Summary
Intravesical Bacillus Calmette–Guérin (BCG) has been a proven and effective immunotherapy treatment for superficial transitional cell carcinoma (TCC) of the bladder, especially for high-grade tumors and carcinoma in situ. Nevertheless, significant side effects are associated with BCG instillations, including fever, myalgia, malaise, dysuria, hematuria, and irritable lower urinary tract symptoms. We herein report the case of a patient who developed Reiters syndrome following intravesical BCG instillations. A 39-year-old Chinese man presented with a 3-week history of dysuria, suprapubic pain, and pain at the tip of the penis postmicturition. Initial investigations revealed that he had microhematuria, and an ultrasound with computed tomography scan of the abdomen showed a bladder mass. Transurethral resection of the bladder tumor was performed and the patient received a single dose of intravesical mitomycin postoperatively. Results of histopathological examination revealed high-grade bladder TCC (G3pT1), and the patient was managed with intravesical BCG for 2 weeks following the surgery. Four weekly cycles of BCG were administered uneventfully; however, before the fifth instillation, the patient complained of urethral discharge, bilateral conjunctivitis, and low back pain. Reiters syndrome was diagnosed as a rare but known complication of BCG instillation and the BCG immunotherapy was withheld. The patient was treated with nonsteroidal antiinflammatory drugs (for back pain) and eye ointment (for conjunctivitis) and his condition improved. This case report of Reiters syndrome should be highlighted as a rare but significant complication of BCG immunotherapy and urologists should have a high index of suspicion to diagnose this rare complication.
Keywords
Bacillus Calmette–Guérin;intravesical;Reiters syndrome
1. Introduction
The classical triad of urethritis, conjunctivitis, and arthritis often prompts the clinician toward the diagnosis of Reiters syndrome. This syndrome is often described following urinary, respiratory, venereal, or gastrointestinal infections. However, in our patient, we diagnosed the syndrome following intravesical installations of Bacillus Calmette–Guérin (BCG) for superficial bladder transitional cell carcinoma (TCC). Fortunately, we recognized this uncommon syndrome and treated the patient with appropriate medications. We therefore recommend that clinicians should be highly vigilant and suspicious of Reiters syndrome following intravesical BCG immunotherapy in patients.
2. Case report
A 39-year-old Chinese mechanic presented with a 3-week history of painful micturition and microhematuria. The patient felt pain at the tip of the penis at the end of micturition and it lasted for a few minutes postmicturition; in addition, a vague pain was also felt at the suprapubic region when the bladder was full. The patient did not have any obvious urethral discharge nor any previous infections with sexually transmitted diseases (STDs). He was generally in good health with no significant comorbidities, but he was a smoker of 20 pack-years. The general and abdominal clinical examination results were unremarkable. Initial investigations confirmed microhematuria on urine microscopy and an abdominal ultrasound revealed a suspicious lesion at the dome of the bladder.
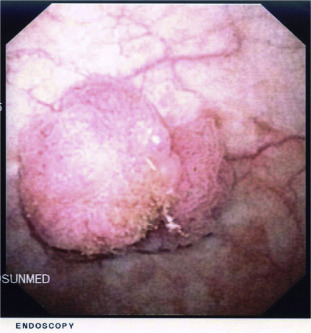
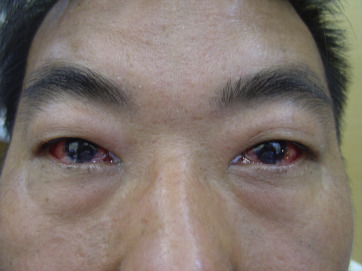
Abdominal computed tomography scan confirmed the bladder lesion with no extra vesical extension. A subsequent flexible cystoscopy showed a solid papillary lesion at the dome of the bladder (Fig. 1) and two smaller lesions in a background of inflamed urothelium (Fig. 2). The patient underwent transurethral resection of the bladder tumor with cystodiathermy, followed by postoperative installation of a single dose of mitomycin C in the recovery suite. The histopathological report confirmed high-grade 3 TCC of the bladder with no carcinoma in situ and no evidence of muscularis propria invasion. He made an uneventful recovery and 2 weeks later an intravesical course of BCG was initiated to reduce the risk of recurrence and progression of the bladder tumor. He received weekly intravesical installation of BCG (81 mg/week) and received 4 weeks of installation uneventfully. However, 2 days before the fifth instillation, the patient reported milky urethral discharge, bilateral red sore eyes, and low backache associated with asymmetrical arthralgias of the hands and feet. There were no preceding flu-like symptoms, lethargy, fever, or any gastrointestinal or urinary tract infections and he had no previous rheumatologic disorders. On examination, bilateral conjunctivitis was identified ( Fig. 3) and the patient had limited back movement due to pain. There were no stigmata of genital cutaneous lesions. Blood test results were largely unremarkable, urine culture did not reveal any bacterial growth, and urethral smear was negative. Routine tests for STD were negative. We suspected Reiters syndrome and BCG treatment was deferred. The patient was then referred to a rheumatologist and an ophthalmologist for their opinions, who confirmed the diagnosis as Reiters syndrome. The patient was treated symptomatically with nonsteroidal antiinflammatory drugs (NSAIDs) for the back pain and with chloramphenicol eye ointment for conjunctivitis. He was then closely monitored in order to initiate treatment with steroids and isoniazid if there was no spontaneous improvement. Fortunately, the conjunctivitis subsided after 8 days of treatment and his backache resolved after 3 weeks. We decided to stop further BCG treatment, and a subsequent cystoscopy check revealed only generalized inflammation with no signs of recurrence. The subsequent follow-up cystoscopies to detect recurrences were essentially normal. Once these aforementioned symptoms resolved, no recurrences of conjunctivitis, arthralgias, or any further urethral discharge was noted.
