Summary
Background
Obesity and type II diabetes mellitus (T2DM) are closely related and difficult to control by current medical treatment. Bariatric surgery has been proposed for inadequately controlled T2DM in association with obesity. However, prediction of successful T2DM remission after surgery has not been clearly studied in Asian patients. This information might be helpful for applying gastrointestinal surgery as metabolic surgery for T2DM.
Methods
This was a retrospective clinical study. From January 2002 to December 2008, 88 consecutive patients with morbid obesity, who were enrolled into a surgically supervised weight loss program, and who had T2DM before surgery with at least 1 year complete follow-up data were included. Sixty-eight (77.2%) patients received gastric bypass procedures, and the remaining 20 (22.8%) received restrictive procedures. We analyzed the available information during the initial evaluation of patients who were referred for bariatric surgery, by logistic regression analysis and data mining methods for predictors of successful diabetes remission after surgery.
Results
Overall, 68 (77.2%) of the 88 patients had remission of their T2DM 1 year after surgery. Patients in the bypass group had a higher remission rate than those in the restrictive group [59/68 (86.7%) vs. 9/20 (45.0%), p = 0.000]. In univariate analysis, patients who had T2DM remission after surgery were younger, heavier, had a wider waist, less severe disease, shorter duration, and higher C-peptide levels than those without remission. Type of operation and T2DM duration remained independent predictors of success after multivariate logistical regression analysis (p < 0.000). Data mining analysis confirmed that T2DM duration was the most important predictor.
Conclusions
Bariatric surgery is a treatment option for T2DM. Duration of diabetes is the most predictor of success after surgery.
Keywords
bariatric surgery;obesity;type 2 diabetes
1. Introduction
Obesity and its associated type 2 diabetes mellitus (T2DM) are an ongoing health-care problem worldwide.1 ; 2 Both diseases are closely related and difficult to control by current medical treatment, including diet, drug therapy and behavioral modification.3; 4 ; 5 Gastrointestinal surgery, performed as bariatric surgery, has been the most powerful ammunition for obesity treatment. There is strong evidence that bariatric surgery can cure most of the associated T2DM in patients with morbid obesity.6; 7; 8; 9; 10 ; 11 Remission of diabetes has been found to be associated with a range of excess weight loss after surgery.8 ; 9 Current consensus for bariatric surgery is set at body mass index (BMI) > 35 kg/m2 with comorbidity but gastrointestinal metabolic surgery recently has been proposed as a new treatment modality for obesity-related T2DM for patients with BMI < 35 kg/m2.12; 13; 14 ; 15 However, optimal outcomes for diabetes remission after bariatric surgery will occur if patients who are best suited to the surgery are selected and those who will predictably have a poor result are excluded.16 Furthermore, it could be that certain categories of patients are better suited to one type of bariatric procedure. To be able to make such decisions, we need preoperative information on the association between possible predictors and outcome.
The aim of this study was to examine the efficacy of surgically induced weight loss on diabetes remission. Furthermore, we looked for the preoperative predictors of diabetes remission after bariatric surgery.
2. Patients and methods
2.1. Patients
From January 2002 to December 2008, 88 (10.8 %) out of 811 patients who were enrolled in a surgically supervised program for weight reduction, and who had T2DM before surgery with at least 1 year follow-up, were retrospectively identified and included. There were 53 female and 35 male patients with a mean age of 35.7 years (range: 18–64 years) and a mean BMI of 39.5 kg/m2 (range: 30.0–61.7 kg/m2). Diagnosis and classification of T2DM was based on fasting plasma glucose concentrations ≧ 126 mg/dL or those with positive history and under antidiabetic medications.17 Remission of diabetes was defined in this study as a fasting plasma glucose level < 110 mg/dL or hemoglobin (Hb)A1C level < 6.4% without hypoglycemic medication at 1 year after surgery. The institutional review board approved this study.
