Summary
Background/objective
Laparoscopic gastrectomy (LG) is increasingly used to treat gastric cancer. Simultaneously, internal hernia (IH) has been reported after LG with Roux-en-Y reconstruction (RY). The aim of this study was to investigate IH after LG with RY for gastric cancer.
Methods
This study included 15 patients with IH from a database of 355 consecutive patients who underwent LG with RY for gastric cancers. We retrospectively analyzed IH incidence and clinical characteristics by operative procedures.
Results
The total incidence of IH was 4.2%. The incidence of IH at Petersens defect tended to decrease with modifications to the reconstruction methods, but not significantly so. The incidence of IH at jejunojejunostomy mesenteric defect significantly decreased with closure of this defect (p = 0.01). The incidence of IH at transverse mesocolic defect was 1.3% in patients who underwent retrocolic RY; emergent small-bowel resection was only required in two cases of herniation through this defect after laparoscopic total gastrectomy.
Conclusion
Retrocolic RY with appropriate closure of defects can reduce IH incidence at Petersens defect and at jejunojejunostomy mesenteric defect. Although the IH incidence at the transverse mesocolic defect is not particularly high, the possibility of herniation through this defect should be kept in mind.
Keywords
gastric cancer;internal hernia;laparoscopic gastrectomy;Roux-en-Y reconstruction
1. Introduction
In Japan, gastric cancer is the second most common cause of cancer death.1 Laparoscopic gastrectomy (LG) has been widely adopted as a treatment option, not only because it is less invasive and offers better cosmetic outcomes, but also because it enables the rapid recovery of intestinal movement and facilitates accurate lymph-node dissection through magnified viewing.2 Simultaneously, internal hernia (IH) has been reported as a cause of postoperative small-bowel obstruction after LG, particularly after Roux-en-Y reconstruction (RY); in contrast, more adhesions are observed after open gastrectomies.3; 4; 5; 6 ; 7 IH is a well-known postoperative complication of laparoscopic Roux-en-Y gastric bypass (LRYGB). The use of the antecolic antegastric route or closure of mesenteric defects is widely reported to reduce IH after LRYGB,8; 9; 10; 11; 12; 13 ; 14 as is the use of proper techniques, such as avoiding mesenteric division and ensuring appropriate orientation of the alimentary limb.15 Excess weight loss has been reported as a cause of IH.16
Unfortunately, IH is difficult to diagnose because its associated symptoms are rather nonspecific, and the imaging modalities used in its diagnosis are inadequately sensitive; however, it can be life threatening.16; 17 ; 18 Whereas LRYGB and LG with RY have some differences (such as postoperative construction of the supracolic component and preoperative obesity with LRYGB), few reports have addressed IH after LG with RY. This study aimed to clarify the characteristics of IH after LG for gastric cancer.
2. Methods
2.1. Patients
This was an observational, historical cohort study. We analyzed patients from a database of 355 consecutive patients who underwent LG with RY for gastric cancers at the Department of Surgery, Japan Community Health care Organization, Kyushu Hospital between April 2006 and April 2012. Laparoscopic gastrectomies were indicated for all patients regardless of the clinical stages of their cancers, when an informed consent was obtained. These patients consisted of 257 who underwent laparoscopic distal gastrectomy (LDG) and 98 who underwent laparoscopic total gastrectomy (LTG). Postoperative staging was performed according to the tumor–node–metastasis staging system.19 Early gastric cancer was defined as cancer invading the mucosa or submucosa, with or without lymph-node metastasis.20
2.2. Operative procedures for RY
Table 1 shows the changes in RY procedures over time at our institution. We performed antecolic RY without closure of Petersens defect, which is found at the back side of the Roux limb or of the jejunojejunostomy mesenteric defect until March 2009 (first period). In April 2009, because of increasing IH occurrence, we changed our standard technique to retrocolic RY with closure of the jejunojejunostomy mesenteric defect (second period). Since April 2011, we have also closed Petersens defect (third period). The transverse mesocolic defect was also closed by fixing the gastrojejunostomy site (LDG) or jejunum (LTG) to it in all patients who underwent retrocolic RY. All defects were closed with 4-0 absorbable intermittent sutures. To bring up the Roux limb, approximately 5 cm of the small bowel was sacrificed in LDG, and 20 cm in LTG, instead of dividing the mesentery. Both gastrojejunostomy (LDG) and esophagojejunostomy (LTG) were performed using linear staplers under pneumoperitoneum; the jejunojejunostomy was fashioned using hand sutures through the minilaparotomy or linear staplers under pneumoperitoneum in all cases.
