survival advantage [7]. Thus, the notion that ROS are ‘bad’ and antioxidants are ‘good’ depends to some extent on context.
This lack of a simple dichotomy also applies somewhat to autophagy. The accumulation of damaged proteins or organelles leads to the generation of autophagosomes, which encapsulate the faulty cell contents and deliver them to lysosomes for degradation. This process involves over 30 proteins and many cellular signaling pathways [8], the perturbation of which leads to tumorigenesis [9]. This makes sense because autophagy suppresses chronic tissue damage and maintains genomic stability, but again the relationship is complex. For example, depending on cell context, autophagy may promote tumor growth by suppressing the p53 response, sustaining metabolic homeostasis and survival in stress and preventing the diversion of tumors to benign oncocytomas [10]. In light of these findings, autophagy inhibitors such as chloroquine have been tested in cancer therapy [11].
Thus, the effect of redox status and autophagy in cancer appears to be a question of context, and in particular, timing [[[#fig1|Fig. 1]]]. Although high levels of ROS and defects in autophagy promote cancer initiation, tumor cells with established genome mutations or rearrangements depend strongly on antioxidants and autophagy to gain survival advantages. How exactly to hit the tumor where it hurts will thus depend on complex phenotyping as part of the continuation of the quest to develop personalized treatments.
|
|
|
Fig. 1. Autophagy and ROS in tumor initiation and progression. In normal cells, the accumulation of ROS promotes tumor initiation. Autophagy removes ROS-damaged cellular components, thus protecting against tumorigenesis. However, in established tumor cells, the removal of these components by autophagy offers certain survival advantages and may lead to chemoresistance. Figure adapted from Hjelmeland et al. [3]. |
Spotlight on original articles
Drop in incidence of cleft lip/palate in Taiwan
Multiple factors have been linked to the development of cleft defects, including genetics, socio-economic status and in particular, environmental factors such as smoking, low folate consumption and drinking alcohol. While awareness about the dangers of smoking and drinking during pregnancy has increased over the years, so too has the use and accuracy of prenatal diagnosis by sonography [12]. In this issue of the Biomedical Journal, Chang et al. [13] report a drop in the incidence of cleft defects in Taiwan over the past 20 years, and suggest that this is due to an increase in the termination of fetuses with cleft defects.
Cleft lip and/or palate are the most common congenital craniofacial anomalies with an incidence of 1:700 to 1:1000 births depending on the population. These defects arise between the sixth and ninth week of pregnancy, when the tissues of the mouth and face are formed. Their treatment requires a multidisciplinary approach, involving surgery during the first sixth months of life, followed by subsequent surgical procedures and visits to a speech therapist, orthodontist, psychologist and specialist nurse.
Cleft lip was first diagnosed prenatally by sonography in 1981 [14]. Today, using 3D sonography, cleft lip with or without plate can be detected with an accuracy of 86–100% whereas a cleft palate alone remains difficult to diagnose before birth [15]. This improvement in technology has created a situation in which it is now possible in many countries to diagnose a cleft lip and terminate a pregnancy during the second trimester, all within the realm of the law. In Taiwan, abortion is legally permitted before 24 weeks of pregnancy if the fetus has severe congenital anomalies or causes detrimental effect to the mother. In 1995, following the establishment of National Health Insurance, prenatal sonography screening became readily available to Taiwanese women on a large scale for the first time.
To investigate the impact of widely available prenatal diagnosis, Jung et al. determined the rate of cleft defects in Taiwan between 1994 and 2013, during the introduction of National Health Insurance. They collected data from the two only Craniofacial centers in Taiwan where patients with clefts are referred. Out of nearly five million live births in Taiwan during the 20 year period, a total of 7282 new patients with cleft defects were identified. Linear regression revealed a significant decrease in the incidence of cleft lip with palate of 2.9% during the period, but there was a small increase in the incidence of cleft palate alone. Out of the 148 children treated for cleft lip with or without palate between 2009 and 2012, 73% had been diagnosed prenatally.
