Keywords
Cytomegalovirus ; Endoscopy ; Enteritis
Introduction
Gastrointestinal (GI) cytomegalovirus (CMV) disease is common in patients who are immunocompromised but is rare in immunocompetent hosts. Regardless of the host factor, CMV colitis accounts for the majority of cases of GI CMV disease [1] . CMV enteritis is quite exceptional, particularly in an immunocompetent host. The endoscopic findings and clinical features have not well been recognized.
We report a case of CMV enteritis with an unusual endoscopic finding of diffuse suppurative inflammation in the small intestine. To the best of our knowledge, this is the first report in the English literature of CMV enteritis in an immunocompetent patient with this atypical endoscopic finding.
Case report
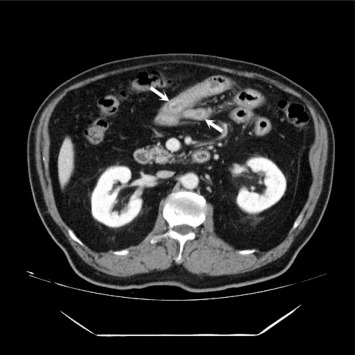
A 70-year-old man was in relatively good health before symptoms appeared and had no history of diabetes mellitus, hypertension, immunosuppressive drug intake, or habitual alcohol drinking. He was admitted to our hospital because he was having severe, watery diarrhea along with fever and abdominal pain about three to four times a day and had a body weight loss of approximately 8 kg within 2 weeks. The patient visited another hospital first and an initial esophagogastroduodenoscopy showed nonspecific findings. Abdominal computed tomography and an upper GI series disclosed a long segmental wall thickening at the distal duodenum and jejunum (Fig. 1 ). As the symptoms persisted, he was transferred to our hospital for further investigation and treatment.
|
|
|
Figure 1. The abdominal computed tomography scan shows a long segmental luminal narrowing at the distal duodenum and jejunum. |
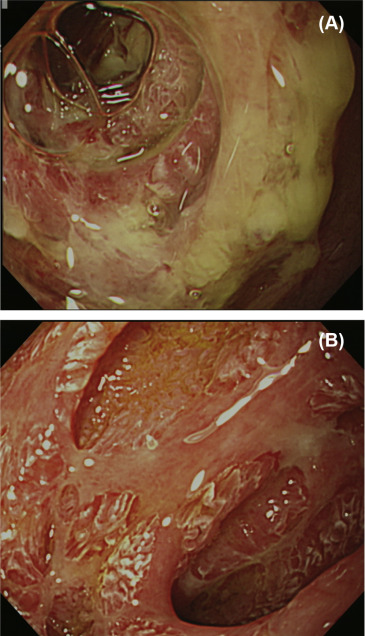
On admission, the patient appeared to have acute illness, with blood pressure of 127/77 mmHg, heart rate of 82 beats/min, respiratory rate of 16 breaths/min, and body temperature of 36.8°C. Physical examination revealed localized tenderness over epigastric and paraumbilical areas. Initial laboratory investigations were normal except for leukocytosis (white blood cell count: 12,400/mm3 ), low serum albumin (1.8 g/dL; normal 3.5-5.0) and high C-reactive protein level (10.0 mg/dL; normal below 0.5). Esophagogastroduodenoscopic and colonoscopic evaluations were normal. On enteroscopic examination, an extensive inflammatory change with a large amount of mucopurulent exudates with fibrotic and necrotic tissue scattered was noticed after the third portion of duodenum (Fig. 2 A). A closer view showed a complete loss of mucosal architecture with some mucosa islands (Fig. 2 B). The differential diagnosis after first enteroscopy was acute bacterial enteritis, inflammatory bowel disease like Crohn disease, and viral enteritis. Multiple biopsy specimens of the jejunum were sent to pathology for histologic examination, which only showed infiltration of dense inflammatory cells. There was no caseating granulomatous inflammation, evidence of Crohn disease, or other specific findings of viral infection. The culture and polymerase chain reaction for tuberculosis of the biopsy specimen were also negative. Under the tentative diagnosis of bacterial enteritis, the patient received total parenteral nutrition and broad-spectrum antibiotics with ceftriaxone plus metronidazole for 2 weeks. The subsequent serologic study was positive for anti-CMV immunoglobulin (Ig)G, negative for anti-CMV IgM, and negative for antihuman immunodeficiency virus. Immunological assessment for CD4 and CD8 lymphocytes was also found to be normal.