| Period | Number of patients | Route of Roux limb | Closure of Petersen | Closure of JJ | Closure of T-colon |
|---|---|---|---|---|---|
| First period | 119 | Antecolic | No | No | — |
| 30 | Retrocolic | No | No | Yes | |
| Second period | 3 | Antecolic | No | Yes | — |
| 98 | Retrocolic | No | Yes | Yes | |
| Third period | 105 | Retrocolic | Yes | Yes | Yes |
First period: April 2006–March 2009; second period: April 2009–March 2011; third period: April 2011–April 2012.
JJ = jejunojejunostomy mesenteric defect; Petersen = Petersens defect; T-colon = transverse mesocolic defect.
2.3. Clinicopathological variables
We collected the following clinicopathological data for patients who developed IH: age, sex, cancer stage, degree of lymph-node dissection, operative time, intraoperative bleeding, body mass index (BMI) at LG, interval between LG and IH, symptoms, presence of acute pancreatitis, bowel resection during emergent surgery for IH, and death. These variables were compared between patients who underwent antecolic RY (antecolic group) and patients who underwent retrocolic RY (retrocolic group).
2.4. Statistical analysis
A statistical analysis was performed using the JMP statistical software (version 9.0.2; SAS Institute, Cary, NC, USA). Fishers exact probability test or the Chi-square test was used to evaluate differences in clinical factors between the two groups. The Mann–Whitney U test was used for continuous data. A p value < 0.05 was considered to be significant.
3. Results
3.1. Incidence of IH
Fifteen patients developed IH after LG with RY. The incidence of IH after LG with RY was 4.2% (15/355). IH was not detected in patients who underwent other types of LG, such as LDG with Billroth I or laparoscopic proximal gastrectomy. Eleven of the 15 patients underwent LG in the first period, three in the second period, and one in the third period. IH occurred at Petersens defect in seven patients, the jejunojejunostomy mesenteric defect in five, and the transverse mesocolic defect in three.
Table 2 shows the incidence of IH at Petersens defect by operative procedure. While IH at Petersens defect was observed in 5 of 122 patients (4.1%) who underwent antecolic RY without closure of the defect, IH was observed in only 2 of 128 patients (1.6%) who underwent retrocolic RY without defect closure (p = 0.27). Moreover, the incidence did not significantly differ even when patients who underwent antecolic RY without closure of Petersens defect were compared with those who underwent retrocolic RY with defect closure (p = 0.06).
| Route of Roux limb | Closure of Petersen | Number of patients | Internal hernia (%) | p |
|---|---|---|---|---|
| Antecolic | No | 122 | 5 (4.1) | |
| Retrocolic | No | 128 | 2 (1.6) | |
| Retrocolic | Yes | 105 | 0 (0) |
Petersen = Petersens defect.
Unlike Petersens defect, there is no anatomic difference in the jejunojejunostomy mesenteric defect between antecolic and retrocolic RY. Table 3 shows the incidence of IH in association with closure; IH was observed in 5 of 149 patients (3.4%) without closure, while no IHs were observed in the 206 patients with closure (p = 0.01).
| Closure of JJ | Number of patients | Internal hernia (%) | p |
|---|---|---|---|
| No | 149 | 5 (3.4) | 0.01 |
| Yes | 206 | 0 (0) |
JJ = jejunojejunostomy mesenteric defect.
Finally, IH at the transverse mesocolic defect is unique to retrocolic RY, and 3 of 233 patients (1.3%, Table 4) who underwent retrocolic RY developed IHs. Two of the three patients had undergone LTG, and the remaining patient had undergone LDG.
| Closure of T-colon | Number of patients | Internal hernia (%) |
|---|---|---|
| Yes | 233 | 3 (1.3) |
T-colon = transverse mesocolic defect.
