Highlights
- Here, we are presenting a very rare case of coarctation of abdominal aorta where a transcatheter closure by a vascular plug of the feeding collateral to a large aneurysm has been done. To the best of our knowledge, this mode of therapy has never been described in persons with coarctation of abdominal aorta.
- Aneurysms in patients with an abdominal coarctation are not well recognized. This is probably the only case being reported where transcatheter closure of the feeding vessel to the aneurysm has been successfully performed.
- In this case, aneurysm was closed by a vascular plug only to prevent sudden rupture and death, and no attempt was made for stenting or dilatation of the atretic segment as the segment was long and no direct connection could be noted between upper and lower segments. The incidence of coarctation of the abdominal aorta is rare and the possibility of aneurysms in coarctation of the abdominal aorta is very rare compared to coarctation of the descending thoracic aorta. Thus, this case is being reported in view of the extreme rarity of the problem.
Keywords
Middle aortic syndrome;Takayasus arteritis;Aortic angiography;Vascular plug;Intermittent claudication
1. Introduction
Coarctation of the abdominal aorta (mid-aortic dysplastic syndrome) is a clinical condition caused by segmental narrowing of the abdominal or distal descending thoracic aorta, either a congenital anomaly or associated with neurofibromatosis, retroperitoneal fibrosis, fibromuscular dysplasia, mucopolysaccharidosis, and Takayasus arteritis. Congenital abdominal coarctation usually manifests itself in early adulthood or earlier (average age, 20 years). The upper extremities and thorax may be more developed than the lower extremities in presence of abdominal coarctation.
The abdominal aorta is the site of abnormality in about 2% of patients with coarctation of the aorta. The association of aneurysm formation with an abdominal coarctation is not well recognized, although similar pressures and flow patterns are present in both thoracic and abdominal aortic coarctation. Our search of the literature has revealed only 3 cases with associated aneurysms. This is probably the only case being reported where transcatheter closure of feeding vessel to the aneurysm has been successfully performed.
2. Case history
A 35-year-old female presented with dull aching pain in right loin for the last 3 months. She was diagnosed with hypertension from the age of 16 years and has been on antihypertensives since then. She was able to perform her usual daily household work; however, she was having intermittent claudication in both lower limbs. There was no history of prolonged fever, arthralgia or any neurological symptoms in the past.
On examination, she had mild pallor with average health, both femoral, popliteal, dorsalis pedis and posterior tibial pulses were weak but upper limb pulses and carotids were normal. BP was 200/120 mmHg in both upper limbs and 130/90 mmHg in both lower limbs. Temperature of both lower limbs was normal without any skin ulcers or gangrene. Cardiovascular examination revealed a heaving apical impulse. A prominent systolic bruit was heard in the right lumbar region. Incidentally, she was suffering from TB meningitis and had a poor neurological status.
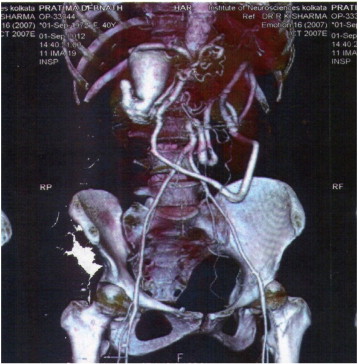
CT angiography showed agenesis of abdominal aorta from origins of renal arteries, abnormal branching of superior mesenteric artery forming vascular loop and reconstituting lower aorta, and large aneurismal dilatation of the distal part of the gastroduodenal artery (Fig. 1).
