Summary
Introduction
To report our experience in palliative hepaticojejunostomy for advanced malignant biliary obstruction by means of robotic approach
Methods
Robot-assisted laparoscopic hepaticojejunostomy for advanced malignant biliary obstruction was performed in nine patients from May 2009 to April 2014.
Results
During the study period, robotic hepaticojejunostomy for advanced malignant biliary obstruction was completed successfully in nine patients. Roux-en-Y hepaticojejunostomy and double (hepaticojejunostomy, and gastrojejunostomy) bypass were performed in five and four patients, respectively. The mean operating time was 212.8 minutes. The mean blood loss was 38.7 mL. The overall complication rate was 22.2%. Bile leak complication occurred in one patient only. There was no procedure-related mortality. The mean postoperative hospital stay was 13.3 days. Five patients received palliative systemic chemotherapy after bypass surgery. The mean survival time was 11.1 months. During follow up, only three patients with cholangiocarcinoma had recurrent biliary obstruction after end-to-side hepaticojejunostomy due to tumor progression, and needed percutaneous transhepatic biliary drainage. Among these nine patients, there were a total of eight episodes of readmission in four patients due to tumor-related symptoms or complications.
Conclusions
Robot-assisted laparoscopic hepaticojejunostomy for advanced malignant biliary obstruction had a low complication rate and was associated with an improved quality of life.
Keywords
cholangiocarcinoma;hepaticojejunostomy;jaundice;pancreatic cancer;robot
1. Introduction
Stenting of the biliary tree is a common palliative procedure to relieve obstructive jaundice in advanced malignancy. However, the methods adopted for palliation should be able to provide optimum palliation and restoration of quality of life with minimal physical trauma, low morbidity, and rapid recovery. The minimally invasive approach of surgical biliary bypass has these potential advantages. Laparoscopic biliary bypass has the potential advantages of earlier recovery, less postoperative pain, shorter hospital stay, and better cosmetic outcome. However, laparoscopic hepaticojejunostomy remains a surgical challenge, despite the recent advances in minimally invasive surgical techniques, because of its high degree of complexity.1 ; 2 Its application cannot be popularized. In an attempt to overcome this limitation and to facilitate the difficult steps in the minimally invasive surgery for hepaticojejunostomy, robot-assisted laparoscopic hepaticojejunostomy may be a solution. There are many special advantages of robotic system, which overcome the obstacles of conventional laparoscopic surgery.3 They improve visualization, restore proper hand-eye coordination, increase dexterity, and an ergonomic position. However, this technique and application was rarely reported.
We report our experience in hepaticojejunostomy for advanced malignancies by means of a robotic approach.
2. Materials and methods
Use of the robotic system for general surgery in our hospital began in May 2009. The da Vinci S Surgical System (Intuitive Surgical Inc., Sunnyvale, CA, USA) was used for all robot-assisted procedures. Since then, a prospective database has tracked all robot-assisted laparoscopic procedures. Between May 2009 and April 2014, nine consecutive patients undergoing robot-assisted laparoscopic palliative hepaticojejunostomy for advanced malignancies were identified in our prospectively collected database. Their demographics, pathology, perioperative outcomes, and follow-up progress were recorded in the database. All operations were performed by consultant surgeons with experience in the conventional laparoscopic technique.
2.1. Operative technique
The patient is placed in a supine position with legs apart. The patient is placed in a 20° reverse Trendelenburg position. A 12-mm port was placed through a subumbilical incision using a standard open technique. Then, one 12-mm assistant port and three 8-mm robotic ports are inserted under direct vision. An assistant port was used for passing sutures, passing endostaplers, water irrigation, and doing suction by the bedside surgeon. After staging laparoscopy and laparoscopic ultrasound assessment, the robot system is docked in.
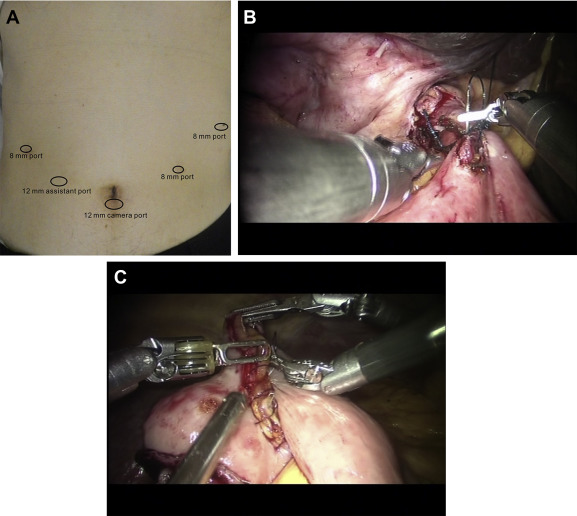
The following procedure is similar to the open approach. In order to prepare a Roux limb, a single jejunal Roux limb approximately 60 cm from the ligament of Treitz is selected and transected with endostaplers. The Roux limb is brought up in an antecolic fashion for a tension-free hepaticojejunal anastomosis. For palliation of malignant distal biliary strictures, a side-to-side sutured hepaticojejunal anastomosis is fashioned. For palliation of more proximal malignant biliary strictures, an end-to-side sutured hepaticojejunal anastomosis is fashioned after transection of the bile duct. For a thin bile duct wall, interrupted 3/0 Monocryl (Ethicon, Inc. Johnson and Johnson Company, Somerville, NJ, USA) sutures were used. For a thickened bile duct wall, continuous 3/0 V-loc (Covidien, Dublin, Ireland) sutures were used. Side-to-side jejunojejunostomy is fashioned at about 40 cm from the hepaticojejunal anastomosis. If a double gastric and biliary bypass is to be performed, then the hepaticojejunal anastomosis is performed first and the gastrojejunal anastomosis second (Fig. 1A–C).