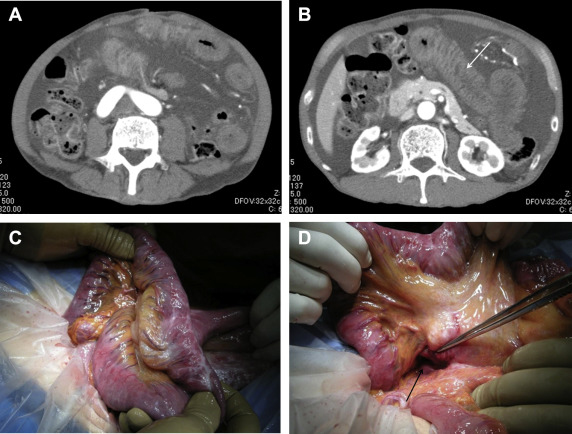
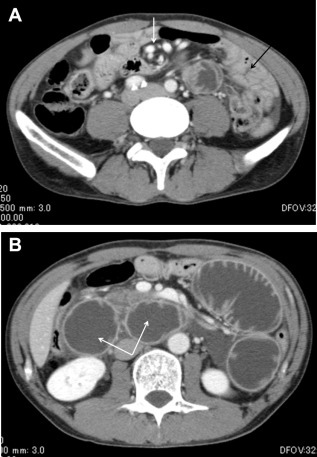
3.2. Clinical features of IH
Table 5 shows a comparison of the clinical features of IH between patients who underwent antecolic versus retrocolic RY. These variables (patient age, sex, cancer stage, degree of lymph-node dissection, operative time, intraoperative bleeding, and BMI at LG) did not significantly differ between the two groups. The median interval between LG and IH was 36.1 months (range 15.5–92.2 mo) in the antecolic group, and 8.4 months (range 0.2–28.9 mo) in the retrocolic group (p < 0.01). The most common symptom in our study was abdominal pain, which was observed in 14 of the 15 patients; three patients suffered repeated abdominal pain until the diagnosis of IH. The remaining patient experienced repeated, massive ascites three times without any other symptoms ( Figure 1). Because this ascites disappeared without treatment within a few days, the IH responsible for the ascites was missed by an outside hospital during the first two events despite other imaging findings, such as whirl sign, biliopancreatic limb dilatation, and localization of the bowels to the left upper quadrant on computed tomography (Figure 2). Also, 3 of the 15 patients (all of whom had undergone antecolic RY) had histories of acute pancreatitis due to biliopancreatic limb obstruction.
| Variable | Antecolic RY (n = 9) | Retrocolic RY (n = 6) | p |
|---|---|---|---|
| Age (y)a | 68 (42–78) | 70.5 (62–77) | 0.41 |
| Sex (male/female) | 8/1 | 6/0 | 1.00 |
| Stage (early/advanced) | 6/3 | 4/2 | 1.00 |
| Lymph-node dissection | 0.60 | ||
| D1+ | 6 | 5 | |
| D2 | 3 | 1 | |
| Operative time (min)a | 310 (234–567) | 418.5 (307–520) | 0.06 |
| Intraoperative bleeding (mL)a | 50 (5–190) | 65 (0–520) | 0.95 |
| Body mass index at gastrectomy (kg/m2)a | 22.3 (19.5–24.1) | 22.1 (21.3–24.6) | 0.81 |
| Interval between gastrectomy and IH (mo)a | 36.1 (15.5–92.2) | 8.4 (0.2–28.9) | <0.01 |
| Symptom | 1.00 | ||
| Abdominal pain | 8 | 6 | |
| Massive ascites | 1 | 0 | |
| Acute pancreatitis | 3 | 0 | 0.23 |
| Bowel resection in the operation for IH | 0 | 2 | 0.14 |
| Death | 2 | 1 | 1.00 |
IH = internal hernia; LDG = laparoscopic distal gastrectomy; LTG = laparoscopic total gastrectomy; RY = Roux-en-Y reconstruction.
a. Data reported as median (range).
