Abstract
Objectives
The aim of this study was to analyze the effect of tibial tunnel positioning in single bundle and double bundle ACL reconstructions on lateral meniscus anterior root.
Materials
Twelve single knee cadavers were used, 6 for a single bundle ACL reconstruction, which were reamed gradually starting from 8 mm, 9 mm and ended with a 10 mm reamers, while the other 6 were prepared for a double bundle ACL reconstruction in which 7 mm reamer for the AM tunnel and 6 mm reamer for the PL tunnel were used. After drilling, changes of lengths and thicknesses of anterior horns of the lateral menisci were recorded.
Results
Before drilling, the groups were homogenous for the lateral menisci dimensions. After drilling, no statistically significant difference was noticed between the two groups. However, in single bundle group, 2 anterior horns width injury (1.44 mm and 2.13 mm) with the 9 mm reamer and 3 anterior horns width injury (2.51 mm, 3.55 mm and 4.28 mm) with the 10 mm reamer were recorded. However in double bundle group a single anterior horn width injury (2.82 mm) was recorded.
Conclusion
Using a greater size reamer in single bundle reconstruction, causes a relatively higher risk of lateral meniscal anterior root injury. Lateral meniscus stability should be examined arthroscopically after reaming with large reamers.
Keywords
Anterior cruciate ligament reconstruction ; Anterior meniscus root ; Meniscus injury ; Tunnel reaming ; Cadaver study
Introduction
Anterior and posterior meniscus roots injuries disturb the normal transformation pattern of axial loads into circumferential stresses in the knee joint and leads to significant changes in its load-sharing capacity as a result of meniscal extrusion.1 ; 2 ; 3 ; 4
Certain injuries to the meniscus such as tearing of the meniscal root destroy its ability to resist circumferential stress, allowing meniscal instability to occur, which may lead to a future osteoarthritis.2 ; 5
Many studies demonstrated the close relationship of the menisci anterior roots to the anterior cruciate ligament (ACL), the three-dimensional anatomy of the menisci anterior root is still not well defined.6 ; 7 ; 8 ; 9 ; 10
Many studies have focused on the anterior horn tears of the medial meniscus and the relation of such tears with the anterior root attachment proximity to the ACL insertion.9 ; 11 ; 12 However it is strange not to find a well-organized anatomical study focusing on the effect of different ACL tibial tunnel placement techniques on the anterior horn of the lateral meniscus in the literature.
Recent arguments have been agreed on the placement of anterior cruciate ligament (ACL) reconstruction tunnels at the center of the anatomic attachment of the ACL. However, some other recent studies have suggested that placement of tibial tunnel at the center of the ACL footprint may also increase the risk of the anterior meniscal roots damage.13 ; 14 ; 15 These anterior root insertions are in close proximity to the native ACL insertion and have the potential to be disrupted with anatomic ACL reconstruction.7 ; 16 ; 17
This cadaveric study was conducted to assess the effect of different tibial tunnel placement techniques in ACL reconstruction procedures on the integrity of anterior root of the lateral meniscus in an in vitro setting when using different tibial reamer sizes.
Materials and methods
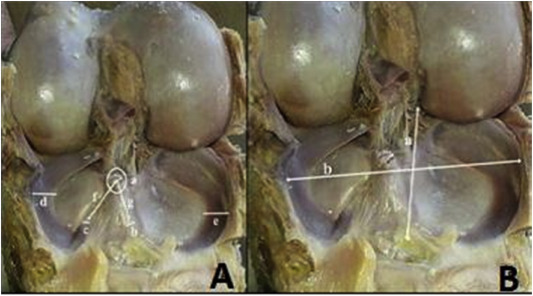
To obtain a two homogenous cadaveric groups, the tibial plateau dimensions (lateral–medial and anterior–posterior) of the cadaveric samples were chosen close to each others, for that reason only 12 single knees were selected for the trial from a total of 65 human cadaver specimens that were preserved in formalin based dilution for at less than 1 year. Donors were 12 men ranging in age from 49 to 72 years. The selected 12 knees were divided into two groups, each group receives one of the two methods of tibial tunnel placement techniques. Age, height and tibial plateau widths were distributed homogenously in order to minimize their influence on the results. The anterior–posterior and lateral–medial widths of tibial plateau, the length and the thickness of the anterior horns of lateral menisci were recorded. The lengths of the roots were evaluated by measuring the distance between the center (foot print) of ACL and the tip of root itself (Fig. 1 ).
