Abstract
Alkaptonuria is a rare metabolic disease caused by a partial or total deficiency of homogentisic acid oxidase, which results in excess homogentisic acid (HGA) levels. Homogentisic acid and its oxidation products can accumulate in hyaline cartilage, tendons, and ligaments. A 55-year-old male was admitted complaining of worsening chronic pain in his left knee. A radiographic evaluation showed tricompartmental end- stage osteoarthritis. A cemented total knee replacement was performed. At the 10-year follow-up, he had returned to full activity, had no knee pain, and was very satisfied with the outcome. No abnormality was observed in the femoral, tibial, or patellar components on radiography. We believe that total knee replacement is a good option in a patient with marked degenerative arthritis secondary to ochronotic arthritis.
Keywords
Ochronotic arthropathy ; Alkaptonuria ; Arthroplasty ; Knee joint
Alkaptonuria is a rare autosomal-recessive metabolic disease, resulting from excess homogentisic acid (HGA) due to an autosomal recessive mutation of the homogentisate 1,2-dioxygenase (HGO ) gene on chromosome 3. 1 ; 2 ; 3 It affects one in 100,000 to 250,000 individuals, although there is evidence that certain populations have a much higher incidence. 3 ; 4 It results from partial or total deficiency of homogentisic acid oxidase, which is present in the liver and kidneys. Homogentisic acid oxidase is responsible for the turnover of HGA in phenylalanine and tyrosine catabolism. Homogentisic acid and its oxidation products accumulate in hyaline cartilage, tendons, ligaments, the sclera, skin, heart valves, the cartilage of the nose and ears, renal tubule epithelial cells, pancreas, and arteries. 4 ; 5 ; 6
The diagnosis of alkaptonuria may be confirmed by quantifying homogentisic acid in urine. Currently, there is no specific treatment for alkaptonuria. The treatment is symptomatic, and consists of local heat, physiotherapy, analgesics, and external support. Surgical treatment can include synovectomy, arthroscopic debridement, or arthroplasty as indicated for the affected joint.4 ; 7 ; 8
This case report presents the long-term results of arthroplasty for the treatment of ochronotic arthropathy.
Case report
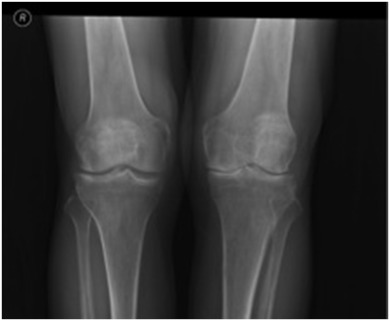
A 55-year-old male presented complaining of chronic knee pain that had worsened over the previous 3 years. This had been treated medically and with physiotherapy for the last year. The treatment included anti-inflammatory medications, two injections with viscosupplementation, and two intra-articular steroid injections, but resulted in no sustained improvement. On physical examination, the left knee was neutrally aligned. There was a mild effusion, with tenderness over the medial and lateral joint lines. The range of movement was from 0° of extension to 120° of flexion; extension was painless, while knee flexion was painful over the terminal 40°. There was no laxity of the collateral or cruciate ligaments. The distal neurovascular examination of the extremities was intact and symmetric. Radiographically, the left knee showed degenerative osteophytic changes and osteophytes in all compartments of both knees, with narrowing and sclerosis of the medial joint space (Fig. 1 ). The patient also had the darkly stained sclera and pinnae characteristic of ochronosis (Fig. 2 ).
|
|
|
Fig. 1. Preoperative radiographs showing osteoarthritic changes. |
|
|
|
Fig. 2. Pigmentation of sclerae and skin of peri-orbital area. |
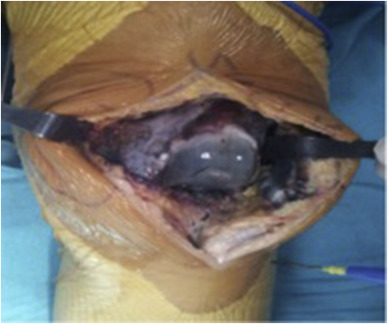
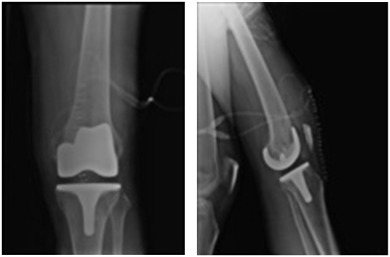
A cemented left total knee replacement was performed. Degeneration was observed throughout the knee, with loss of articular cartilage involving the medial and lateral compartments. A black pigment was deposited throughout the articular cartilage (Fig. 3 ). The postoperative radiographs showed that the total knee components were in good alignment and position (Fig. 4 ). The patient progressed well postoperatively, maintaining a good range of motion and achieving independent ambulation 4 weeks after surgery. At the 10-year follow-up, the patient had returned to full activities, reported no knee pain, and was very satisfied with the outcome. No abnormality of the femoral, tibial, and patellar components was observed in the plain x-rays taken 10 years postoperatively (Fig. 5 ).