|
|
|
Figure 1. Abdominal enhanced computed tomography showed (A) significant ascites and (B, arrow) an edematous Roux limb. Both findings had been seen previously (2 mo before and again 2 wk before the episode shown), but had temporarily vanished without any treatment. (C) Operative findings revealed an edematous Roux limb, which was not ischemic. Ascites had been induced by the obstruction of mesenteric venous return. (D) The small bowel had passed through Petersens defect (arrow) from the right side to the left side. |
|
|
|
Figure 2. (A) Abdominal enhanced computed tomography showed a whirl sign (white arrow) and localization of the small bowel to the left upper quadrant (black arrow). (B) Abdominal enhanced computed tomography revealed a dilated biliopancreatic limb (arrows), which induced pancreatitis. |
Small-bowel resection could not be avoided in two patients, both of whom had developed IH at the transverse mesocolic defect after LTG with retrocolic RY. One of the two patients died from disseminated intravascular coagulation after the emergency resection. There were two other deaths in this study. One patient died from cancer. Another patient, who originally developed an IH at the jejunojejunostomy mesenteric defect following antecolic RY, experienced subsequent recurrence of the IH at Petersons defect, despite previous closure of this defect in addition to the jejunojejunostomy mesenteric defect during emergency surgery for the first IH. This patient suffered ileus, acute pancreatitis, and resulting disseminated intravascular coagulation, which resulted in his death.
4. Discussion
In recent years, LG procedures have become increasingly performed in Japan. While LG for advanced gastric cancer is still a controversy, it is reported not only that LG is superior to open gastrectomy in terms of offering less blood loss, shorter hospital stay, and lower risk of complications, but also that the scope of lymph-node dissection may be identical.21 We explained these facts to all patients, and LG was performed only to the patients who chose LG with an informed consent. Although the aim of this study was not to evaluate the oncological outcome of LG, we should clarify the survival with a long-term follow-up period in the future.
With the spread of LG, IH after LG with RY has become more common, as reported by many bariatric surgeons following LRYGB.3; 4; 5; 6; 7; 8; 9; 10; 11; 12; 13; 14; 15; 16; 22; 23; 24 ; 25 We initially introduced LG with antecolic RY and without closure of defects; subsequently, we observed more IH over time, whereas many studies of IH after LRYGB had mentioned that performing antecolic antegastric LRYGB could reduce IH, sometimes even without closure of defects.8; 9; 10; 11; 12; 13; 14; 15 ; 16 Moreover, the reported incidence of IH after LG with RY is not always low, particularly when defects were not closed (Table 6).2; 3; 4; 5; 6 ; 7 On the other hand, these studies often had shorter follow-up periods than the present study, in which more than 2 years elapsed since the last LG performed. In this respect, the IH incidence in our study may be more accurate than these studies with shorter follow-up periods.
| Author/year | Incidence of IH (%) | Laparoscopic or open (%) | Route of Roux limb (%) | Closure of Petersen | Closure of JJ | Follow-up period (mo) |
|---|---|---|---|---|---|---|
| Okabe et al2/2014 | 1.3 (2/158) | Laparoscopic (100) | Antecolic (100) | Yes | No | 29.6, median |
| Yoshikawa et al3/2014 | 2.8 (12/428) | Laparoscopic (42)/open (58) | Antecolic (98)/retrocolic (2) | No | No | 51.0, mean |
| Kelly et al4/2013 | 5.4 (16/298) | Laparoscopic (11)/open (89) | Antecolic (86)/retrocolic (14) | No | No | 22.4, median |
| Kojima et al5/2014a | 2.2 (6/268) | Laparoscopic (100) | Antecolic (100) | No | Yes | 43.1, median |
| 0 (0/90) | Yes | Yes | 9.2, median | |||
| Miyagaki et al6/2012 | 0.2 (18/8983) | Laparoscopic (14)/open (86) | Antecolic/retrocolic | No | Yes/no | 30.3, mean |
| Hosoya et al7/2011b | 6.9 (4/58) | Laparoscopic (100) | Antecolic (100) | No | No | 24.0, mean |
| 0 (0/115) | No | Yes | 9.2, mean |
IH = internal hernia; JJ = jejunojejunostomy mesenteric defect; Petersen = Petersens defect.
a. Internal hernia at Petersens defect was only reported.
b. Internal hernia at the jejunojejunostomy mesenteric defect was only reported.