|
|
|
Figure 2. Endoscopic photographs of cytomegalovirus disease in the small intestine. (A) Extensive inflammatory change with mucopurulent appearance on the distal duodenum and jejunum. (B) A closer view shows a complete loss of mucosal architecture with some mucosa islands. |
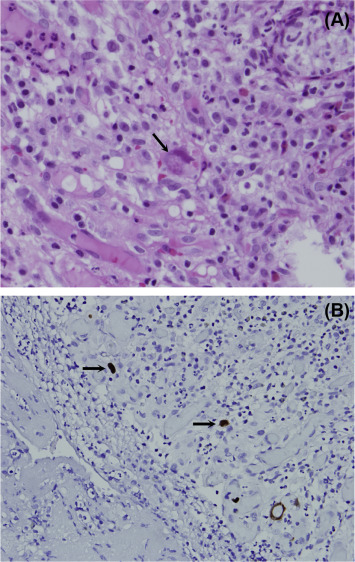
The patients clinical condition deteriorated rapidly and he underwent repeated enteroscopy 2 weeks later. There was no obvious change and endosopic biopsy was performed again. The specimen obtained during the repeated enteroscopy revealed an endothelial cell that exhibits CMV cytopathic changes with periodic acid-Schiff (PAS) stain, and CMV inclusions were also positive in the immunohistochemistry (IHC) stain (Fig. 3 ). Ganciclovir was then prescribed under the diagnosis of CMV enteritis. The patients clinical condition improved and this patient was discharged after 2 weeks of therapy. At 6 months' posttreatment follow-up, the patient was well and had no other gastrointestinal symptoms.
|
|
|
Figure 3. The typical cytomegalovirus (CMV) inclusions are seen in stromal cytomegalic cells of the lamina propria. (A) Periodic acid-Schiff stain (hematoxylin and eosin, 400×). (B) Typical brown CMV inclusions within the endothelial cell positive for CMV immunohistochemistry stain (hematoxylin and eosin, 400×). |
Discussion
GI CMV is common in immunocompromised patients but rare in the immunocompetent hosts. CMV enteritis is a highly lethal disease and early diagnosis is crucial to enable prompt treatment. Nevertheless, it is challenging when CMV infection of the GI tract occurs in an immunocompetent patient or in the small bowel, beyond the diagnostic fields of regular esophagogastroduodenoscopy and colonoscopy. Currently, only limited case reports aimed to illustrate the clinical features of CMV enteritis in immunocompetent patients [2] ; [3] ; [4] The ileum is the most common site reported and distal duodenum or jejunum is rare. Although diarrhea is the most common symptom, bowel perforation and hematochezia account for the crucial presentations. For our case, the patient recovered uneventfully, which could be attributed to prompt diagnosis and treatment.
The presence of discrete, punched-out shallow ulcerations is a hallmark of GI CMV infection, but typical endoscopic findings in the small intestine were lacking. It could be aphthoid lesions, shallow ulcers to deep and geographic ulcers with edema, erythema, or hemorrhagic changes of surrounding mucosa [2] ; [5] , also presenting as segmental ischemic change [6] A previous study at Chang Gung Memorial Hospital described the endoscopic findings of enterocolitis as four different types: inflammatory mucosa alone, ulceration alone, inflammatory mucosa associated with ulcer, and submucosal tumor with ulcer [7] For our case, the endoscopic finding is quite different with the appearance of diffuse suppurative inflammation and exudation accompanying loss of mucosa architecture.