|
|
|
Fig. 3. Macroscopic findings at surgery, showing black pigmentation in the synovium and articular surfaces. |
|
|
|
Fig. 4. Radiographs following total knee arthroplasty. |
|
|
|
Fig. 5. Anteroposterior and lateral radiograph of same knee at 10th year postoperatively, with stable components. |
Discussion
There is no effective treatment to replace the deficient enzyme in ochronosis. Some treatment modalities are currently being evaluated. Symptomatic treatment consists of non-steroidal anti-inflammatory drugs (NSAIDs), intra-articular steroid injection, and ascorbic acid. Treatment with high doses of ascorbic acid lowers the HGA excreted in urine,3 ; 4 but does not prevent the occurrence of arthropathy. The surgical treatment options include arthroscopic debridement, synovectomy, partial or total joint arthroplasty, and fusion.9 ; 10 ; 11 ; 12 ; 13 Nevertheless, our knowledge of the surgical treatment for ochronotic arthritis is limited to a few case reports with short follow-up.12 ; 13 ; 14 ; 15 ; 16 ; 17
Spencer et al performed arthroplasties for 11 joints in three patients who had lower and upper extremity ochronotic degenerative joint disease and reported good results at the 12-year follow-up.18
Arthroplasty is effective for treating severe arthritis of the knee ascribable to ochronosis. We report an excellent outcome with total knee replacement in a patient with significant degenerative arthritis secondary to ochronotic arthritis.
Conclusion
This study demonstrates that total knee replacement has excellent outcomes in a patient with significant degenerative arthritis secondary to ochronosis and joint replacement in alkaptonuric patients with ochronotic arthritis is associated with prosthetic survival comparable to that found in patients with primer osteoarthritis.
References
- 1 J.M. Fernández-Cañón, B. Granadino, D. Beltrán-Valero de Bernabé, et al.; The molecular basis of alkaptonuria; Nat Genet, 14 (1) (1996), pp. 19–24
- 2 A. Zatková, D.B. de Bernabé, H. Poláková, et al.; High frequency of alkaptonuria in Slovakia: evidence for the appearance of multiple mutations in HGO involving different mutational hot spots; Am J Hum Genet, 67 (5) (2000), pp. 1333–1339 Epub 2000 Oct 2
- 3 K. Forslind, F.A. Wollheim, B. Akesson, U. Rydholm; Alkaptonuria and ochronosis in three siblings. Ascorbic acid treatment monitored by urinary HGA excretion; Clin Exp Rheumatol, 6 (1988), pp. 289–292
- 4 J.M. Keller, W. Macaulay, O.A. Nercessian, I.A. Jaffe; New developments in ochronosis: review of the literature; Rheumatol Int, 25 (2005), pp. 81–85
- 5 D. Resnick; Alkaptonuria; D. Resnick, G. Niwayama (Eds.), Diagnosis of Bone and Joint Disorders (2nd ed.), W. B. Saunders, Philadelphia (1988), pp. 1787–1803
- 6 S. Aydogdu, E. Cullu, M.H. Ozsoy, H. Sur; Cementless total knee arthroplasty in ochronotic arthropathy: a case report with a 4-year follow-up; J Arthroplasty, 15 (2000), pp. 539–543
- 7 M. Raaijmaakers, F. Steenbrugge, C. Dierickx; Ochronosis, arthroscopy of a black knee: a case report and review of the literature; Knee Surg Sports Traumatol Arthrosc, 16 (2008), pp. 182–184
- 8 F.H. Laskar, K.D. Sargison; Ochronotic arthropathy. A review with four case reports; J Bone Jt Surg, 52 (1970), pp. 653–666
- 9 Y. Kabasakal, I. Kıyıcı, D. Özmen, A. Yağcı, G. Gümüşdiş; Spinal abnormalities similar to ankylosing spondylitis in a 58-year-old woman with ochronosis; Clin Rheumatol, 14 (1995), pp. 355–357
- 10 B. Balaban, M. Taşkaynatan, E. Yaşar, K. Tan, T. Kalyon; Ochronotic spondyloarthropathy: spinal involvement resembling ankylosing spondylitis; Clin Rheumatol, 25 (2006), pp. 598–601
- 11 E. Çetinus, I. Çever, C. Kural, H. Ertürk, M. Akyıldız; Ochronotic arthritis: case reports and review of the literature; Rheumatol Int, 25 (2005), pp. 465–468
- 12 M. Kefeli, Y. Tomak, B. Can, S. Bariş; Arthroplasty for the treatment of joint degeneration caused by ochronosis in two cases; Acta Orthop Traumatol Turc, 42 (2) (2008), pp. 139–144 [in Turkish)]
- 13 C. Kural, E.M. Cetinus, A. Kural, A.A. Uğraş, I. Kaya; Knee ochronotic arthropathy and arthroscopic findings; Acta Orthop Traumatol Turc, 43 (1) (2009), pp. 67–71 [in Turkish)]
- 14 K. Dom, T. Pittevils; Ochronotic arthropathy: the black hip case report and review of the literature; Acta Orthop Belg, 63 (2) (1997), pp. 122–124
- 15 A. Makela, O. Korkala; Hip arthroplasty for alkaptonuric ochronosis; Acta Orthop Scand, 57 (1986), pp. 171–172
- 16 O. Aynaci, C. Onder, A.U. Turhan; Bilateral hip arthroplasty for ochronotic arthropathy; Clin Rheumatol, 19 (2) (2000), pp. 150–152
- 17 A. Yilmaz, E. Egilmez; Knee arthroplasty for ochronotic arthropathy; J Knee Surg, 15 (4) (2002), pp. 231–233
- 18 J.M. Spencer, C.L. Gibbons, R.J. Sharp, A.J. Carr, N.A. Athanasou; Arthroplasty for ochronotic arthritis: no failure of 11 replacements in three patients followed for 6–12 years; Acta Orthop Scand, 75 (2004), pp. 355–358
Document information
Published on 31/03/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?