Although several factors may account for the decrease in cleft defects in Taiwan in recent years, a decrease specifically in the rate of cleft lip but not cleft palate alone suggests that prenatal diagnosis has played a prominent role. The aim of prenatal screening is not to increase the termination rate but to provide information to ensure the best care of both mother and fetus. Whether a prenatal diagnosis of cleft defect leads to termination largely depends on cultural factors and religion. A slowly declining trend in the incidence of cleft lip with or without palate and a stable incidence of cleft palate alone has been reported in other countries such as the Netherlands [16], where screening is carried out and abortion is permitted until the end of the second trimester. However, in a survey of Argentine parents of children with craniofacial clefts, none said that they would have terminated the pregnancy had they known about the condition, and half said that abortion should not be an option for any couple expecting a child [17].
In Taiwan, craniofacial defects are not well accepted and there is a relatively low stigma surrounding abortion. Yet, the decision to terminate a pregnancy second to a non-life threatening deformity is a complicated one, which is even reflected in the under-reporting of such terminations in some countries [18]. Technology in prenatal diagnosis is advancing. Now we must decide how to use it wisely.
Also in this issue:
News and perspectives
Road to a Nobel Prize
Chen [19] honors the awardees of the 2015 Nobel Prize in Physiology or Medicine by describing the route leading to the discovery of the anti-parasitic drugs avermectin and artemisinin, which have revolutionized treatment of roundworms and malaria, respectively.
Review article
Visualizing retinal diseases in real time
In this review, Murthy et al. [20] discuss advances in optical coherence tomography, a non-invasive imaging technique that uses light waves to take cross-sectional pictures of the retina, and describe how this technique has become indispensable in the diagnosis and management of retinal diseases.
Original articles
Anti-EGFR therapy in the face of resistance
Lung adenocarcinoma is a deadly disease with a poor prognosis. Some patients with particular mutations in the epidermal growth factor (EGFR) respond to anti-EGFR targeted therapies; however, most people eventually acquire resistance to these drugs [21]. If new lesions appear then treatment should be altered, yet the condition of some patients deteriorates rapidly after the withdrawal of anti-EGFR agents, despite acquired resistance [22]. In this retrospective study of 102 patients, Hsu et al. [23] find no clear benefit to discontinuing EGFR therapy following acquired resistance.
Diabetes is a risk factor for recurrent infection with multidrug resistant bacteria
Multidrug-resistant A. baumannii (MDR-AB) is becoming an increasing menace in hospital environments and is a frequent case of healthcare-associated infections [24]. In some patients, the infection comes back despite appearing to be clinically eradicated. To identify factors that might promote recurrent infections, Lin et al. [25] retrospectively analyzed 106 patients with pulmonary MDR-AB infection, and identify diabetes mellitus as a risk factor for relapse of infection.
Dental screening for tinnitus patients
Tinnitus is a ringing in the ears which is readily perceived by patients but cannot be objectively measured. In clinical practice, the condition is often associated with problems in the jaw or muscles of the face (temporomandibular disorders), suggesting that a dental exam should be an integral part of the care of tinnitus patients. Now, Di Berardino [26] et al. use T-scan III occlusal imaging to measure occlusal stability in individuals with or without tinnitus. Their findings suggest a useful diagnostic tool to determine whether patients with tinnitus should be referred to a dentist.
Optimal sedation approach for endoscopy technique in an outpatient setting
Endoscopic retrograde cholangiopancreatography (ERCP) is a specialized technique combing endoscopy and X-rays to diagnose and treat problems of the bile and pancreatic ducts. ERCP can be performed in an outpatient setting with different sedation techniques being applied in different centers. In this prospective clinical trial of 49 patients, Akhondzadeh et al. [27] compare combinations of anesthetics and analgesics among patients undergoing ERCP outside the operating room and found that propofol–ketamine was associated lower levels of pain and apnea than propofol–fentanyl.
