Abstract
Background
Regeneration of R-wave or disappearance of Q-wave sometimes occurs after myocardial infarction (MI) especially in the coronary intervention era. We assessed the impact of poor R-wave progression (PRWP) or residual R-wave in precordial leads on myocardial infarct size in patients with prior anterior MI treated with coronary intervention.
Methods
Fifty-three patients with prior anterior MI and 20 age- and sex-matched patients without underwent electrocardiogram (ECG), myocardial perfusion single photon emission tomography (SPECT) and echocardiography. Poor R-wave progression (PRWP) was defined as RV3 ≤ 3 mm.
Results
R-wave was significantly lower in all precordial leads in patients with prior anterior MI than those without. Among 53 patients with prior anterior MI, 33 patients had PRWP, and the remaining 20 patients did not. Patients with PRWP had larger sum of defect score (17.5 ± 8.6 vs 7.6 ± 10.3, p < 0.001) and lower left ventricular ejection fraction (LVEF) (46.1 ± 9.8% vs 55.2 ± 12.9%, p < 0.01) than those without. The sum of R-wave in lead V1 to V6 inversely correlated with the sum of defect score (r = − 0.56, p < 0.001), and positively correlated with LVEF (r = 0.45, p < 0.001).
Conclusion
Our data suggested that residual R-wave during the follow-up period reflected myocardial infarct size and left ventricular systolic function well in patients with prior anterior MI treated with coronary intervention.
Keyword
Electrocardiogram;Defect score;Poor R progression
1. Introduction
The role of 12-lead electrocardiogram (ECG) in diagnosing myocardial infarction (MI) is well established [1], and poor R-wave progression (PRWP) is interpreted as the probable anterior MI [2] ; [3]. However, regeneration of R-wave or disappearance of Q-wave sometimes occurs after MI especially in the coronary intervention era [4]; [5]; [6]; [7] ; [8]. This phenomenon can cancel PRWP, and conceal the ECG phenotype even in patients with definitive anterior MI. Therefore, it is of great interest to evaluate the association between residual R-wave in precordial leads and myocardial infarct size after anterior MI in the coronary intervention era.
In the current study, we assessed the impact of PRWP or residual R-wave in precordial leads on myocardial infarct size in patients with prior anterior MI treated with coronary intervention by using myocardial perfusion single photon emission computed tomography (SPECT).
2. Methods
2.1. Patients
The study population consisted of 53 patients with prior anterior MI beyond at least more than 6 months after the onset and 20 age- and sex-matched patients without. Anterior MI was diagnosed by chest pain consistent with ongoing myocardial ischemia for more than 30 min, elevation of serum creatine kinase to more than twice the normal upper limit and a culprit lesion of the proximal left anterior descending artery on angiography [9]. All patients underwent stent deployment during early period, and underwent ECG, myocardial perfusion SPECT and echocardiography beyond at least more than 6 months after MI. Patients with ventricular pacing or bundle branch block on ECG, myocardial ischemia on myocardial perfusion SPECT and left ventricular hypertrophy on echocardiography were excluded in this study because these factors could influence R-wave in precordial leads.
2.2. Electrocardiogram
A 12-lead ECG was obtained at the time of myocardial perfusion SPECT. ECG was recorded at a paper speed of 25 mm/s and an amplification of 10 mm/mV. The sum of R-wave in lead V1 to V6 was measured in each patient. PRWP was defined as RV3 ≤ 3 mm according to the DePace criteria [3].
2.3. Myocardial perfusion SPECT
All patients fasted overnight, and underwent myocardial perfusion SPECT. Adenosine was infused over 6 min (120 μg/kg/min), and Tl-201 (111 MBq [3.0 mCi]) was injected 3 min after the initiation of adenosine infusion. The stress Tl-201 SPECT acquisition was started 5 min after the stress test. Four hours later, rest Tl-201 SPECT images were also obtained. ECG-gated myocardial perfusion images were acquired with a dual-detector 90° γ-camera (E.CAM; Siemens Medical Solutions). Images were acquired with the following parameters: 32 total projections; 180° from right anterior oblique to left posterior oblique and a noncircular orbit; 64 × 64 matrix; 0.6-cm pixel size; 8 frames per cardiac cycle; low-energy, high-resolution collimation; and 40 s per stop. Tl-201 SPECT images were acquired with a 10% symmetric window over the 80-keV Tl-201 photopeak. Filtered backprojection with a Butterworth prefilter (order, 5; cutoff frequency, 0.65 cycles/pixel for rest and stress images) and decay correction were used for reconstruction. No scatter or attenuation correction was applied. Automated quantification of myocardial perfusion was performed using Quantitative Perfusion SPECT (QPS; version 7.2) (Cedars-Sinai Medical Center, USA) [10]. The sum of defect score was automatically calculated on rest Tl-201 SPECT with QPS using normal database developed for Japanese patients.