|
|
|
Fig. 1. A. Measurements of the anatomical dimensions; ACL Footprint (a), Medial meniscus width (e), Lateral meniscus width (d), ACL footprint–medial meniscus anterior root distance (g), ACL footprint–lateral meniscus anterior root distance (f), Lateral meniscus anterior root width (c), Medial meniscus anterior root width (b). B. Tibial plateau anteroposterior width (a), tibia plateau medio-lateral width (b). |
Single tunnel technique, tibial tunnel placement
For creation of the anatomic ACL tibial tunnel, a 55 elbow tibial ACL reaming guide (Acufex, Smith & Nephew) was positioned in the center of the ACL footprint. The mid portion of the ACL tibial footprint was localized anterior to the posterior border of anterior horn of lateral meniscus.18 A 2.4-mm guide pin was then drilled inside out with the pin placed at the center of the ACL footprint on the proximal tibia and exiting from the anteromedial aspect of the tibia. Gradual reaming of all samples was performed starting with 8 mm reamer then followed by 9 mm reamer and finalized by 10 mm–diameter reamer (Cannulated Headed Reamer, Arthrex) were used for antegrade reaming over the guide pin.19
Double tunnel technique, tibial tunnel placement
Double tunnel tibial insertion site is carefully dissected with a sharp device, posteriolateral (PL) and anteromedial (AM) insertion sites are marked between the anterior tibial tubercle and the medial tibial crest. The elbow ACL tibial drill guide is set up at 45° and the tip of the drill guide is placed intra-articularly on the tibial footprints of the PL bundle. Another way to locate the tip of the tibial guide intra-articularly, is to place it just in front of the posterior root of the lateral menisci posterolateral to the AM bundle of the ACL and a guide-wire is then advanced. Another guide-wire is similarly advanced to the center of the AM insertion with the guide.20 A 2.4 mm guide wires are passed into the base of the PL and AM tibial footprints, which are then over-drilled, using cannulated reamers, 7 mm for the AM tunnel and 6 mm for the PL tunnel.
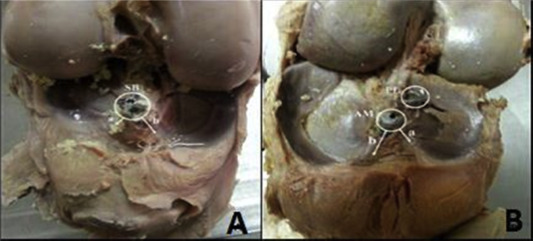
After drilling the tibial tunnels in both groups (Fig. 2 ), the iatrogenic damage of the anterior meniscal roots resulted from drilling were documented. All of measurements before and after drilling, were processed on high resolution images using an official image software (Osirix version 5.8.5 32-bit, Pixmeo Sarl, Switzerland). The measurements were statistically analyzed by using Mann Whitney–U test.