|
|
|
Fig. 1. CT angiography showing agenesis of abdominal aorta, collaterals reconstituting the lower abdominal aorta and the aneurysm from gastroduodenal artery. |
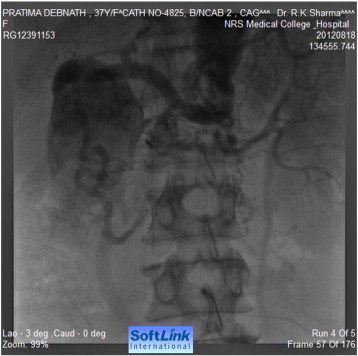
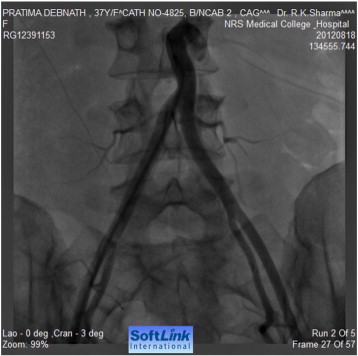
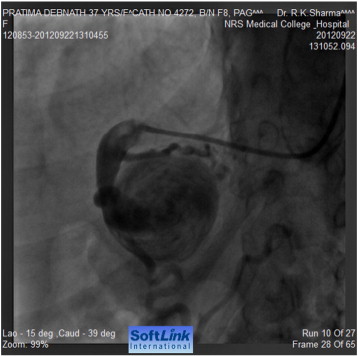
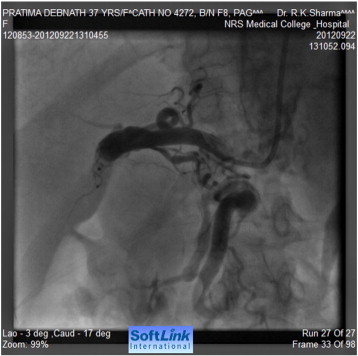
Tran-femoral catheter passage beyond the bifurcation of the abdominal aorta was not possible due to total occlusion and trans-radial aortic angiography showed a long segment of total occlusion (coarctation of abdominal aorta) just below the origin of both renal arteries, multiple dilated collaterals connecting both upper and lower aortic segments with a huge aneurysm involving gastroduodenal artery (Fig. 2, Fig. 3 ; Fig. 4). Lower thoracic aorta was calcified and arch vessels origins and proximal aorta were normal. The blood pressure within the aneurysm was 190/110 mmHg (Fig. 5).
|
|
|
Fig. 2. Aortography showing interruption of abdominal aorta below the origin of renal arteries. |
|
|
|
Fig. 3. Abdominal aorta after the coarctation segment and iliac arteries. |
|
|
|
Fig. 4. Selective angiography of feeding vessel to aneurysm via a right Judlins catheter. |
|
|
|
Fig. 5. Selective injection into the aneurysm. |
As the patient was having nagging pain at the site of aneurysm, there was a risk of rupture of the aneurysm. As she had a very high surgical risk because of high BP, poor general health and risk of renal compromise; transcatheter closure of aneurysm was planned. An Amplatzer Vascular Plug II was deployed in the distal end of the feeding collateral branch of the gastroduodenal artery through right brachial artery and the aneurysm was successfully closed (Fig. 6 ; Fig. 7). Since then, the loin pain disappeared and surgical revascularization by aorto-iliac or aorto-femoral bypass grafting is being considered for relief of lower limb ischemic symptoms.
|
|
|
Fig. 6. Plug inserted. |
|
|
|
Fig. 7. Successful closure of the feeding vessel. |
Coarctation of the abdominal aorta, also known as middle aortic syndrome or mid-aortic dysplastic syndrome, is a clinical condition caused by segmental narrowing of the abdominal or distal descending thoracic aorta secondary either to a congenital anomaly in the development of the abdominal aorta or to one of several acquired conditions. Acquired conditions include neurofibromatosis, retroperitoneal fibrosis, fibromuscular dysplasia, mucopolysaccharidosis, and Takayasus arteritis, all of which may result in narrowing of the abdominal aorta and other vessels [1] ; [2].
First described by Schlesinger and Quain, congenital abdominal coarctation usually manifests itself in early adulthood or earlier (average age, 20 years), although any age may be represented [3] ; [4]. The upper extremities and thorax may be notably more developed than the lower extremities in the presence of abdominal coarctation or coarctation of descending thoracic aorta [3].
The abdominal aorta is the site of abnormality in about 2% of patients with coarctation of the aorta [5]. One hundred ten cases of abdominal coarctation had been reported in the literature as of 1973 [6]. D'Abreu and his associates [3] classified abdominal coarctation into segmental and hypoplastic types; these have been further subdivided in relation to the position of the renal arteries.
