Abstract
Objective
The aim of this study was to assess appropriateness of the sizes of available cervical disc prostheses based on tomographic measurement of human cervical vertebrae.
Methods
The anatomic dimensions of the C3–C7 segments were measured on 50 patients (age range 26–47 years) with computerized tomography scan and compared with the sizes of the popular cervical total disc prostheses (CTDP) at the market [Bryan (Medtronic), Prodisc-C (Synthes), Prestige LP (Medtronic), Discover (DePuy)]. The mediolateral and anteriorposterior diameters of the upper and lower endplates were measured with a digital measuring system.
Results
Overall, 43.7% of the largest implant footprints were smaller in the anterior-posterior diameter and 42.6% in the mediolateral diameter were smaller than cervical endplate measurements. Discrepancy of the level C5/C6 and C6/C7 was calculated as 56.2% at the anteroposterior diameter and 43.8% at the center of mediolateral diameter.
Conclusion
Large disparity has been found between the sizes of devices and cervical anatomic data.
Companies that produce CTDP should take care of the anatomical dimensions and generate different sizes of CTDP. Spine surgeon should be familiar with the size mismatch in CTDP that may affect the clinical and radiological outcome of the surgery.
Keywords
Discrepancy ; Cervical disc prostheses ; Anatomical cervical dimensions ; Mismatch ; Cervical degenerative disc disease
Introduction
Anterior cervical decompression and fusion is commonly performed and has been considered to be the gold standard surgical treatment option of symptomatic cervical degenerative disc disease for several decades.1 Total disc replacement (TDR) is an alternative surgical technique option to fusion after anterior neural decompression. The theoretical advantage of TDR is the maintenance of segmental mobility and, thereby, reduction or avoidance of adjacent segment degeneration and other limitations of fusion.2 ; 3 ; 4
Cervical total disc prostheses (CTDP) may experience failure due to complications such as subsidence, dislocation, vertebral body fracture, and device wear.5 With an incidence of 3%–10%, subsidence is the most commonly reported CTDP-related problem, which is caused by an unfitted CTDP.5 ; 6 The cause of subsidence is variable, from osteoporosis and incorrect endplate proceeding to insufficient load sharing.5 A CTDP should closely fit the vertebral endplates to share the axial load.5 An unfitted CTDP may cause abnormal kinematics, which could affect the center of rotation (COR) of cervical vertebrae. Changes in COR may result from an unstable CTDP and may also change loadings weight distribution at the adjacent levels and facet joints.7 It has been demonstrated that abnormal cervical alignment and heterotopic ossification is caused by unfitted CTDP.8
CTDPs are available in different sizes. Design of the CTDP endplates should be fitted to the dimensions of vertebral endplates. The purpose of the current study was to compare the footprints of the most popular CTDPs used in Turkey (Bryan, Medtronic, Minneapolis, MN, USA; Prestige LP, Medtronic, Fridley, MN, USA; Discover, DePuy, Raynham, MA, USA; ProDisc-C, Synthes, West Chester, PA, USA) using anatomic dimensions of cervical vertebrae received from digital computed tomography (CT) scans.
Materials and methods
A total of 400 endplates of 250 vertebrae in 50 patients (22 men, 28 women; age range: 27–52 years; mean age: 42.3 years) who had been treated at an outpatient clinic for non-radicular chronic cervical disc pain were assessed. CT scans were performed between September 2011 and March 2015. Sequential 1.25-mm continuous cross-sectional images were obtained parallel to the endplates of C3 to C7 on a CT unit (GE LightSpeed VCT, GE Healthcare, Little Chalfont, UK). Inclusion and exclusion criteria of the study are shown in Table 1 .