Brief communication
Mucormycetes infection despite functioning immune system
Mucormycosis is a serious but rare fungal infection caused by molds called mucormycetes. It usually infects individuals with a weakened immune, but in this case report, Bhattacharya et al. [28] describe the unusual presentation of esophageal mucormycosis in an immunocompetent infant.
Letter to the editor
Challenges to increasing the use of contraceptives in Northern India
Roy [29] comments on an article by Deepti Choudhary et al. [30] in a recent issue of the Biomedical Journal in which the authors analyzed patterns of contraceptive behavior in Northern India. Roy asks Choudhary to elaborate on why some women who do not want any more children choose not use contraceptives despite knowledge of their existence. In her reply, Choudhary [31] lists several reasons, including inability to choose appropriate method, unavailability of methods, lack of knowledge about how to use them, and fear of side-effects.
References
- [1] T. Finkel, N.J. Holbrook; Oxidants, oxidative stress and the biology of ageing; Nature, 408 (2000), pp. 239–247
- [2] G. Waris, H. Ahsan; Reactive oxygen species: role in the development of cancer and various chronic conditions; J Carcinog, 5 (2006), p. 14
- [3] A. Hjelmeland, J. Zhang; Metabolic, autophagic, and mitophagic activities in cancer initiation and progression; Biomed J, 39 (2016), pp. 98–106
- [4] M.F. Huang, W.L. Lin, Y.C. Ma; A study of reactive oxygen species in mainstream cigarette smoke; Indoor Air, 15 (2005), pp. 135–140
- [5] A.A. Sablina, A.V. Budanov, G.V. Ilyinskaya, L.S. Agapova, J.E. Kravchenko, P.M. Chumakov; The antioxidant function of the p53 tumor suppressor; Nat Med, 11 (2005), pp. 1306–1313
- [6] G.M. DeNicola, F.A. Karreth, T.J. Humpton, A. Gopinathan, C. Wei, K. Frese, et al.; Oncogene-induced Nrf2 transcription promotes ROS detoxification and tumorigenesis; Nature, 475 (2011), pp. 106–109
- [7] M.B. Sporn, K.T. Liby; NRF2 and cancer: the good, the bad and the importance of context; Nat Rev Cancer, 12 (2012), pp. 564–571
- [8] Y. Feng, D. He, Z. Yao, D.J. Klionsky; The machinery of macroautophagy; Cell Res, 24 (2014), pp. 24–41
- [9] S. Lorin, A. Hamaï, M. Mehrpour, P. Codogno; Autophagy regulation and its role in cancer; Semin Cancer Biol, 23 (2013), pp. 361–379
- [10] J.Y. Guo, B. Xia, E. White; Autophagy-mediated tumor promotion; Cell, 155 (2013), pp. 1216–1219
- [11] N. Chen, V. Karantza; Autophagy as a therapeutic target in cancer; Cancer Biol Ther, 11 (2011), pp. 157–168
- [12] P. Paterson, H. Sher, F. Wylie, S. Wallace, A. Crawford, V. Sood, et al.; Cleft lip/palate: incidence of prenatal diagnosis in Glasgow, Scotland, and comparison with other centers in the United Kingdom; Cleft Palate Craniofac J, 48 (2011), pp. 608–613
- [13] W.J. Chang, L.C. See, L.J. Lo; Time trend of incidence rates of cleft lip/palate in Taiwan from 1994 to 2013; Biomed J, 39 (2016), pp. 150–154
- [14] J.E. Christ, M.G. Meininger; Ultrasound diagnosis of cleft lip and cleft palate before birth; Plast Reconstr Surg, 68 (1981), pp. 854–859
- [15] W. Maarse, S.J. Berge, L. Pistorius, T. van Barneveld, M. Kon, C. Breugem, et al.; Diagnostic accuracy of transabdominal ultrasound in detecting prenatal cleft lip and palate: a systematic review; Ultrasound Obstet Gynecol, 35 (2010), pp. 495–502
- [16] A.B. Mink van der Molen, W. Maarse, L. Pistorius, H.S. de Veye, C.C. Breugem; Prenatal screening for orofacial clefts in the Netherlands: a preliminary report on the impact of a national screening system; Cleft Palate Craniofac J, 48 (2011), pp. 183–189
- [17] D.F. Wyszynski, C. Perandones, R.D. Bennun; Attitudes toward prenatal diagnosis, termination of pregnancy, and reproduction by parents of children with nonsyndromic oral clefts in Argentina; Prenat Diagn, 23 (2003), pp. 722–727
- [18] http://www.telegraph.co.uk/news/health/news/9845780/Cleft-lip-abortions-10-times-as-common-as-reported.html [Last accessed on 06.05.16].