2.4. Echocardiography
Echocardiographic studies were performed in a supine left lateral decubitus position. Interventricular septal thickness, posterior wall thickness and left ventricular internal dimension were measured at end-diastole according to established standards of the American Society of Echocardiography. Left ventricular ejection fraction (LVEF) was obtained using a modified biplane Simpsons method from the apical 2- and 4-chamber views.
2.5. Statistical analysis
Statistical analysis was performed with chi-square and Students t-tests. The association between the sum of R-wave in lead V1 to V6 and the sum of defect score and the association between the sum of R-wave in lead V1 to V6 and LVEF were determined by linear regression analysis. All data are expressed as mean ± SD. Differences were considered significant if the p value was < 0.05.
3. Results
3.1. Clinical characteristics
Clinical characteristics of 53 patients with prior anterior MI and 20 patients without are shown in Table 1. There was no significant difference in age, gender, diabetes or hypertension. Patients with prior anterior MI had higher hemoglobin A1C than those without (6.30 ± 1.05% vs 5.89 ± 0.52%, p < 0.01). R-wave was significantly lower in all precordial leads in patients with prior anterior MI than those without. Consequently, the sum of R-wave in lead V1 to V6 was significantly lower in patients with prior anterior MI than those without (34.5 ± 21.2 mm vs 67.3 ± 15.9 mm, p < 0.001). In patients with prior anterior MI, the sum of defect score ranged from 0 to 46 with a mean value of 13.8 ± 10.4. Left ventricular ejection fraction (LVEF) was significantly lower in patients with prior anterior MI than those without (49.5 ± 11.8% vs 64.0 ± 4.6%, p < 0.001).
| Patients with prior anterior MI (n = 53) | Patients without prior anterior MI (n = 20) | p value | |
|---|---|---|---|
| Age (years) | 71.3 ± 8.6 | 71.5 ± 5.5 | ns |
| Male gender | 37 (70%) | 14 (70%) | ns |
| Diabetes | 23 (43%) | 5 (25%) | ns |
| Hypertension | 40 (75%) | 11 (55%) | ns |
| Low-density lipoprotein cholesterol (mg/dl) | 82.7 ± 26.6 | 93.4 ± 38.5 | ns |
| High-density lipoprotein cholesterol (mg/dl) | 56.9 ± 13.2 | 64.8 ± 15.6 | ns |
| Triglyceride (mg/dl) | 125.3 ± 97.9 | 115.9 ± 51.9 | ns |
| Serum creatinine (mg/dl) | 1.00 ± 0.35 | 0.85 ± 0.29 | ns |
| Hemoglobin A1C | 6.30 ± 1.05 | 5.89 ± 0.52 | < 0.01 |
| Electrocardiographic variables | |||
| R wave in lead V1 (mm) | 1.0 ± 1.9 | 2.6 ± 2.1 | < 0.001 |
| R wave in lead V2 (mm) | 1.9 ± 3.0 | 7.2 ± 4.2 | < 0.001 |
| R wave in lead V3 (mm) | 3.5 ± 4.5 | 10.3 ± 3.4 | < 0.001 |
| R wave in lead V4 (mm) | 7.8 ± 7.1 | 17.6 ± 5.2 | < 0.001 |
| R wave in lead V5 (mm) | 11.0 ± 6.1 | 17.9 ± 4.9 | < 0.001 |
| R wave in lead V6 (mm) | 9.2 ± 4.5 | 12.0 ± 4.7 | < 0.05 |
| Sum of R wave in lead V1 to V6 (mm) | 34.5 ± 21.2 | 67.3 ± 15.9 | < 0.001 |
| Poor R-wave progression | 33 (62%) | 0 (0%) | < 0.001 |
| SPECT variable | |||
| Sum of defect score | 13.8 ± 10.4 | 0 ± 0 | < 0.001 |
| Echocardiographic variables | |||