Although IH after retrocolic LRYGB has been reported to occur after a shorter interval than with antecolic procedures, the reason for this is unknown.10; 22 ; 24 Our study showed a similar result; accordingly, clinicians should be particularly vigilant for IHs soon after LG with retrocolic RY. Moreover, this shorter interval clouds the reported association between IHs after LG and excess weight loss, which has been often considered to be a risk factor for IH after LRYGB,10 ; 25 although BMI at IH diagnosis is not available to us.
Although Petersen26 originally reported IH through the space formed by the stomach wall, the gastrojejunal anastomosis, the transverse mesocolon, and the retroperitoneum in a loop gastrojejunostomy,26 the meaning of “Petersens hernia” has varied to date.27 Recently, Petersens defect is considered to be the space between the dorsum of the Roux limb and the transverse mesocolon. However, this space continues superior to the transverse colon (i.e., the supracolic component), and therefore, Petersens defect is often simply considered as the back side of the Roux limb.28 Thus, this study regarded the entire space behind the Roux limb as the Petersens defect, in both antecolic and retrocolic RY. Apart from LRYGB, gastrectomy and lymph-node dissection are included in LG, and widen the space behind the Roux limb in antecolic RY, which may easily cause IH at Petersens defect. To narrow this defect, we initially adopted retrocolic RY to prevent IH at the supracolic component. Subsequently, we introduced the defect closure to prevent IH at the infracolic component. Hirahara et al29 reported a different technique in LDG with antecolic RY, using the greater omentum filled in between the remnant stomach and the pancreas space. Although this technique can prevent IH at both supracolic and infracolic spaces, it may be difficult to be adapted to LTG.
The closure of defects is known to reduce IH incidence after LG.5 ; 7 Our result with the jejunojejunostomy mesenteric defect also supports this fact. However, one patient did experience a recurrent IH, which resulted in his death, after the closure of all defects during an emergency surgery for the initial IH; the recurrent IH may have been caused by insufficient closure. Since April 2012, we have used nonabsorbable running sutures for closure,5 ; 7 and no IHs have been observed. Uncut RY may be an alternative procedure, which does not have this defect.30 ; 31 However, this technique requires the antecolic route. Thus, we should pay attention to the large Petersens defect instead.
IH at the transverse mesocolic defect is unique to retrocolic RY. In our study, two patients required bowel resection; both had undergone LTG with retrocolic RY and developed IH at this defect. Although the existence of this defect reportedly increases the IH incidence, the precise IH incidence had been unclear until now.8; 9; 10; 11; 12; 13; 14 ; 15 This study showed the incidence to be 1.3%, which is not very high. We closed this defect by fixing the gastrojejunostomy site to the mesocolon after anastomosis in LDG. In contrast, Iida et al28 mentioned that fixing the remnant stomach to the transverse mesocolon first facilitated anastomosis and filling this defect; it may therefore be a useful procedure. However, we are only able to fix the jejunum to the mesocolon in LTG. This difference in fixation might influence the occurrence of IH after LTG. The establishment of a more secure procedure to prevent IH at this defect in LTG is necessary.
An early diagnosis of IH is often challenging because of atypical symptoms or an insecure imaging diagnostic protocol.3; 4; 6; 10; 11; 13; 14; 15; 16; 17; 18; 22 ; 23 In Japan, we routinely follow LG patients for at least 5 years postoperatively; still, patients may first go to a primary care doctor when IH occurs. In fact, the patient with spontaneously vanishing massive ascites was transferred to our hospital during his third episode. Herniation through the large Petersens defect might cause resolvable but repeated ascites. In addition, elevated pancreatic enzymes and pancreatitis have also been reported as important IH symptoms and indicators of biliopancreatic limb obstruction.3; 13 ; 18 In our study, pancreatitis was a leading cause of IH-associated fatality. Although intermittent abdominal pain and vomiting are relatively well-known symptoms, other symptoms, such as repeated ascites or pancreatitis, should be better known to other clinicians.