Blood was drawn for laboratory examination from an antecubital vein following an overnight fast. The test was measured on the Hitachi 7170 and with the J&J nepholometer assay (Dade Behring, USA). C-peptide levels were measured with DPC Immulite analyzer. All specimens were processed within 24 hours of collection and then stored at –30°C until assay. Insulin resistance (IR) was measured by homeostatic model assessment–insulin resistance (HOMA-IR) index, which can be calculated as plasma glucose (mmol/L) × insulin (IU/mL)/22.5.18
2.2. Interventions
Among the 88 patients in the study group, the surgical procedures performed included restrictive type in 20 (22.8%) patients and gastric bypass procedures in 68 (77.2%) patients. The restrictive procedures included laparoscopic adjustable gastric banding (LAGB, using Lap Ban from Bioenterics Corp., Carpinteria, CA, USA) in seven patients, and laparoscopic sleeve gastrectomy (LSG) in 13 patients. The gastric bypass included laparoscopic mini-gastric bypass (LMGBP) in 68 patients. The techniques of LAGB and LMGBP are described in detail elsewhere.19; 20 ; 21 All procedures were performed by laparoscopic surgery. No drain was left. All the trocar wounds were closed by the mesh plug technique using bioabsorbable hemostatic gauze (Cellulostat, Horng Tzer Medical Instruments, Kaohsiung, Taiwan).22 The patients chose either procedure after discussion with a surgeon on an individual basis. There was no operative mortality in this series. One patient (1.1%) developed a major complication of leakage and five (5.6%) had minor complications.
2.3. Statistical analyses
All statistical analyses were performed using SPSS version 12.01 (SPSS Inc., Chicago, IL, USA), with baseline comparison made using χ2 tests and two-sample t tests. Continuous variables were expressed as mean ± standard deviation (SD), with differences expressed as mean ± SD. A two-sided p value < 0.05 was considered statistically significant.
We performed a predictor of diabetes resolution analysis using binary logistic regression, and a data mining technology of artificial neural networks (ANNs) was used to examine the associates of diabetes remission. Neural networks mimic human neurobiological information-processing activities. Analyses applied in this study were Back Propagation Neural networks (BPNs) conformed to a three-layered perception architecture. All preoperative factors were set as the input nodes in the input layer with only one dependent factor (successful diabetes remission) as the output node in the output layer. Details of this analysis have been described previously.23 ; 24 We further compared the performance of ANNs and the logistic regression model by using the cross-validation method. ANNs were constructed using Qnet97 (Vesta Services Inc., 1998).
3. Results
3.1. Patient characteristics and weight loss after surgery
The preoperative clinical characteristics of all patients are shown in Table 1. Among the clinical characteristics of the study patients receiving different surgical procedures, patients with older age, lesser degrees of obesity, and longer duration of diabetes preferred the restrictive mode of surgery at baseline (Table 1). The accompanying metabolic parameters were comparable for blood pressure, fasting plasma glucose, and plasma lipid levels between both groups.
| Bypass (n = 68) | Restrictive (n = 20) | p value | |
|---|---|---|---|
| Age (yr) | 34.4 ± 10.7 | 40.4 ± 11.2 | 0.024* |
| Sex, M/F | 28/40 | 7/13 | 0.620 |
| BMI (kg/m2) | 40.5 ± 8.0 | 36.2 ± 5.6 | 0.034* |
| Waist (cm) | 120.0 ± 15.9 | 113.6 ± 16.3 | 0.073 |
| SBP (mmHg) | 136.0 ± 15.1 | 130.7 ± 11.9 | 0.262 |
| DBP (mmHg) | 81.1 ± 9.9 | 81.4 ± 7.8 | 0.984 |
| FPG (mg/dL) | 207.7 ± 87.1 | 230.1 ± 92.9 | 0.458 |
| Total cholesterol (mg/dL) | 206.4 ± 49.0 | 214.6 ± 52.9 | 0.690 |
| Triglyceride (mg/dL) | 280.9 ± 287.4 | 273.3 ± 151.4 | 0.165 |
| HDL-C (mg/dL) | 44.4 ± 21.1 | 40.2 ± 7.7 | 0.494 |
| HbA1C (%) | 8.4 ± 2.2 | 8.9 ± 2.5 | 0.433 |
| C-peptide (ng/mL) | 5.3 ± 3.4 | 5.2 ± 4.3 | 0.552 |
| HOMA-IR | 17.9 ± 23.3 | 16.4 ± 19.2 | 0.986 |
| Metabolic syndrome | 53 (77.9%) | 17 (85%) | 0.355 |
| Duration of DM (yr) | 1.6 ± 3.7 | 3.8 ± 4.0 | 0.002* |
| Insulin case (no.) | 2 (2.9%) | 2 (10%) | 0.183 |
- p < 0.05. BMI = body mass index; DBP = diastolic blood pressure; DM = diabetes mellitus; F = female; FPG = fasting plasma glucose; HbA1c = hemoglobin A1c; HDL-C = high-density lipoprotein cholesterol; HOMA-IR = Homeostasis model assessment–insulin resistance17; M = male; SBP = systolic blood pressure.