|
|
|
Fig. 2. A. Single bundle tibial tunnel–lateral meniscal root distance (a) Single bundle tibial tunnel–medial meniscal root distance (b). B. Double bundle AM tibial tunnel–lateral meniscal root distance (a) Double bundle AM tibial tunnel–medial meniscal root distance (b). |
Results
In the pre-reaming status, the anatomical measurements of knees have been made after dissection, in the first group the lateral menisci anterior roots mean widths was 6,61 ± 0,5 (5,91–7,24) mm, the lateral menisci anterior horns mean distance to the ACL center was 9,75 ± 0,8 (8,76–10,82) mm and the lateral menisci mean widths was 9,22 ± 1,7 (8,64–11,72) mm. In the second group of knees, the lateral menisci anterior roots mean widths was 6,36 ± 0,6 (6,41–8,31), the lateral menisci anterior horns mean distance to the ACL center was 9,49 ± 0,8 (8,67–10,55) mm and the lateral menisci mean widths was 9,53 ± 0,9 (8,83–12,20) mm. No statistical significance was detected between the measurements of the two groups (p = 0.631, p = 0.201, p = 0.368) respectively. The mean tibial plateau lateral–medial and anterior–posterior widths in group 1 was 72,09 ± 4,5 (64,83–76,36) mm and 44,71 ± 4,6 (38,71–51,97) mm respectively. The mean tibial plateau lateral–medial and anterior–posterior widths in group 2 was 71,11 ± 4,7 (65,92–79,15) mm and 45,01 ± 2,4 (42,64–48,72) mm respectively (Table 1 ). No statistical significance was detected between the two groups (p = 0.423, p = 0.337) respectively.
| LMAR width | ACL c-root d lat. | LM width | TP width L-M | TP Width A-P | ACL width L-M | ACL width A-P | Root injury | |
|---|---|---|---|---|---|---|---|---|
| SB Mean ± SD | 6,61 ± 0,5 | 9,75 ± 0,8 | 9,22 ± 1,7 | 72,09 ± 4,5 | 44,71 ± 4,6 | 10,08 ± 1,0 | 15,39 ± 1,0 | 1,72 ± 2,0 |
| DB Mean ± SD | 6,36 ± 0,6 | 9,49 ± 0,8 | 9,53 ± 0,9 | 71,11 ± 4,7 | 45,01 ± 2,4 | 9,73 ± 0,9 | 15,24 ± 1,4 | 0,47 ± 1,2 |
| P values | 0.631 | 0.201 | 0.368 | 0.423 | 0.337 | 0.873 | 0.522 | 0.216 |
In group 1 knees the mean ACL footprint anterior–posterior and lateral–medial widths were measured 15,39 ± 1,0 (13,99–16,64) mm and 10,08 ± 1,0 (8,25–11,09) mm respectively. In group 2 knees the mean ACL footprint anterior–posterior and lateral–medial widths were measured 15,24 ± 1,4 mm (12,99–16,71) mm and 9,73 ± 0,9 (8,32–10,96) mm respectively, no statistical significance was detected between the two groups (p = 0.873, p = 0.522) respectively.
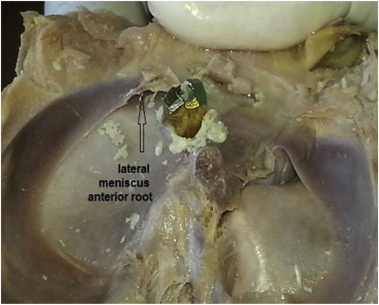
In group 1 (single bundle ACL reconstruction), after tibial reaming with 8 mm reamer, no meniscal anterior root injury was detected. However after reaming the tibial tunnel with 9 mm reamer, the width of 2 lateral menisci anterior horns were injured (1,44 mm and 2,13 mm) (Fig. 3 ). Reaming with 10 mm reamer resulted in damage to the lateral meniscal anterior root widths in 3 knees (2,51 mm, 3,55 mm and 4,28 mm). In group 2 (double bundle ACL reconstruction) only 1 lateral meniscal anterior root width damage was observed (2,82 mm). In the knees with single bundle drilling tunnel the injury risk of the lateral meniscus anterior root was relatively higher than that of the knees with the double bundle drilling tunnel. This is not statistically significant (p = 0.216).