|
|
|
Figure 1. (A) Port sites position (one subumbilical 12 mm camera port, three 8 mm ports for robotic arms, and one 12 mm assistant port for bedside surgeon); (B) side-to-side hepaticojejunostomy was fashioned with interrupted 3/0 Monocryl (Ethicon, Inc. Johnson and Johnson Company, Somerville, NJ, USA) sutures; (C) side-to-side jejunojejunostomy (Roux-en-Y reconstruction) was fashioned with running 3/0 Monocryl (Ethicon, Inc. Johnson and Johnson Company) sutures. |
2.2. Statistical method
Continuous variables were expressed as mean ± standard deviation (SD) or range.
3. Results
During the study period, robot-assisted laparoscopic palliative hepaticojejunostomy was completed successfully in nine patients. Baseline characteristics of the patients are shown in Table 1.
| Sex (male/female) (n) | 5/4 |
| Mean age (y) | 71.6 ± 10.5 |
| Pathologies (n) | |
| Ca head of pancreas | 4 |
| Ca ampulla | 1 |
| Cholangiocarcinoma | 4 |
| Causes of inoperability (n) | |
| Metastases | 4 |
| Locally advanced with major vascular encasement or invasion | 5 |
| Operations (n) | |
| Hepaticojejunostomy | 5 |
| Hepaticojejunostomy + gastrojejunostomy | 4 |
| Mean operation time (min) | 212.8 ± 68.9 (SD) |
| Mean blood loss (mL) | 38.7 (range, 3–50) |
| Overall complications (n) | 2 (22.2%) |
| Intra-abdominal collection | 0 |
| Bile leak | 1 |
| Gastrojejunal anastomotic ulcer | 1 |
| Wound infection | 0 |
| Mean postoperative hospital stay (d) | 13.3 (range, 5–53) |
| Recurrent gastric outlet obstruction during follow-up (n) | 0 |
| Recurrent biliary obstruction with PTBD insertion during follow-up (n) | 3 |
| Number of patients with readmission (n) | |
| Anemia | 1 |
| Biliary obstruction | 3 |
| Total episodes of admission due to tumor-related symptoms or complications (n) | 8 |
| Mean overall survival (mo) | 11.1 ± 7.2 |
Roux-en-Y hepaticojejunostomy and double (hepaticojejunostomy and gastrojejunostomy) bypass was performed in five and four patients, respectively. The mean operating time was 212.8 minutes. The mean blood loss was 38.7 mL. The overall complication rate was 22.2%. Bile leak complication occurred in one patient only. There was no procedure-related mortality. The mean postoperative hospital stay was 13.3 days. Five patients received palliative systemic chemotherapy after bypass surgery. The mean survival time was 11.1 months. During follow up, three patients with cholangiocarcinoma over the common hepatic duct (n = 1), and mid-part of the common bile duct (n = 2) had recurrent biliary obstruction due to tumor progression after end-to-side hepaticojejunostomy, and needed percutaneous transhepatic biliary drainage. Among these nine patients, there were just eight episodes of readmission in four patients due to tumor-related symptoms or complications ( Table 1).
4. Discussion
The ideal palliative treatment for unresectable malignancies that cause biliary obstruction should have a low incidence of procedure-related complications and a long-term relief of obstructive jaundice with minimal need for reintervention. Surgical biliary bypass via the laparoscopic approach is one of the feasible options. As with most laparoscopic operations, laparoscopic palliative hepaticojejunostomy follows the same surgical principle as its open counterpart, but with reduced physical trauma. The potential advantages of laparoscopic palliative bypass surgery for advanced malignancies are those of minimally invasive surgery, such as earlier recovery, shorter hospital stay, and better cosmetic outcome. However, for the group of patients with advanced malignancies, the surgical bypass with earlier recovery can transform into a better chance of receiving palliative systemic or local therapy, and having a better quality of life. There was a low rate of anastomosis occlusion and need for repeat procedures in patients treated by surgical bypass.