In conclusion, retrocolic RY with the appropriate defect closures can reduce the incidence of IH at Petersens defect and the jejunojejunostomy mesenteric defect. In particular, our procedural modifications might be effective in preventing IH in the supracolic component of Petersens defect. Although the IH incidence at the transverse mesocolic defect was not particularly high, the possibility of IH at this site—which may be characterized by a shorter interval between LG and IH, and by severe ischemic damage of the incarcerated bowel—should be kept in mind.
References
- 1 Y. Isobe, A. Nashimoto, K. Akazawa, et al.; Gastric cancer treatment in Japan: 2008 annual report of the JGCA nationwide registry; Gastric Cancer, 14 (2011), pp. 301–316
- 2 H. Okabe, K. Obama, S. Tsunoda, E. Tanaka, Y. Sakai; Advantage of completely laparoscopic gastrectomy with linear stapled reconstruction: a long-term follow-up study; Ann Surg, 259 (2014), pp. 109–116
- 3 K. Yoshikawa, M. Shimada, N. Kurita, et al.; Characteristics of internal hernia after gastrectomy with Roux-en-Y reconstruction for gastric cancer; Surg Endosc, 28 (2014), pp. 1774–1778
- 4 K.J. Kelly, P.J. Allen, M.F. Brennan, M.J. Gollub, D.G. Coit, V.E. Strong; Internal hernia after gastrectomy for cancer with Roux-Y reconstruction; Surgery, 154 (2013), pp. 305–311
- 5 K. Kojima, M. Inokuchi, K. Kato, K. Motoyama, K. Sugihara; Petersens hernia after laparoscopic distal gastrectomy with Roux-en-Y reconstruction for gastric cancer; Gastric Cancer, 17 (2014), pp. 146–151
- 6 H. Miyagaki, S. Takiguchi, Y. Kurokawa, et al.; Recent trend of internal hernia occurrence after gastrectomy for gastric cancer; World J Surg, 36 (2012), pp. 851–857
- 7 Y. Hosoya, A. Lefor, T. Ui, et al.; Internal hernia after laparoscopic gastric resection with antecolic Roux-en-Y reconstruction for gastric cancer; Surg Endosc, 25 (2011), pp. 3400–3404
- 8 L. Elms, R.C. Moon, S. Varnadore, A.F. Teixeira, M.A. Jawad; Causes of small bowel obstruction after Roux-en-Y gastric bypass: a review of 2395 cases at a single institution; Surg Endosc, 28 (2014), pp. 1624–1628
- 9 A. Obeid, S. McNeal, M. Breland, R. Stahl, R.H. Clements, J. Grams; Internal hernia after laparoscopic Roux-en-Y gastric bypass; J Gastrointest Surg, 18 (2014), pp. 250–256
- 10 M. Abasbassi, H. Pottel, B. Deylgat, et al.; Small bowel obstruction after antecolic antegastric laparoscopic Roux-en-Y gastric bypass without division of small bowel mesentery: a single-centre, 7-year review; Obes Surg, 21 (2011), pp. 1822–1827
- 11 A. Rodriguez, M. Mosti, M. Sierra, et al.; Small bowel obstruction after antecolic and antegastric laparoscopic Roux-en-Y gastric bypass: could the incidence be reduced?; Obes Surg, 20 (2010), pp. 1380–1384
- 12 K.E. Steele, G.P. Prokopowicz, T. Magnuson, A. Lidor, M. Schweitzer; Laparoscopic antecolic Roux-En-Y gastric bypass with closure of internal defects leads to fewer internal hernias than the retrocolic approach; Surg Endosc, 22 (2008), pp. 2056–2061
- 13 E. Comeau, M. Gagner, W.B. Inabnet, D.M. Herron, T.M. Quinn, A. Pomp; Symptomatic internal hernias after laparoscopic bariatric surgery; Surg Endosc, 19 (2005), pp. 34–39
- 14 R.F. Hwang, D.E. Swartz, E.L. Felix; Causes of small bowel obstruction after laparoscopic gastric bypass; Surg Endosc, 18 (2004), pp. 1631–1635