Physical signs include cardiac murmurs, mid systolic abdominal bruits, and continuous bruits from the collateral vessels auscultated in the left loin, the back, and the thorax [7] ; [8], and collateral arteries palpable in the territory of the superior and inferior superficial epigastric arteries [8] ; [9]. Enlarged collateral vessels may be palpated in the intercostals spaces anteriorly; the axilla, and the interscapular area posteriorly [9] ; [10]. Symptoms include leg weakness and pain on exercise, typical of intermittent claudication [7] ; [8]. Uncontrolled hypertension may cause occipital headache, worse when the patient wakes up in the morning and subsides later in the day [7] ; [8]. Dizziness, palpitations, fatigability, epistaxis, blurred vision, and cerebrovascular and cardiac events may also occur [9] ; [10]. Because the proximal portions of the renal arteries are involved in as many as 80% of cases of abdominal coarctation [9], symptoms secondary to renal function impairment may be found [7] ; [8]. Very occasionally, orificial stenosis of the mesenteric arteries (celiac and superior mesenteric artery) may result in gastrointestinal complaints secondary to chronic bowel ischemia [9] ; [10].
The association of aneurysms with thoracic aorta coarctation is well recognized and has been reviewed by Skandalakis and his associates [11]. Of 1,091 patients with thoracic coarctation, 102 had an associated aneurysm or aneurysms. In most, the aneurysms were located in the aorta proximal or distal to the stenotic segment. The intercostal arteries were less commonly involved. Multiple aneurysms were present in 13% of the patients, and 10% of the aneurysms were calcified. Sixty-three of the 102 patients were examined postmortem; the cause of death in 41 was rupture of the aneurysm [3]. Thus, the presence of an aneurysm represents a serious risk to the patient.
The association of aneurysm formation with an abdominal coarctation is not well recognized, although similar pressures and flow patterns are present in both thoracic and abdominal aortic coarctation. Our search of the literature has revealed 3 cases with associated aneurysms.
Skandalakis and his colleagues [11] summarized, “Since less than 30% (of aneurysms) were of mycotic origin, none were syphilitic and few could be attributed to hypertension per se, the majority of aneurysms associated with coarctation must be explained as being due to some other intrinsic factor.” Three factors appear to be of importance: 1) congenital weakness of the aortic wall associated with luminal hypoplasia; 2) abnormal flow patterns and eddy currents in and around the narrowed aortic segment; and 3) hypertension.
Balloon angioplasty has been used for at least 20 years in the treatment of middle aortic syndrome [12]. Successful stent implantation by Ledesma et al. [13] was achieved in 53 (98%) of 54 patients aged 8 to 49 years with aortic coarctation in the thoracic aorta and a mean pressure gradient of 50 ± 20 mm Hg across the lesion. The procedure was performed with minimal morbidity and no mortality. Clinical success, defined as a peak-to-peak pressure gradient of 20 mm Hg or less, was achieved in 52 (96%) of 54 patients, with 29 having no pressure gradient after stent deployment. All patients had localized aortic coarctation except one who had a long tubular stenosis.
Dilatation of the stenosed aortic segments with balloon angioplasty and balloon-expandable endovascular stents was proven effective in the short- to mid-term by D'Souza et al. [14] in three pediatric patients with abdominal aortic coarctation, of whom two had concomitant bilateral renal artery stenosis.
In this case, aneurysm was closed by a vascular plug to prevent sudden rupture and death, no attempt was made for stenting or dilatation of the atretic segment as the segment was long and no direct connection could be noted between upper and lower segments. The proximal part of the aorta was also grossly calcified and stretching the aorta would carry a very high risk of tearing of the aorta. Surgical repair by aorto-iliac or aorto-femoral bypass grafting remains the only option and would be attempted shortly. The incidence of coarctation of the abdominal aorta is rare and the possibility of aneurysms in coarctation of the abdominal aorta is very rare compared to coarctation of the descending thoracic aorta. Thus, this case is being reported in view of the extreme rarity of the problem. To the best of our knowledge, endovascular plug implantation for the prevention of rupture of a large aneurysm in middle aortic syndrome has not been reported so far.