At 1 year after surgery, with a greater body weight loss in the gastric bypass group than in the restrictive group (35.0 ± 16.1 vs. 18.7 ± 11.2 kg, p < 0.0001), individuals who underwent gastric bypass experienced a higher rate of excess weight loss (69.4 ± 19.3% vs. 52.0 ± 30.3%, p = 0.021) and achieved a similar BMI (28.3 ± 5.0 vs. 29.5 ± 7.1 kg/m2, p = 0.854) compared to individuals who underwent restrictive type surgery.
3.2. Diabetes remission and other health outcomes
Remission of T2DM was achieved in a total of 68 (77.2%) patients at 1 year after bariatric surgery. Patients in the bypass group had a higher diabetes remission rate than those in the restrictive group [59/68 (86.7%) vs. 9/20 (45.0%), p = 0.000]. The accompanying metabolic parameters, that is, fasting plasma glucose, blood lipid levels and HbA1c significantly improved in the individuals who underwent gastric bypass surgery (Table 2). The degree of IR was also much better in the individuals who underwent gastric bypass surgery, with a lower level of fasting insulin/C-peptide and HOMA-IR index. The patients who underwent gastric bypass surgery manifested a lower frequency of metabolic syndrome (10.2% vs. 50%, p < 0.001) and reached a higher rate of diabetes remission (86.7% vs. 45%; p < 0.001), as shown in Table 2.
| Bypass (n = 68) | Restrictive (n = 20) | p value | |
|---|---|---|---|
| BMI (kg/m2) | 28.3 ±5.0 | 29.5 ±7.1 | 0.854 |
| % of BMI loss | 30.1% | 18.5% | 0.001* |
| Waist (cm) | 92.4 ± 13.5 | 93.8 ± 16.5 | 0.815 |
| SBP (mmHg) | 124.1 ± 16.2 | 128.8 ± 15.3 | 0.290 |
| DBP (mmHg) | 74.5 ± 11.2 | 77.1 ± 11.0 | 0.561 |
| FPG (mg/dL) | 90.0 ± 19.1 | 121.1 ± 44.8 | 0.000* |
| Total cholesterol (mg/dL) | 159.1 ± 29.5 | 194.3 ± 25.5 | 0.000* |
| Triglyceride (mg/dL) | 88.6 ± 41.6 | 145.0 ± 66.1 | 0.000* |
| HDL-C (mg/dL) | 47.8 ± 12.7 | 44.8 ± 7.3 | 0.473 |
| HbA1C (%) | 5.3 ± 0.5 | 6.5 ± 1.2 | 0.000* |
| C-peptide (ng/mL) | 1.7 ± 0.9 | 2.3 ± 1.3 | 0.014* |
| HOMA-IR | 1.1 ± 1.0 | 2.6 ± 2.2 | 0.002* |
| Metabolic syndrome | 7 (10.2%) | 10 (50%) | 0.000* |
| DM remission | 59 (86.7%) | 9 (45%) | 0.000* |
- p < 0.05. BMI = body mass index; DBP = diastolic blood pressure; DM = diabetes mellitus; FPG = fasting plasma glucose; HbA1c = hemoglobin A1c; HDL-C = high-density lipoprotein cholesterol; HOMA-IR = homeostasis model assessment–insulin resistance17; SBP = systolic blood pressure.