Laparoscopic hepaticojejunostomy has been reported but the experience remains limited, because laparoscopic suturing requires advanced skills, requiring versatile, fine, and precise movements to manipulate and suture tissue within a confined space. The majority of reports were concentrated on the pediatric group with choledochal cysts. Conventional laparoscopic surgery has its own limitations, including a reduced degree of freedom of movement and a two-dimensional view instead of a three-dimensional operative field, and poor ergonomics. These limitations translate into a long learning curve, which requires a lot of time and effort to acquire such advanced laparoscopic skills. These limitations of conventional laparoscopic surgery were the impetus behind the development of robotic surgery. The robotic system appears to provide some advantages to the surgeon. To our best knowledge, human experiences of robotic hepaticojejunostomy have only been reported in pediatric groups with choledochal cysts, and patients with recurrent pyogenic cholangitis.4; 5; 6; 7; 8 ; 9 Some of the experiences were from robotic pancreaticoduodenostomy.10; 11 ; 12 Its application as palliative bypass in advanced malignancy was reported in an animal study only.13 Although the study population was not large, the technique was safe, feasible, and easy.
Our study evaluated the perioperative outcome and follow-up results of robot-assisted laparoscopic Roux-en-Y hepaticojejunostomy in patients with advanced malignancy. To our best knowledge, this was the first reported series in this area. The robotic system makes surgeries that were technically difficult previously, now possible. Although the current series was small, the robotic approach was associated with a low complication rate, a low reintervention rate, and a low readmission rate. These advantages also allowed patients to receive palliative systemic therapy in an earlier time, and to have less interruption due to tumor-related complications during the course of palliative systemic therapy. These also transformed into a better quality of life.
In conclusion, robot-assisted laparoscopic hepaticojejunostomy for advanced malignant biliary obstruction had a low complication rate and was associated with an improved quality of life.
References
- 1 S.L. Liu, L. Li, W.Y. Hou, et al.; Laparoscopic excision of choledochal cyst and Roux-en-Y hepaticojejunostomy in symptomatic neonates; J Pediatr Surg, 44 (2009), pp. 508–511
- 2 C.N. Tang, W.T. Siu, J.P. Ha, C.K. Tai, K.K. Tsui, M.K. Li; Laparoscopic biliary bypass–a single centre experience; Hepatogastroenterology, 54 (2007), pp. 503–507
- 3 A.R. Lanfranco, A.E. Castellanos, J.P. Desai, W.C. Meyers; Robotic surgery: a current perspective; Ann Surg., 239 (2004), pp. 14–21
- 4 N.K. Alizai, M.J. Dawrant, A.S. Najmaldin; Robot-assisted resection of choledochal cysts and hepaticojejunostomy in children; Pediatr Surg Int, 30 (2014), pp. 291–294
- 5 M.J. Dawrant, A.S. Najmaldin, N.K. Alizai; Robot-assisted resection of choledochal cysts and hepaticojejunostomy in children less than 10 kg; J Pediatr Surg, 45 (2010), pp. 2364–2368
- 6 T. Akaraviputh, A. Trakarnsanga, N. Suksamanapun; Robot-assisted complete excision of choledochal cyst type I, hepaticojejunostomy and extracorporeal Roux-en-y anastomosis: a case report and review literature; World J Surg Oncol, 8 (2010), p. 87
- 7 C.M. Kang, H.S. Chi, J.Y. Kim, et al.; A case of robot-assisted excision of choledochal cyst, hepaticojejunostomy, and extracorporeal Roux-en-y anastomosis using the da Vinci surgical system; Surg Laparosc Endosc Percutan Tech, 17 (2007), pp. 538–541
- 8 R. Woo, D. Le, C.T. Albanese, S.S. Kim; Robot-assisted laparoscopic resection of a type I choledochal cyst in a child; J Laparoendosc Adv Surg Tech A, 16 (2006), pp. 179–183
- 9 E.C. Lai, C.N. Tang, G.P. Yang, M.K. Li; Approach to manage the complications of choledochoduodenostomy: robot-assisted laparoscopic Roux-en-Y hepaticojejunostomy; Surg Laparosc Endosc Percutan Tech, 21 (2011), pp. e228–231
- 10 E.C. Lai, G.P. Yang, C.N. Tang; Robot-assisted laparoscopic pancreaticoduodenectomy versus open pancreaticoduodenectomy–a comparative study; Int J Surg, 10 (2012), pp. 475–479
- 11 E.C. Lai, C.N. Tang; Current status of robot-assisted laparoscopic pancreaticoduodenectomy and distal pancreatectomy: a comprehensive review; Asian J Endosc Surg, 6 (2013), pp. 158–164
- 12 S. Chalikonda, J.R. Aguilar-Saavedra, R.M. Walsh; Laparoscopic robotic-assisted pancreaticoduodenectomy: a case-matched comparison with open resection; Surg Endosc, 26 (2012), pp. 2397–2402
- 13 J.P. Ruurda, K.W. van Dongen, J. Dries, I.H. Borel Rinkes, I.A. Broeders; Robot-assisted laparoscopic choledochojejunostomy; Surg Endosc, 17 (2003), pp. 1937–1942
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?