Coarctation of the abdominal aorta must be considered in young hypertensive patients. Weak to absent femoral pulses provide the first clue to the diagnosis. The appearance of a normal aortic arch and the absence of notching of the third through eighth ribs, especially when combined with an abdominal bruit, provide indications for preoperative aortography to establish the site and precise type of coarctation. Associated aneurysms may be found. Operative therapy must include bypass of the obstructed aorta and its branches to relieve the hypertension as well as resection of any associated aneurysms to prevent subsequent rupture.
The risk of rupture of aneurysms in coarctation of aorta is high because a majority of these persons have severe uncontrolled hypertension. If there are features of impending rupture of any aneurysm, then endovascular therapy can be safely and effectively provided.
Conflict of interest
The authors declare that there is no conflict of interest and no financial grant has been taken from any organisation.
References
- [1] K.T. Delis, P. Gloviczki; Middle aortic syndrome: from presentation to contemporary open surgical and endovascular treatment; Perspect Vasc Surg Endovasc Ther, 17 (2005), pp. 187–203
- [2] J.E. Connolly, S.E. Wilson, P.L. Lawrence, R.M. Fujitani; Middle aortic syndrome: distal thoracic and abdominal coarctation: a disorder with multiple etiologies; J Am Coll Surg, 194 (2002), pp. 774–781
- [3] A.L. D'Abreu, C.G. Rob, J.F. Vollmar; Die coarctation aortae abdominalis; Langenbecks Arch Klin Chir, 290 (1959), p. 521
- [4] L.K.M. Graham, G.B. Zelenock, E.E. Erlandson, et al.; Abdominal aortic coarctation and segmental hypoplasia; Surgery, 86 (1979), pp. 519–529
- [5] J.R. Cohen, E. Birnbaum; Coarctation of the abdominal aorta; J Vasc Surg, 8 (1988), pp. 160–164
- [6] M. Ben-Shoshan, N.P. Rossi, M.E. Karns; Coarctation of the abdominal aorta; Arch Pathol, 95 (1973), p. 221
- [7] S. Kaplan; Congenital heart disease; J.B. Wyngaarden, L.H. Smith Jr. (Eds.), Cecil Textbook of Medicine, W.B. Saunders Company, Philadelphia (1988), pp. 303–318
- [8] W.F. Friedman; Congenital heart disease; R.G. Petersdorf, R.D. Adams, E. Braunwald (Eds.), et al., Harisons Principles of Internal Medicine, McGraw-Hill International, Aukland (1984), pp. 1383–1397
- [9] T.W. Rooke, J.W. Joyce; Uncommon arteriopathies; R.B. Rutherford (Ed.), Vascular Surgery, W.B. Saunders Company, Philadelphia (2000), pp. 418–434
- [10] R.D. Patman, W.P. Shutze; Non-atherosclerotic vascular diseases and conditions; R.H. Dean, J.S.T. Yao, D.C. Brewster (Eds.), Current Diagnosis and Treatment in Vascular Surgery, Prentice Hall International, London (1995), pp. 172–192
- [11] J.E. Skandalakis, B.F. Edwards, S.W. Gray, B.M. Davis, W.A. Hopkins; Coarctation of the aorta with aneurysm; Znt Abstr Surg, 11 1 (1960), p. 307
- [12] S. Adwani, J.V. De Giovanni; Percutaneous transluminal balloon angioplasty of abdominal aortic coarctation in an infant; Pediatr Cardiol, 17 (1996), pp. 346–348
- [13] M. Ledesma, C. Alva, F.D. Gomez, et al.; Results of stenting for aortic coarctation; Am J Cardiol, 88 (2001), pp. 460–462
- [14] S.J. D'Souza, W.S. Tsai, M.M. Silver, et al.; Diagnosis and management of stenotic aorto-arteriopathy in childhood; J Pediatr, 132 (1998), pp. 1016–1022
Document information
Published on 19/05/17
Submitted on 19/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?