|
|
|
Figure 1. Cystoscopic view of bladder lesion. |
|
|
|
Figure 2. Cystoscopic view of the inflamed urothelium of the bladder. |
|
|
|
Figure 3. Bilateral conjunctivitis. |
3. Discussion
Reiters syndrome, which is also known as reactive arthritis, is the classic triad of conjunctivitis, urethritis, and arthritis occurring after an infection, particularly following an infection of the urogenital or gastrointestinal tract.1 Classically, this syndrome has been described following urinary, respiratory, venereal, or gastrointestinal infections. However, in our case, the patient developed the syndrome following intravesical BCG instillations for superficial bladder TCC. In a recent review of reactive arthritis following BCG immunotherapy, there have been a few case reports of Reiters syndrome following intravesical BCG immunotherapy.2
The infamous phrase of “can't see, can't pee, and can't climb a tree” often gets associated with this syndrome due to the corresponding symptoms of conjunctivitis, urethritis, and arthritis. In most cases this syndrome tends to affect adults, although children have also been reported to be affected. In general, the syndrome has a significant male preponderance and often occurs in the third decade of life.
The pathophysiology of this syndrome is largely thought to be due to immune and infectious components. Numerous organisms have been associated with the preceding cause of Reiters syndrome and its close association with HLA-B27 may lead to cross-reactivity, a situation in which the antibodies developed against these infections will also have the affinity for HLA-B27.1 Likewise, in the case of BCG immunotherapy-induced Reiters syndrome, both local and systemic immune mechanisms have been thought to induce the molecular mimicry mechanism of the disease.2
Clinical manifestations of Reiters syndrome can be quite variable and these include the urogenital, rheumatologic, ophthalmologic, dermatologic, and visceral systems. However, the classical triad of urethritis, conjunctivitis, and arthritis only occurs in about one third of patients.3 In our case, the patient presented with the classical triad of urethral discharge, conjunctivitis, and back pain, which helped us to diagnose the syndrome promptly. In fact, back pain has been noted to be present in 49% of the patients at the onset,4 whereas conjunctivitis was also reported as the most common eye symptom, observed in up to 60% of patients.5
Often the diagnosis of Reiters syndrome will be based on thorough medical history and systematic clinical examination, with a high index of suspicion when the triad of symptoms is noticed. There is no single confirmatory laboratory or radiological test that can confirm diagnosis. In addition, there are also differential diagnoses of gout, gonococcal urethritis, and psoriatic arthritis that must be excluded. In our patient, the syndrome was diagnosed based on multiple consultations with the ophthalmologist and rheumatologist.
Treatment of Reiters syndrome usually revolves around providing symptomatic relief and this includes bed rest, NSAIDs, and eye ointments. These general symptomatic measures often will provide the remission of symptoms. Occasionally, steroids with or without isoniazid or rifampicin may be started if the symptoms prolong or worsen. There is no consensus with regard to the use of antibiotics, especially in the usual cases preceded by infections, but in our patient, who developed Reiters syndrome following intravesical BCG instillations, no antibiotics were needed. In cases of BCG-induced Reiters syndrome, cessation of the intravesical BCG immunotherapy is perhaps the most important treatment together with medications aimed at symptomatic relief.
The prognosis of Reiters syndrome is variable, but most cases achieve spontaneous resolution of symptoms by a few weeks, and in rare cases may progress to chronic illness. Our patient has had no relapse of Reiters syndrome and fortunately, despite not completing the full 6-week course of intravesical BCG, he has not had recurrence of bladder tumor as well.
4. Conclusion
This case report of Reiters syndrome should be highlighted as a rare but significant complication of BCG immunotherapy and urologists should have a high index of suspicion to diagnose this rare complication. Early recognition of this syndrome will lead to prompt treatment, which includes cessation of BCG immunotherapy and symptomatic relief of the conjunctivitis and arthritic pain, thereby reducing the need for immunosuppressive therapy and progression to chronic arthritis.
References
- 1 I.B. Wu, R.A. Schwartz; Reiters syndrome: the classic triad and more; J Am Acad Dermatol, 59 (2008), pp. 113–121
- 2 E. Tinazzi, V. Ficarra, S. Simeoni, W. Artibani, C. Lunardi; Reactive arthritis following BCG immunotherapy for urinary bladder carcinoma: a systematic review; Rheumatol Int, 26 (2006), pp. 481–488
- 3 M.J. Rothe, F.A. Kerdel; Reiter syndrome; Int J Dermatol, 30 (1991), pp. 173–180
- 4 R.F. Willkens, F.C. Arnett, T. Bitter, et al.; Reiters syndrome. Evaluation of preliminary criteria for definite disease; Arthritis Rheum, 24 (1981), pp. 844–849
- 5 A. Keat; Reiters syndrome and reactive arthritis in perspective; N Engl J Med, 309 (1983), pp. 1606–1615
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?