|
|
|
Fig. 3. Anterior root injury of the lateral meniscus with a 9 mm reamer in a single tibia tunnel placement technique. |
Discussion
Meniscus main functions are shock absorption, load transmission and femoral congruency. Normal meniscal position is crucial for proper force transmission. In the presence of meniscal injury, load per unit area on the femorotibial joint cartilage is increased.5 The most important finding of the present study is that iatrogenic injury to the anterior roots of lateral menisci may occur while reaming ACL tibial reconstruction tunnels. Watson et al found that iatrogenic injury to the anterior roots of the medial and lateral menisci was seen in 25% and 67% of reamed tunnels respectively, even though the guide pin was positioned exactly in the calculated center of the ACL footprint.10 In our study lateral meniscus anterior root injuries were seen in both single and double bundle tibial tunnels placement. In knees with a single bundle drilling, smaller tunnels created less root injuries, however when the classical 10 mm reamer was used 50% (3 knees) injury of the lateral meniscal anterior horns was observed. Total injury of the anterior root was not recorded. A drill with a smaller diameter (6–7 mm) is generally used for double bundle drilling; therefore, the root injury ratio was found to be less than that of a single bundle drilling. While drilling a single bundle, a thicker drill (8–11 mm) is used which may be the reason for a higher injury ratio of the menisci anterior roots. Recent anatomical and biomechanical reports documented that the ACL has an apparent attachment over the anterolateral root that covers up to 63% of the AL root attachment area.17 ; 21 Moreover, another study reported that, based on the new knowledge of the lateral meniscal attachments, the centers of the anterolateral root and ACL were only 5 mm distant.17 Due to this close relationship, recent studies certified that the anterolateral root is at risk of injury when the tibial tunnel is placed anatomically during ACL reconstruction.13 ; 15
Meniscal posterior root avulsions result in a significant increase in peak contact pressure and decreased contact areas in comparison with the intact knee.12 ; 22 ; 23 ; 24 ; 25 Two studies also reported a significant increase of meniscal extrusion and gap formation after meniscus root injuries compared to intact and repaired roots.1 ; 26
Costa et al reported that 89% of anterior horn tears had 6 mm of meniscal extrusion, which is two times of the clinical standard that has been correlated with increased cartilage degeneration.9 Therefore, biomechanical, clinical and radiographic studies show that intact meniscal roots are essential for avoidance of articular cartilage damage in the knee. Although the clinically significant amount of meniscal root disruption has not been quantified. Loss of either the medial or lateral posterior meniscal root attachment has been shown to result in increased tibiofemoral contact pressures and decreased contact areas that may damage the articular cartilage.4 ; 26 ; 27 While total meniscectomies are no longer a common clinical practice, long-term follow-up studies have described higher levels of osteoarthritis and surgical reoperations after partial meniscectomy.23 ; 28 For this reason, meniscus root repair is recommended over partial or total meniscectomy in patients with meniscus root injury.24 Watson et al showed that even with guide pin placement in the center of the ACL footprint, the ACL reconstruction tibial tunnels may move anteriorly and meniscal root injury may result. In addition, this study shows that the ACL tibial tunnels have a slim margin of placement error before they could result in an iatrogenic anterior meniscal root injury, with increasing misaligned tibial tunnel placement theoretically leading to the possibility of a complete anterior meniscal root avulsions.24 ; 29
This anatomical study was conducted to assess the effect of different tibial tunnel placement techniques in ACL reconstruction procedures on the integrity of anterior root of the lateral meniscus in an in vitro setting when using different tibial reamers. We noticed that the smaller the tibial reamer in single bundle ACL reconstruction the less the injury resulted in the anterior horn of the lateral menisci.
The weakness of this study is its being an anatomical study. In which all reaming processes had been done after anatomical dissection not arthroscopically, which may minimize the error of anterior slip of the tunnel placement. Also the limited number of samples used in this study minimized the resultant anterior root injury. Further anatomical studies with large samples accompanied with biomechanical studies should be conducted to assess the impact of anterior horn injuries on meniscal stability in tibial tunnel placement techniques with variant tibial reamers in ACL reconstruction surgeries.
Conclusion
In this cadaveric study, anterior horns of the lateral menisci were more safe in ACL double tunnel placement technique maybe due to smaller reamers sizes used in tibial tunnel placement, smaller reamers are advised to be used in a single bundle tibial tunnel placement techniques, however further clinical trials are required to support this result.