3.3. Predictor analyses for diabetes remission
We used two methods to identify preoperative factors that were likely to predict diabetes remission after surgical treatment. Logistic regression analysis between those with and without T2DM remission disclosed 12 positive preoperative clinical predictors of remission (Table 3). In the more obese patients who had a higher BMI, weight had better remission 1 year after surgery. Patients with more severe status in insulin and C-peptide and shorter T2DM history had a better remission rate. Multivariate analysis confirmed that the mode of operation and duration of T2DM history had significant effects on remission (p < 0.0001). The average correct classification rate of logistic regression was 85.9% (Table 4).
| Factor | Not remission (n = 20) | Remission (n = 68) | p value |
|---|---|---|---|
| Age, yr | 44.4 ± 9.7 | 33.2 ± 10.2 | 0.000* |
| Weight (kg) | 92.3 ± 19.5 | 115.0 ± 25.9 | 0.000* |
| BMI (kg/m2) | 34.3 ± 4.3 | 41.1 ± 7.8 | 0.000* |
| Waist (cm) | 111.5 ± 12.1 | 120.7 ± 16.6 | 0.010* |
| FPG (mg/dL) | 247.6 ± 84.9 | 202.6 ± 87.4 | 0.038* |
| AST (IU/L) | 28.1 ± 15.8 | 44.5 ± 27.5 | 0.013* |
| ALT (IU/L) | 37.9 ± 24.8 | 69.6 ± 50.2 | 0.004* |
| Insulin (IU/L) | 17.6 ± 15.6 | 47.2 ± 70.4 | 0.020* |
| HbA1C (%) | 9.8 ± 2.3 | 8.2 ± 2.1 | 0.006* |
| C-peptide (ng/mL) | 3.4 ± 1.6 | 5.9 ± 3.9 | 0.004* |
| Duration of DM (yr) | 6.1 ± 5.2 | 0.9 ± 2.3 | 0.000* |
| Insulin case (no.) | 4 (20%) | 0 (0%) | 0.000* |
- p < 0.05. ALT = alanine aminotransferase; ALT = aspartate aminotransferase; BMI = body mass index; DM = diabetes mellitus; FPG = fasting plasma glucose; HbA1c = hemoglobin A1c.
| Factor | 95% CI | p value |
|---|---|---|
| Operative methods | 0.000–0.212 | 0.000* |
| Diabetes duration | 0.020–2.126 | 0.000* |
- p < 0.05.
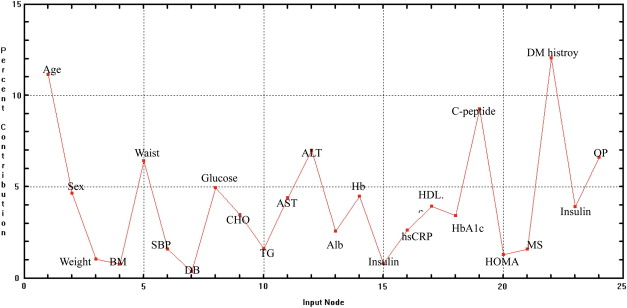
Consistent with the logistic regression model, ANNs also confirmed that duration of T2DM history was the most important predictor of diabetes remission after surgery. Age was another independent predictor but not type of surgery. Fig. 1 shows the relative importance of preoperative predictor variables. The average correct classification rate of the BPN model was 90.4%.
|
|
|
Figure 1. Relative importance of preoperative predictor variables for diabetes remission (significant factor was defined by those with percent contribution > 10). Alb = albumin; ALT = alanine aminotransferase; AST = aspartate aminotransferase; BM = body mass index; CHO = total cholesterol; DBP = diastolic blood pressure; Hb = hemoglobin; HDL-C = high-density lipoprotein cholesterol; HOMA-IR = homeostasis model assessment–insulin resistance; hsCRP = high-sensitivity C-reactive protein; MS = metabolic syndrome; OP = methods of surgery; SBP = systolic blood pressure; TG = triglyceride. |
3.4. Duration of T2DM and diabetes remission
The T2DM remission rates for those with disease duration < 2 years, 2–5 years and > 5 years were 57/59 (98.5%), 7/17 (39.3%) and 4/12 (37.3%), respectively (p < 0.001) (Table 5). For the restrictive group, the remission rate was 100% in patients with duration of T2DM < 2 years. The T2DM remission rates for those with preoperative C-peptide < 3 ng/mL, 3–6 ng/mL and > 6 ng/mL were 9/18 (60.0%), 25/33 (75.7%) and 19/21 (90.1%), respectively (p = 0.001) (Table 6). The T2DM remission rate dropped dramatically in the restrictive group for patients with C-peptide < 6 ng/mL. Both duration of T2DM and C-peptide level had a significant predictive power for diabetes remission in the restrictive group compared with the bypass group.