- [19] W.J. Chen; Honoring antiparasitics: the 2015 Nobel Prize in Physiology or Medicine; Biomed J, 39 (2016), pp. 93–97
- [20] R.K. Murthy, S. Haji, K. Sambhau, S. Grover, K.V. Chalam; Clinical applications of spectral domain optical coherence tomography in retinal diseases; Biomed J, 39 (2016), pp. 107–120
- [21] D. Jackman, W. Pao, G.J. Riely, J.A. Engelman, M.G. Kris, P.A. Jänne, et al.; Clinical definition of acquired resistance to epidermal growth factor receptor tyrosine kinase inhibitors in nonsmall- cell lung cancer; J Clin Oncol, 28 (2010), pp. 357–360
- [22] J.E. Chaft, G.R. Oxnard, C.S. Sima, M.G. Kris, V.A. Miller, G.J. Riely; Disease flare after tyrosine kinase inhibitor discontinuation in patients with EGFR-mutant lung cancer and acquired resistance to erlotinib or gefitinib: implications for clinical trial design; Clin Cancer Res, 17 (2011), pp. 6298–6303
- [23] P.C. Hsu, L.C. Chiu, S.H. Li, C.H. Chen, C.L. Wang, C.Y. Liu, et al.; Continuous epidermal growth factor receptor- tyrosine kinase inhibitor administration in primary lung adenocarcinoma patients harboring favorable mutations with controlled target lung tumors dose not hinder survival benefit despite small new lesions; Biomed J, 39 (2016), pp. 121–129
- [24] A. Howard, M. O'Donoghue, A. Feeney, R.D. Sleator; Acinetobacter baumannii: an emerging opportunistic pathogen; Virulence, 1 (2012), pp. 243–250
- [25] C.Y. Lin, Y.M. Chen, M.C. Lin, Y.P. Chang, T.Y. Chao, A.S. Lin, et al.; Risk factors of multidrug-resistant Acinetobacter baumannii recurrence after successful eradication in ventilated patients; Biomed J, 39 (2016), pp. 130–138
- [26] F. Di Berardino, E. Filipponi, M. Sciappadori, S. Forti, D. Zanetti, A. Cesarani; The occlusal imaging and analysis system by T-scan III in tinnitus patients; Biomed J, 39 (2016), pp. 139–144
- [27] R. Akhondzadeh, A. Ghomeishi, S. Nesioonpour, S. Nourizade; A comparison between the effects of propofolefentanyl with propofoleketamine for sedation in patients undergoing endoscopic retrograde cholangiopancreatography outside the operating room; Biomed J, 39 (2016), pp. 145–149
- [28] J.B. Bhattacharya, S. Kaushal, S.K. Aggarwal; Esophageal mucormycosis in an immunocompetent child: a rare presentation; Biomed J, 39 (2016), pp. 155–157
- [29] M.P. Roy; Contraceptive behaviour in North India; Biomed J, 39 (2016), p. 158
- [30] D. Choudhary, R. Pal, N. Goel; Awareness and practice patterns of family planning methods among antenatal women in Indian community: are we hitting the bulls eye?; Biomed J, 38 (2015), pp. 356–358
- [31] D. Choudhary; Meeting the unmet needs of family planning methods; Biomed J, 39 (2016), p. 159
Document information
Published on 20/10/16
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?