The diagnosis of CMV disease is often difficult. There is no reliable, noninvasive diagnostic test currently available. The definite diagnosis of CMV GI disease depends on serology, CMV antigen testing, and endoscopic method (or procedure) with biopsies and histologic findings. The mucosa may present with the direct or indirect demonstration of CMV in pathologic tissue. A diagnosis of CMV enteritis is substantiated by the presence of CMV inclusions [8] . However, the inclusions may be rare and difficult to detect [9] , especially in immunocompetent hosts. Therefore, a correct diagnosis depends on a high index of clinical suspicion and repeat endoscopic biopsy with PAS and IHC stain for CMV, which applied to this patient.
The primary therapy for clinically significant CMV infection is use of antiviral drugs such as ganciclovir and foscarnet. A previous study [10] suggested that young, otherwise healthy, well-selected patients can improve without the need for antiviral therapy, but immunocompromised patients and patients older than 55 years with comorbidities require antiviral therapy. Page et al [11] demonstrated that the mortality of CMV enteritis is significantly higher in healthy individuals, but not in immunocompromised patients who are easily identified for this disease. The reason may by attributable to delayed diagnosis and therapy [11] . Mortality is also higher in patients older than 65 years and increased time to institution of therapy [11] . In immunocompetent patients, under specific circumstances, antiviral therapy should be used as early as possible.
In conclusion, we reported a case of CMV enteritis in an immunocompetent patient, with unusual endoscopic findings showing diffuse suppurative inflammation, and repeat endoscopy according to the clinical suspicion made the treatment successful.
Conflicts of interest
All authors declare no conflicts of interest.
References
- [1] J.M. Cha, J.I. Lee, J.W. Choe, K.R. Joo, S.W. Jung, H.P. Shin, et al.; Cytomegalovirus enteritis causing ileal perforation in an elderly immunocompetent individual; Yonsei Med J, 51 (2010), pp. 279–283
- [2] E.Y. Chae, S.S. Lee, J.W. Chung, H.J. Kim, S.H. Park, A.Y. Kim, et al.; Cytomegalovirus enterocolitis in apparently immunocompetent hosts: evaluation of the radiologic findings and clinical features; J Comput Assist Tomogr, 34 (2010), pp. 892–898
- [3] N. Almeida, J.M. Romaozinho, P. Amaro, M. Ferreira, M.A. Cipriano, M.C. Leitao; Fatal mid-gastrointestinal bleeding by cytomegalovirus enteritis in an immunocompetent patient; Acta Gastroenterol Belg, 72 (2009), pp. 245–248
- [4] Y. Kakugawa, S.W. Kim, K. Takizawa, T. Kikuchi, A. Fujieda, F. Waki, et al.; Small intestinal CMV disease detected by capsule endoscopy after allogeneic hematopoietic SCT; Bone Marrow Transplant, 42 (2008), pp. 283–284
- [5] R.W. Goodgame; Gastrointestinal cytomegalovirus disease; Ann Intern Med, 119 (1993), pp. 924–935
- [6] J. Keates, S. Lagahee, P. Crilley, M. Haber, T. Kowalski; CMV enteritis causing segmental ischemia and massive intestinal hemorrhage; Gastrointest Endosc, 53 (2001), pp. 355–359
- [7] S.K. Chuah, C.S. Changchien, C.M. Kuo, K.L. Wu, K.W. Chiu, Y.C. Chiu, et al.; Gastrointestinal tract cytomegalovirus disease in southwestern Taiwan: a clinical study of 1950 endoscopic biopsies; Chang Gung Med J, 28 (2005), pp. 467–475
- [8] W.L. Drew; Cytomegalovirus infection in patients with AIDS; J Infect Dis, 158 (1988), pp. 449–456
- [9] G.A. Talmon; Histologic features of cytomegalovirus enteritis in small bowel allografts; Transplant Proc, 42 (2010), pp. 2671–2675
- [10] P. Galiatsatos, I. Shrier, E. Lamoureux, A. Szilagyi; Meta-analysis of outcome of cytomegalovirus colitis in immunocompetent hosts; Dig Dis Sci, 50 (2005), pp. 609–616
- [11] M.J. Page, J.C. Dreese, L.S. Poritz, W.A. Koltun; Cytomegalovirus enteritis: a highly lethal condition requiring early detection and intervention; Dis Colon Rectum, 41 (1998), pp. 619–623
Document information
Published on 15/05/17
Submitted on 15/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?