| Duration (yr) | < 2 | 2–5 | > 5 | p |
|---|---|---|---|---|
| All patients | 98.5% (57/59) | 39.3% (7/17) | 33.3% (4/12) | 0.000* |
| Bypass group | 98.1% (51/53) | 55.6% (5/9) | 50.0% (3/6) | 0.005* |
| Restrictive group | 100.0% (6/6) | 25.0% (2/8) | 16.7% (1/6) | 0.000* |
T2DM = type 2 diabetes mellitus.
- p < 0.05.
| C-peptide (ng/mL) | <3 | 3–6 | >6 | p |
|---|---|---|---|---|
| All patients | 60% (9/18) | 75.7% (25/33) | 90.1% (19/21) | 0.001* |
| Bypass group | 71.4% (7/12) | 92.3% (24/26) | 93.3% (14/15) | 0.014* |
| Restrictive group | 33.3% (2/6) | 14.3% (1/7) | 83.3% (5/6) | 0.037* |
- p < 0.05.
4. Discussion
In this report, we show that bariatric surgery is a promising treatment for obese Asian patients with inadequately controlled T2DM. The overall 1-year remission rate was 77.9% for a group of T2DM patients with mean HbA1c of 8.6%. In previous studies by Pories et al and Shauer et al, the resolution rate of T2DM in Caucasian patients with morbid obesity after gastric bypass was 88%, which agrees with our study.6 ; 25 Successful remission of T2DM in this group of patients can be translated to a decrease in diabetes-related mortality. Recent studies have disclosed that bariatric surgery can reduce mortality by up to 30–40%, and more important is that the reduction of mortality by bariatric surgery is mostly attributed to the reduction in diabetes-related death.10 ; 11 These data constitute a good argument for proposing metabolic surgery in inadequately controlled obesity-related T2DM patients as soon as possible.
The most important finding of the present study was that duration of T2DM was the most important predictor of diabetes remission after surgery. Old age, longer T2DM history and use of insulin have been found to be negative predictors of T2DM remission in previous studies of bariatric surgery in patients with morbid obesity.6 ; 26 However, no data were available for Asian patients. The duration of T2DM turned out to be the most important predictor for Asian patients in our study. Although the duration might be inconsistent and influenced by the attitude of both patients and doctors, duration of diabetes does reflect the residual β-cell mass in T2DM patients. This study and others also support the thesis that duration of diabetes is probably more important than type of surgery to predict a successful result of surgical treatment of diabetes.25; 26 ; 27 Therefore, duration of diabetes may not only be a criterion for patient selection but also for choice of different surgical procedure.
Type of surgery was another independent predictor by multivariate analysis in the present study. Gastric bypass has been proven to have a better weight reduction and higher diabetes remission rate compared with purely restrictive procedures. Although less effective in diabetes remission than gastric bypass surgery, restrictive type surgery is 10 times safer than a complex gastric bypass procedure,8 and avoids the long-term sequelae of micronutrient deficiency following duodenum exclusion,28 ; 29 and should still be considered as the first choice in gastrointestinal metabolic surgery.30 For restrictive type surgery, Dixon et al have reported a T2DM remission rate of 73% for gastric banding, which is much higher than the 45% in the present study.12 However, in the study of Dixon et al, only newly diagnosed patients with duration of T2DM < 2 years were recruited. In this study, the remission rate of restrictive type surgery for those with duration of T2DM < 2 years was 100%. For other restrictive type surgery, Vidal et al also have reported a 100% T2DM remission rate in patients with morbid obesity receiving sleeve gastrectomy.31 In the study of Vidal et al, the patients were all morbidly obese with a mean BMI of up to 51.9 kg/m2 but no duration of T2DM was available. However, another recent study also has reported that remission of T2DM after sleeve gastrectomy dropped to 13% in those with duration of T2DM > 5 years, which is similar to the present study.27 For gastric bypass, a recent study has demonstrated a decrease in diabetes remission in patients with duration of T2DM > 10 years.32 Taken together, for choice of surgical procedures, gastric banding may be considered for diabetes treatment in patients with duration of T2DM < 2 years. The recommended selection criteria for sleeve gastrectomy may be patients with duration of T2DM < 5 years. Sleeve gastrectomy has a better effect on weight loss than gastric banding; probably because of changes in ghrelin.33 Gastric bypass surgery is recommended for the rest of T2DM patients but they should have C-peptide > 1 ng/mL with central obesity.34 Further studies are required before conclusions are drawn about other surgical procedures.16