| Left ventricular internal dimension (mm) | 53.3 ± 7.2 | 47.2 ± 3.8 | < 0.01 |
| Interventricular septal thickness (mm) | 8.2 ± 1.9 | 8.9 ± 1.7 | ns |
| Posterior wall thickness (mm) | 9.3 ± 1.4 | 9.2 ± 1.3 | ns |
| Left ventricular ejection fraction (%) | 49.5 ± 11.8 | 64.0 ± 4.6 | < 0.001 |
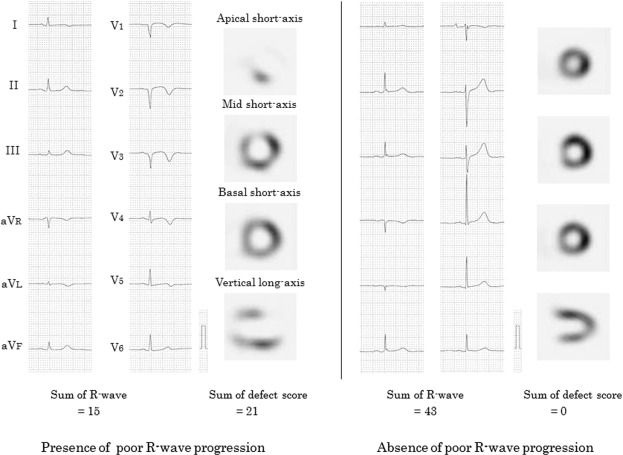
3.2. Poor R-wave progression and infarct size
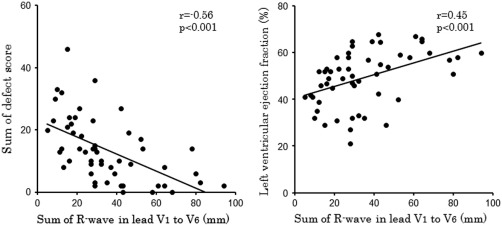
Among 53 patients with prior anterior MI, 33 patients had PRWP, and the remaining 20 patients did not (Table 2). ECG and SPECT images in cases of the presence or absence of PRWP are shown in Fig. 1. Patients with PRWP had larger sum of defect score (17.5 ± 8.6 vs 7.6 ± 10.3, p < 0.001) and lower LVEF (46.1 ± 9.8% vs 55.2 ± 12.9%, p < 0.01) than those without. The sum of R-wave in lead V1 to V6 inversely correlated with the sum of defect score (r = − 0.56, p < 0.001), and positively correlated with left ventricular ejection fraction (r = 0.45, p < 0.001) (Fig. 2).
| Patients with poor R-wave progression (n = 33) | Patients without poor R-wave progression (n = 20) | p value | |
|---|---|---|---|
| Age (years) | 71.8 ± 7.4 | 70.7 ± 10.5 | ns |
| Male gender | 26 (79%) | 11 (55%) | ns |
| Diabetes | 14 (42%) | 5 (25%) | ns |
| Hypertension | 25 (76%) | 11 (55%) | ns |
| Electrocardiographic variables | |||
| R wave in lead V1 (mm) | 0.3 ± 0.6 | 2.6 ± 2.7 | < 0.01 |
| R wave in lead V2 (mm) | 0.4 ± 0.8 | 4.4 ± 3.5 | < 0.001 |
| R wave in lead V3 (mm) | 0.7 ± 1.0 | 8.2 ± 4.1 | < 0.001 |
| R wave in lead V4 (mm) | 4.2 ± 3.4 | 13.9 ± 7.7 | < 0.001 |
| R wave in lead V5 (mm) | 9.4 ± 5.2 | 13.7 ± 6.7 | < 0.05 |
| R wave in lead V6 (mm) | 9.1 ± 4.5 | 9.5 ± 4.5 | ns |
| Sum of R wave in lead V1 to V6 (mm) | 24.2 ± 12.2 | 51.6 ± 22.0 | < 0.001 |
| SPECT variable | |||
| Sum of defect score | 17.5 ± 8.6 | 7.6 ± 10.3 | < 0.001 |
| Echocardiographic variables | |||
| Left ventricular internal dimension (mm) | 55.3 ± 6.9 | 50.0 ± 6.5 | < 0.001 |
| Interventricular septal thickness (mm) | 8.0 ± 2.2 | 8.7 ± 1.2 | ns |
| Posterior wall thickness (mm) | 9.6 ± 1.4 | 8.7 ± 1.4 | ns |
| Left ventricular ejection fraction (%) | 46.1 ± 9.8 | 55.2 ± 12.9 | < 0.01 |
|
|
|
Fig. 1. Electrocardiogram and SPECT images in cases of the presence or absence of poor R-wave progression. |
|
|
|
Fig. 2. The sum of R-wave in lead V1 to V6 inversely correlated with the sum of defect score (r = − 0.56, p < 0.001) (left panel), and positively correlated with left ventricular ejection fraction (r = 0.45, p < 0.001) (right panel). |
4. Discussion
In this study, we demonstrated the following: 1) R-wave was significantly lower in all precordial leads in patients with prior anterior MI than those without; 2) in patients with prior anterior MI, PRWP reflected large myocardial infarct size and severely impaired left ventricular systolic function; and 3) the sum of R-wave in all precordial leads inversely correlated with myocardial infarct size, and positively correlated with left ventricular systolic function.