- 15 J.K. Champion, M. Williams; Small bowel obstruction and internal hernias after laparoscopic Roux-en-Y gastric bypass; Obes Surg, 13 (2003), pp. 596–600
- 16 J. Ortega, N. Cassinello, D. Sánchez-Antúnez, C. Sebastián, F. Martinez-Soriano; Anatomical basis for the low incidence of internal hernia after a laparoscopic Roux-en-Y gastric bypass without mesenteric closure; Obes Surg, 23 (2013), pp. 1273–1280
- 17 S.A. Reddy, C. Yang, L.A. McGinnis, R.E. Seggerman, E. Garza, K.L. Ford 3rd; Diagnosis of transmesocolic internal hernia as a complication of retrocolic gastric bypass: CT imaging criteria; AJR Am J Roentgenol, 189 (2007), pp. 52–55
- 18 F.C. Campanile, C.E. Boru, M. Rizzello, et al.; Acute complications after laparoscopic bariatric procedures: update for the general surgeon; Langenbecks Arch Surg, 398 (2013), pp. 669–686
- 19 K. Washington; 7th edition of the AJCC cancer staging manual: stomach; Ann Surg Oncol, 17 (2010), pp. 3077–3079
- 20 Japanese Gastric Cancer Association; Japanese classification of gastric carcinoma: 3rd English edition; Gastric Cancer, 14 (2011), pp. 101–112
- 21 H.N. Tang, J.H. Hu; A comparison of surgical procedures and postoperative cares for minimally invasive laparoscopic gastrectomy and open gastrectomy in gastric cancer; Int J Clin Exp Med, 8 (2015), pp. 10321–10329
- 22 S. Parakh, E. Soto, S. Merola; Diagnosis and management of internal hernias after laparoscopic gastric bypass without mesenteric closure; Obes Surg, 17 (2007), pp. 1498–1502
- 23 L.A. Miyashiro, W.D. Fuller, M.R. Ali; Favorable internal hernia rate achieved using retrocolic, retrogastric alimentary limb in laparoscopic Roux-en-Y gastric bypass; Surg Obes Relat Dis, 6 (2010), pp. 158–162
- 24 R. Al-Sukaiti, L. Stein, N. Christou, B. Mesurolle, G.P. Artho; Imaging of small bowel obstruction following gastric bypass surgery for morbid obesity: a retrospective review; SQU Med J, 10 (2010), pp. 354–360
- 25 C. Schneider, W. Cobb, J. Scott, A. Carbonell, K. Myers, E. Bour; Rapid excess weight loss following laparoscopic gastric bypass leads to increased risk of internal hernia; Surg Endosc, 25 (2011), pp. 1594–1598
- 26 W. Petersen; Ueber darmverschlingung nach der gastroenterostomie; Langenbecks Arch Klin Chir, 62 (1900), pp. 94–114
- 27 A.M. Rogers, A.M. Ionescu, E.M. Pauli, A.H. Meier, T.R. Shope, R.S. Haluck; When is a Petersens hernia not a Petersens hernia; J Am Coll Surg, 207 (2008), pp. 121–124
- 28 A. Iida, Y. Hirono, D. Fujimoto, et al.; Retrocolic Roux-en-Y anastomosis for total laparoscopic distal gastrectomy: fix-the-remnant-first technique; Asian J Endosc Surg, 6 (2013), pp. 333–337
- 29 N. Hirahara, T. Matsubara, H. Hayashi, K. Takai, Y. Fujii, Y. Tajima; Easy and secure closure of Petersens defect after laparoscopic distal gastrectomy with Roux-en-Y reconstruction; J Laparoendosc Adv Surg Tech A, 25 (2015), pp. 55–59
- 30 S.H. Ahn, S.Y. Son, C.M. Lee, H. Jung do, J. Park do, H.H. Kim; Intracorporeal uncut Roux-en-Y gastrojejunostomy reconstruction in pure single-incision laparoscopic distal gastrectomy for early gastric cancer: unaided stapling closure; J Am Coll Surg, 218 (2014), pp. e17–21
- 31 I. Uyama, Y. Sakurai, Y. Komori, et al.; Laparoscopy-assisted uncut Roux-en-Y operation after distal gastrectomy for gastric cancer; Gastric Cancer, 8 (2005), pp. 253–257
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?