The mechanism for T2DM resolution after bariatric surgery is intriguing. Both restrictive and bypass surgery had been reported to be effective for remission of associated T2DM in patients with morbid obesity. In our previous study, both types of surgery were effective in reducing of IR but the mechanism was related to a caloric effect in the early phase and related to weight loss in the late phase.35 In a meta-analysis, remission of T2DM after bariatric surgery was dose-dependent for weight loss rather than procedure-dependent.8 For a long-term effect on remission of T2DM, sustained weight reduction plays a key role. However, recent studies have suggested the superior effect of gastric bypass over restricted procedures owing to a direct effect of bypass of the hormonally active foregut.36 Rubino and Marescaus have supported the theory in an animal model.37 ; 38 Other studies also have demonstrated an increase in the hindgut hormones, such as GLP-1 and PYY after gastric bypass.39 ; 40 In the present study, the bypass group did have a higher T2DM remission rate compared to the restrictive group. Although the remission of T2DM seems to correlate with weight reduction in different groups, the bypass group had a superior advantage in T2DM remission, other than via weight loss.
Age was also a significant predictor by ANN analysis in the present study. Old age reflected a deteriorating pancreatic preserve and diminished B-cell reserve, which might be evaluated by C-peptide level. C-peptide is a connecting peptide to insulin and a valuable test in the classification of diabetes. Type 1 DM has low C-peptide levels, whereas in T2DM, C-peptide levels are above normal due to a compensatory increase in insulin production. However, in late stage T2DM, as β-cells are progressively destroyed, C-peptide level may become low.41 ; 42 Therefore, C-peptide levels in T2DM patients may reflect their pancreas preserve and predict the success of surgical treatment of T2DM. Preoperative C-peptide was found to be an important predictor of diabetes remission after sleeve gastrectomy in a recent study.42 In our study, the preoperative C-peptide level could also be used as a predictor of successful treatment, especially in restrictive type surgery. Although not an independent predictor, C-peptide levels in T2DM patients may reflect their pancreatic preserve and should be included in evaluating surgical treatment for T2DM.33 Other potential predictors for diabetes remission after surgical treatment, such as stimulated C-peptide level and incretin effect of the patients, require further exploration.
There were several limitations to this study. First, the case number was small. Although sleeve gastrectomy and gastric banding seem to result in different weight loss and gut hormone modulation,32 we did not have enough patients to analyze this point. Second, the 1-year follow-up period was short. The maximal weight reduction effect of restrictive surgery was > 1 year, although maximal weight loss usually happens within 1 year. The best diabetes remission effect of restrictive surgery might also be at > 1 year. Further study with longer follow-up is required to confirm this finding, as well as the durability of T2DM remission after bariatric surgery. Finally, this study was retrospective and procedure choice by the patient may have been biased and affected the conclusions. A randomized clinical trial is indicated before any firm conclusions can be made.
In conclusion, bariatric or gastrointestinal metabolic surgery is a promising treatment for inadequately controlled obesity-related T2DM patients with a 77.2% remission rate for associated diabetes. Although gastric bypass surgery is more effective for diabetes remission than restrictive type surgery, duration of diabetes is the most important predictor of diabetes remission after surgery.
Acknowledgments
This work was supported by a grant from Ming-Shen General Hospital (97-A-01).