This is a reminder for knee surgeons to pay attention while reaming the tibial plateau specially with big reamers in ACL reconstruction surgeries to examine arthroscopically the integrity and the stability of the anterior horn of the lateral meniscus.
References
- 1 A.M. Johannsen, D.M. Civitarese, J.R. Padalecki, M.T. Goldsmith, A. Coen, C.A. Wijdicks, R.F. LaPrade; Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci; Am J Sports Med, 40 (2012), p. 2342
- 2 C.M. LaPrade, W. Evan, E.W. James, L. Engebretsen, R.L. LaPrade; Anterior medial meniscal root avulsions due to malposition of the tibial tunnel during anterior cruciate ligament reconstruction: two case reports; Knee Surg Sports Traumatol Arthrosc, 22 (2014), pp. 1119–1123
- 3 M.F. Shepard, D.M. Hunter, M.R. Davies, M.S. Shapiro, L.L. Seeger; The clinical significance of anterior horn meniscal tears diagnosed on magnetic resonance images; Am J Sports Med, 30 (2) (2002), pp. 189–192
- 4 C.K. Schillhammer, F.W. Werner, M.G. Scuderi, J.P. Cannizzaro; Repair of lateral meniscus posterior horn detachment lesions: a biomechanical evaluation; Am J Sports Med, 40 (2012), pp. 2604–2609
- 5 D.B. Lerer, H.R. Umans, M.X. Hu, M.H. Jones; The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion; Skelet Radiol, 33 (2004), pp. 569–574
- 6 M.B. Ellman, C.M. LaPrade, S.D. Smith, et al.; Structural properties of the meniscal roots; Am J Sports Med, 42 (2014), p. 1881
- 7 T. Zantop, M. Wellmann, F.H. Fu, W. Petersen; Tunnel positioning of anteromedial and posterolateral bundles in anatomic anterior cruciate ligament reconstruction anatomic and radiographic findings; Am J Sports Med, 36 (1) (2008), pp. 65–72
- 8 C.G. Ziegler, S.D. Pietrini, B.D. Westerhaus, et al.; Arthroscopically pertinent landmarks for tunnel positioning in single-bundle and double-bundle anterior cruciate ligament reconstructions; Am J Sports Med, 39 (2011), pp. 743–748
- 9 C.R. Costa, W.B. Morrison, J.A. Carrino; Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear; Am J Roentgenol, 183 (2004), pp. 17–23
- 10 C.M. La Prade, S.D. Smith, M.T. Rasmussen, et al.; Consequences of tibial tunnel reaming on the meniscal roots during cruciate ligament reconstruction in a cadavericmodel, Part 1: the anterior cruciate ligament; Am J Sports Med US, 43 (1) (Jan 2015), pp. 200–206
- 11 M.J. Feucht, P. Minzlaff, T. Saier, A. Lenich, A.B. Imhoff, S. Hinterwimmer; Avulsion of the anterior medial meniscus root: case report and surgical technique; Knee Surg Sports Traumatol Arthrosc (2013) 013-2462-2467
- 12 J.R. Padalecki, K.S. Jansson, S.D. Smith, et al.; Root Attachment site: in situ pull-out repair restores derangement of joint mechanics biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior; Am J Sports Med, 42 (2014), pp. 699–704
- 13 M.T. Goldsmith, K.S. Jansson, S.D. Smith, L. Engebretsen, R.F. LaPrade, C.A. Wijdicks; Biomechanical comparison of anatomic single and double-bundle anterior cruciate ligament reconstructions an in vitro study; Am J Sports Med, 41 (2013), pp. 1595–1599
- 14 K.K. Middleton, T. Hamilton, J.J. Irrgang, J. Karlsson, C.D. Harner, F.H. Fu; Anatomic anterior cruciate ligament (ACL) reconstruction: a global perspective. Part 1; Knee Surg Sports Traumatol Arthrosc, 22 (2014), pp. 1467–1482