Clinical outcome of patients after MI depends on myocardial infarct size, the extent of area at risk or the status of myocardial reperfusion, and these factors can be assessed by myocardial perfusion SPECT in detail [11]; [12] ; [13]. In contrast, ECG is a simple and inexpensive examination, and has been widely used for diagnosing MI. Usefulness of ECG in assessing myocardial infarct size has been also reported. The Selvester QRS score is an ECG index of myocardial damage that incorporates not only the number of Q-waves but also decreased R-wave, but this scoring system is complex [1] ; [14]. In the clinical setting, decreased R-wave in precordial leads is interpreted as some myocardial damage after anterior MI based on experiences. Indeed, the current study showed that R-wave was significantly lower in all precordial leads in patients with prior anterior MI than those without. However, little is known about their quantitative correlation. In the current study, we reviewed ECG, myocardial perfusion SPECT and echocardiography in patients with prior anterior MI, and demonstrated that PRWP reflected large infarct size and poor left ventricular systolic function. We also demonstrated that the sum of R-wave in all precordial leads inversely correlated with myocardial infarct size, and positively correlated with left ventricular systolic function.
With the recent advance of coronary intervention, regeneration of R-wave after reperfusion has been recognized [4]; [5] ; [6]. Isobe et al. assessed implications of this phenomenon by using myocardial SPECT, and reported that the increase of R-wave from 1 to 4 weeks was associated with the improvement of LVEF and the discordance on Tl and iodine-123-β-methyl-p-iodophenyl pentadecanoic acid [5]. Because mismatch between perfusion and metabolism indicates the presence of salvaged myocardium in the risk area after MI [15] ; [16], regeneration of R-wave during the early period appears to reflect the presence of reversible myocardium. On the other hand, there has been few reports about the association between finally fixed residual R-wave and myocardial infarct size during the follow-up period. In the current study, we showed that PRWP remained to be an ECG phenotype of large myocardial infarct size even in patients with prior anterior MI treated with coronary intervention, and that the sum of R-wave in all precordial leads reflected myocardial infarct size and left ventricular systolic function well. Physicians should pay careful attention of ECG findings during the follow-up period as well as early period of MI.
There were several limitations in this study. First, this study included only patients with stable condition after anterior MI, and excluded patients with myocardial ischemia which might affect residual R-wave. Second, we did not evaluate myocardial metabolism, and it was unclear whether patients with prior anterior MI had impaired but viable myocardium. However, it was noteworthy that all patients underwent ECG and myocardial perfusion SPECT at least more than 6 months after MI. This interval possibly allows us to assess our purposes. Finally, the small sample size was a major limitation of this study.
In conclusion, our data suggested that residual R-wave during the follow-up period reflected myocardial infarct size and left ventricular systolic function well. Physicians should pay careful attention of ECG findings during the follow-up period as well as early period of MI.
Conflict of interest
The authors report no relationships that could be construed as a conflict of interest.