References
- 1 P. Zimmer, K.G. Alberti, J. Shaw; Global and societal implications of the diabetes epidemic; Nature, 414 (2001), pp. 782–787
- 2 J.C. Chan, V. Malik, W. Jia, et al.; Diabetes in Asia: epidemiology, risk factor, and pathophysiology; JAMA, 301 (2009), pp. 2129–2140
- 3 Diabetes Control and Complications Trial. The relationship of glycemic exposure (HbA sub1c) to the risk of development and progression of retinopathy in the diabetes control and complications trial; Diabetes, 44 (1995), pp. 968–983
- 4 UK Prospective Diabetes Study Group; Intensive blood glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33); Lancet, 352 (1998), pp. 837–853
- 5 UK Prospective Diabetes Study Group; Effect of intensive blood glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPD 34); Lancet, 352 (1998), pp. 854–865
- 6 W.J. Pories, M.S. Swanson, K.G. MacDonald, et al.; Who would have thought it? An operation provides to be the most effective therapy for adult onset diabetes mellitus; Ann Surg, 222 (1995), pp. 339–352
- 7 L. Sjostrom, A.K. Lindroos, M. Peltonen, D.A. Scia, J.N. Clore; Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery; N Engl J Med, 351 (2004), pp. 2683–2693
- 8 H. Buchwald, Y. Avidor, E. Braunwald, et al.; Bariatric surgery: a systematic review and meta-analysis; JAMA, 292 (2004), pp. 1724–1737
- 9 H. Buchwald, R. Estok, K. Fahrbach, et al.; Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis; Am J Med, 122 (2009), pp. 248–256
- 10 L. Sjostrom, K. Narbro, D. Sjostrom, et al.; Effect of bariatric surgery on mortality in Swedish obese subjects; N Engl J Med, 357 (2007), pp. 741–752
- 11 T.D. Adams, R.E. Gress, S.C. Smith, et al.; Long-term mortality after gastric bypass surgery; N Engl J Med, 357 (2007), pp. 753–761
- 12 J.B. Dixon, P.E. O’Brien, J. Playfair, et al.; Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomized controlled trial; JAMA, 299 (2008), pp. 316–323
- 13 R. Cohen, J.S. Pinheiro, J.L. Correa, et al.; Laparoscopic Roux-en-Y gastric bypass for BMI < 35 kg/m2: a tailored approach; Surg Obes Relat Dis, 2 (2006), pp. 401–404
- 14 W.J. Lee, W. Wang, Y.C. Lee, et al.; Effects of laparoscopic mini-gastric bypass for type 2 diabetes mellitus: comparison of BMI > 35 and < 35 kg/m2; J Gastrointest Surg, 12 (2008), pp. 945–952
- 15 S.S. Shah, J.S. Todkar, P.S. Shah, et al.; Diabetes remission and reduced cardiovascular risk after gastric bypass in Asian Indians with body mass index < 35 kg/m2; Surg Obes Relat Dis, 6 (2010), pp. 332–340
- 16 F. Rubino, L.M. Kaplan, P.R. Schauer, et al.; The Diabetes Surgery Summit Consensus Conference: recommendations for the evaluation and use of gastrointestinal surgery to treat type 2 diabetes mellitus; Ann Surg, 251 (2010), pp. 399–405
- 17 Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus; Diabetes Care, 26 (2003), pp. S5–S20
- 18 D.R. Matthews, J.P. Hosker, A.S. Rudensky, et al.; Homeostasis model assessment: insulin resistance and B-cell function from fasting plasma glucose and insulin concentration in man; Diabetologia, 28 (1985), pp. 412–419
- 19 W.J. Lee, P.Y. Yu, W. Wang, et al.; Laparoscopic Roux-en-Y versus mini-gastric bypass for the treatment of morbid obesity: a prospective randomized controlled clinical trial; Ann Surg, 242 (2005), pp. 20–28
- 20 W.J. Lee, W. Wang, P.J. Yu, et al.; Gastrointestinal quality of life following laparoscopic adjustable gastric banding in Asia; Obes Surg, 16 (2006), pp. 586–591
- 21 K.H. Ser, W.J. Lee, Y.C. Lee, et al.; Laparoscopic sleeve gastrectomy; Surg Endosc, 24 (2010), pp. 2253–2259
- 22 C.C. Chiu, W.J. Lee, W. Wang, et al.; Prevention of trocar-wound hernia in laparoscopic bariatric operations; Obes Surg, 16 (2006), pp. 913–918