- 15 E. Monaco, B. Maestri, F. Conteduca, D. Mazza, C. Iorio, A. Ferretti; Extra-articular ACL reconstruction and pivot shift: in vivo dynamic evaluation with navigation; Am J Sports Med, 42 (2014), pp. 1669–1675
- 16 J.M. Brody, M.J. Hulstyn, B.C. Fleming, G.A. Tung; The meniscal roots: gross anatomic correlation with 3-T MRI findings; Am J Roentgenol, 188 (2007), pp. 447–450
- 17 C.M. LaPrade, M.B. Ellman, M.T. Rasmussen, et al.; Anatomy of the anterior root attachments of the medial and lateral menisci: a quantitative analysis; Am J Sports Med, 42 (2014), pp. 2386–2391
- 18 N. Reeboonlap, N. Kulkamthorn, K. Charakorn, A. Arkasihayuth; Tibial footprint for single anatomical anterior cruciate ligament reconstruction by the meniscal reference point: the cadaveric study; J Med Assoc Thai, 95 (Suppl. 10) (2012), pp. S163–S166
- 19 N.A. Streich, K. Friedrich, T. Gotterbarm, H. Schmitt; Reconstruction of the ACL with a semitendinosus tendon graft: a prospective randomized single blinded comparison of double-bundle versus single-bundle technique in male athletes; Knee Surg Sports Traumatol Arthrosc, 16 (3) (2008), pp. 232–238
- 20 Douglas W. Jackson; Master Techniques in Orthopaedic Surgery: Reconstructive Knee Surgery; (3rd ed.)Lippincott Williams & Wilkins (2008), p. 161
- 21 M.B. Ellman, C.M. LaPrade, S.D. Smith, et al.; Structural properties of the meniscal roots; Am J Sports Med, 42 (2014), pp. 1881–1887
- 22 C. Aga, M.T. Rasmussen, S.D. Smith, et al.; Biomechanical comparison of interference screws and combination screw and sheath devices for soft tissue anterior cruciate ligament reconstruction on the tibial side; Am J Sports Med, 41 (2013), pp. 841–848
- 23 C. Hoser, C. Fink, C. Brown, M. Reichkendler, W. Hackl, J. Bartlett; Long-term results of arthroscopic partial lateral meniscectomy in knees without associated damage; J Bone Jt Surg Br, 83-B (2001), pp. 513–516
- 24 J.N. Watson, K.J. Wilson, C.M. La Prade, et al.; Iatrogenic injury of the anterior meniscal root attachments following anterior cruciate ligament reconstruction tunnel reaming; Knee Surg Sports Traumatol Arthrosc Ger, 23 (8) (Aug 2015), pp. p2360–6
- 25 P. Navarro-Holgado, A. Cuevas-Pérez, M.A. Aguayo-Galeote, P. Carpintero-Benítez; Anterior medial meniscus detachment and anterior cruciate ligament tear; Knee Surg Sports Traumatol Arthrosc, 15 (2007), pp. 587–590
- 26 C.D. Harner, C.S. Mauro, B.P. Lesniak, J.R. Romanowski; Biomechanical consequences of a tear of the posterior root of the medial meniscus; J Bone Jt Surg Am, 91 (Suppl. 2) (2009), pp. 257–270
- 27 R. Allaire, M. Muriuki, L. Gilbertson, C.D. Harner; Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy; J Bone Jt Surg Am, 90 (2008), pp. 1922–1931
- 28 T. Stein, A.P. Mehling, F. Welsch, R. von Eisenhart-Rothe, A. Jäger; Long-term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal repairs; Am J Sports Med, 38 (2010), pp. 1542–1548
- 29 S. Bhatia, K. Korth, G.S. Van Thiel, et al.; Effect of tibial tunnel diameter on femoral tunnel placement in transtibial single bundle ACL reconstruction; Knee Surg Sports Traumatol Arthrosc, 24 (1) (Jan 2016), pp. 51–57 http://dx.doi.org/10.1007/s00167-014-3307-8 [Epub 2014 Sep 19]. PubMed PMID: 25236681
Document information
Published on 31/03/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?