References
- [1] M. Kosuge, K. Kimura; Clinical implications of electrocardiograms for patients with anterior wall ST-segment elevation acute myocardial infarction in the interventional era; Circ J, 76 (2012), pp. 32–40
- [2] M.J. Zema, P. Kligfield; Electrocardiographic poor R wave progression. I: correlation with the Frank vectorcardiogram; J Electrocardiol, 12 (1979), pp. 3–10
- [3] N.L. DePace, J. Colby, A.H. Hakki, B. Manno, L.N. Horowitz, A.S. Iskandrian; Poor R wave progression in the precordial leads: clinical implications for the diagnosis of myocardial infarction; J Am Coll Cardiol, 2 (1983), pp. 1073–1079
- [4] K.C. Preuss, P.D. Chapman, M.J. Ptacin, M.H. Keelan, V.S. Bamrah; Spontaneous recovery of left ventricular function following acute anterior myocardial infarction; Clin Cardiol, 11 (1988), pp. 497–500
- [5] S. Isobe, M. Okada, A. Ando, M. Nanasato, M. Nonokawa, H. Izawa, et al.; Clinical significance of changes in electrocardiographic R-wave voltage on chest leads in patients with acute anterior myocardial infarction; J Electrocardiol, 35 (2002), pp. 173–180
- [6] S. Isobe, Y. Takada, A. Ando, S. Ohshima, K. Yamada, M. Nanasato, et al.; Increase in electrocardiographic R-waves after revascularization in patients with acute myocardial infarction; Circ J, 70 (2006), pp. 1385–1391
- [7] K. Ishikawa, M. Shimizu, M. Ohno, M. Morishita, I. Ogawa, T. Hayashi, et al.; Clinical significance of abnormal Q wave disappearance in acute transmural myocardial infarction; Jpn Circ J, 55 (1991), pp. 213–220
- [8] K. Iwasaki, S. Kusachi, K. Hina, S. Yamasaki, T. Kita, C. Endo, et al.; Q-wave regression unrelated to patency of infarct-related artery or left ventricular ejection fraction or volume after anterior wall acute myocardial infarction treated with or without reperfusion therapy; Am J Cardiol, 76 (1995), pp. 14–20
- [9] S. Kurisu, I. Inoue, T. Kawagoe, M. Ishihara, Y. Shimatani, T. Hata, et al.; Right bundle-branch block in anterior acute myocardial infarction in the coronary intervention era: acute angiographic findings and prognosis; Int J Cardiol, 116 (2007), pp. 57–61
- [10] Y. Xu, P. Kavanagh, M. Fish, J. Gerlach, A. Ramesh, M. Lemley, et al.; Automated quality control for segmentation of myocardial perfusion SPECT; J Nucl Med, 50 (2009), pp. 1418–1426
- [11] R.J. Gibbons, U.S. Valeti, P.A. Araoz, A.S. Jaffe; The quantification of infarct size; J Am Coll Cardiol, 44 (2004), pp. 1533–1542
- [12] P. Chouraqui, S. Livschitz, J. Baron, I. Moalem, M. Shechter; The assessment of infarct size in postmyocardial infarction patients undergoing thallium-201 tomographic imaging is improved using attenuation correction; Clin Nucl Med, 29 (2004), pp. 352–357
- [13] S. Kurisu, I. Inoue, T. Kawagoe, M. Ishihara, Y. Shimatani, N. Mitsuba, et al.; Spontaneous anterograde flow of the infarct artery preserves myocardial perfusion and fatty acid metabolism in patients with anterior acute myocardial infarction; Circ J, 69 (2005), pp. 427–431
- [14] R.H. Selvester, G.S. Wagner, N.B. Hindman; The Selvester QRS scoring system for estimating myocardial infarct size: the development and application of the system; Arch Intern Med, 145 (1985), pp. 1877–1881
- [15] H. Yamanaka, T. Suzuki, H. Kishida, K. Nagasawa, T. Takano; Relationship between the mismatch of 123I-BMIPP and 201Tl myocardial single-photon emission computed tomography and autonomic nervous system activity in patients with acute myocardial infarction; Int Heart J, 47 (2006), pp. 193–207
- [16] A. Hashimoto, T. Nakata, N. Tamaki, T. Kobayashi, T. Matsuki, T. Shogase, et al.; Serial alterations and prognostic implications of myocardial perfusion and fatty acid metabolism in patients with acute myocardial infarction; Circ J, 70 (2006), pp. 1466–1474
Document information
Published on 19/05/17
Submitted on 19/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?