- 23 G. Cybenko; Approximation by superpositions of a sigmoidal Function; Math Control Signal, 2 (1989), pp. 303–314
- 24 K. Hornik, M. Stinchcombe, H. White; Multilayer feed forward networks are universal approximations; Neural Networks, 2 (1989), pp. 336–359
- 25 P.R. Schauer, B. Burguera, S. Ikramuddin, et al.; Effect of laparoscopic Roux-en Y gastric bypass on type 2 diabetes mellitus; Ann Surg, 238 (2003), pp. 467–485
- 26 J.B. Dixon, P.E. O’Brien; Health outcomes of severely obese type 2 diabetes subjects 1 year after laparoscopic adjustable gastric banding; Diabetes Care, 25 (2002), pp. 358–363
- 27 R. Rosenthal, X. Li, S. Samuel, et al.; Effects of sleeve gastrectomy on patients with diabetes mellitus; Surg Obes Relat Dis, 5 (2009), pp. 429–434
- 28 R.E. Brolin, J.H. Gorman, R.C. Gorman, et al.; Prophylactic iron supplementation after Roux-en-Y gastric bypass; Arch Surg, 133 (1998), pp. 740–744
- 29 C. Gasteyger, M. Suter, R.C. Gaillard, V. Giusti; Nutritional deficiencies after Roux-en-Y gastric bypass for morbid obesity often cannot be prevented by standard multivitamin supplementation; Am J Clin Nutr, 87 (2008), pp. 1128–1133
- 30 J. Vidal, F. Ibarzabai, F. Romero, S. Deigado, D. Momblan, F.A. Lacy; Type 2 diabetes mellitus and the metabolic syndrome following sleeve gastrectomy in severely obese subjects; Obes Surg, 18 (2008), pp. 1077–1082
- 31 T.C. Hall, M.G.C. Pellen, P.C. Sedman, P.K. Jain; Preoperative factors predicting remission of type 2 diabetes mellitus after Roux-en-Y gastric bypass surgery for obesity; Obes Surg, 20 (2010), pp. 1245–1250
- 32 F.B. Langer, M.A. Reza Hoda, A. Bohdjalian, et al.; Sleeve gastrectomy and gastric banding: effects on plasma ghrelin levels; Obes Surg, 15 (2005), pp. 1024–1029
- 33 M. Dietel; Surgery for diabetes at lower BMI: some caution; Obes Surg, 18 (2008), pp. 1211–1214
- 34 W.J. Lee, Y.C. Lee, K.H. Ser, J.C. Chen, S.C. Chen; Improvement of insulin resistance after obesity surgery: a comparison of gastric banding and bypass procedures; Obes Surg, 18 (2008), pp. 1119–1125
- 35 M.S. Hickey, W.J. Pories, K.G. MacDonald, et al.; A new paradigm for type 2 diabetes mellitus. Could it be a disease of the foregut?; Ann Surg, 227 (1998), pp. 637–644
- 36 F. Rubino, J. Marescaux; Effect of duodenal–jejunal exclusion in a non-obese animal model of type 2 diabetes: a new perspective for an old disease; Ann Surg, 239 (2004), pp. 1–11
- 37 F. Rubino, A. Forgione, D. Cummings, et al.; The mechanism of diabetes control after gastrointestinal bypass surgery reveals a role of the proximal small intestine in the pathophysiology of type 2 diabetes; Ann Surg, 244 (2006), pp. 741–749
- 38 R. Morinigo, V. Moize, M. Mustri, et al.; GLP-1, PYY, hunger and satiety following gastric bypass surgery in morbidly obese subjects; J Clin Endocrinol Metab, 91 (2006), pp. 1735–1740
- 39 B. Laferrere, J. McGinty, S. Heshka, et al.; Incretin levels and effect are markedly enhanced 1 month after roux-en-Y gastric bypass surgery in obese patients with type 2 diabetes; Diabetes Care, 30 (2007), pp. 1709–1716
- 40 P. Zimmet, R. Tumer, D. McCarty, et al.; Crucial points at diagnosis. Type 2 diabetes or slow type 1 diabetes; Diabetes Care, 22 (1999), pp. B59–B64
- 41 M. Landin-Olsson; Latent autoimmune diabetes in adults; Ann NY Acad Sci, 958 (2002), pp. 112–116
- 42 W.J. Lee, K.H. Ser, K. Chong, et al.; Laparoscopic sleeve gastrectomy for diabetes treatment in nonmorbidly obese patients: efficacy and change of insulin secretion; Surgery, 147 (2010), pp. 664–669
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?