| Inclusion | Exclusion |
|---|---|
| Non-radicular chronic neck pain | Patients with radiculopathy or myelopathy |
| Destruction of bone induced by tuberculosis, tumors, or bone fracture | |
| No limitation on the visualisation of the cervical spine disc spaces (C1–C7) on CT scans | Congenital cervical anomalies |
| Prior cervical spine surgery |
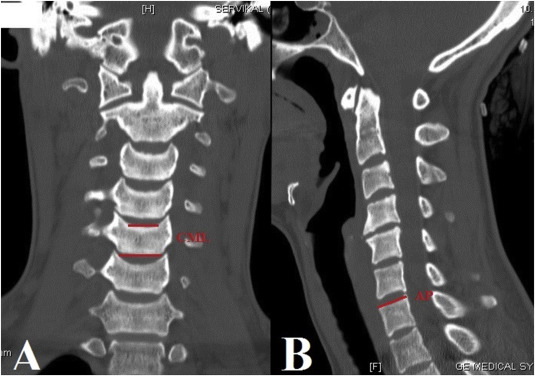
The following parameters were measured on CT scans1 (Fig. 1 ): center mediolateral (CML) diameter of the superior and inferior endplates of C3 to C7 in coronal CT scans2 ; and anterior-posterior (AP) diameter of the superior and inferior endplates of C3 to C7 in sagittal CT scans. Uncinate process and degenerative changes at the lateral border of the vertebrae were excluded in all measurements. Footprints of the most popular CTDPs used in Turkey were compared with anatomic parameters. Data were analyzed using Excel software (Excel 2013, Microsoft, Redmond, WA, USA).
|
|
|
Fig. 1. (A) The center mediolateral (CML) diameter of the superior and inferior endplates of C3–C7 in the coronal CT scans. (B) The anterior-posterior (AP) diameter of the superior and inferior endplates of C3–C7 in the sagittal CT scans. |
Results
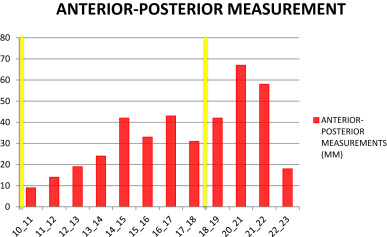
Measurement results are given in Table 2 . Range of AP measurement of the most popular CTDP was 10–18 mm, and range of the cervical endplate measurement was 10.33–22.91 mm (Table 3 ). Our measurements showed that 48.50% of cervical endplates did not match the diameter of the CTDP, 46.25% of endplates exceeded the largest diameter of the CTDP, and 2.25% of endplates were smaller than the smallest diameter of the prostheses. AP diameter of the largest available cervical disc prosthesis was 1.8 cm (Bryan, ProDisc-C).
| Levels | AP | CML |
|---|---|---|
| C3 Inferior | 15.76 (10.33–18.28) | 19.85 (8.28–22.13) |
| C4 Superior | 16.47 (11.92–19.03) | 18.84 (12.10–21.86) |
| C4 Inferior | 16.20 (12.03–20.39) | 18.19 (14.45–19.48) |
| C5 Superior | 17.52 (12.73–21.79) | 16.79 (13.42–25.61) |
| C5 Inferior | 15.93 (11.85–21.07) | 20.91 (15.71–22.01) |
| C6 Superior | 16.87 (13.08–22.02) | 21.38 (16.44–24.37) |
| C6 Inferior | 17.32 (14.88–22.91) | 22.71 (13.71–26.30) |
| C7 Superior | 17.80 (14.32–21.39) | 20.62 (14.51–27.95) |
|
|
|
Table 3. Anterior–posterior (AP) diameter of vertebral endplates at levels C4–C7. Relationship between vertebral endplates and cervical total disc prosthesis sizes. Yellow lines mark AP diameters of available sizes of cervical total disc prostheses. |
Overall, AP diameter of the different prostheses did not match anatomic dimensions (35.75% of Bryan and ProDisc-C footprints, 59.75% of Discover footprints, and 47.25% of Prestige footprints).
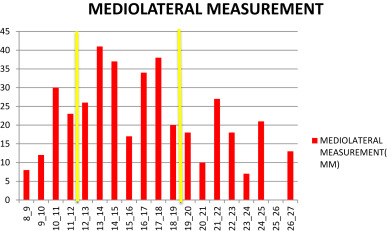
In terms of CML diameter, the range of measurements of the cervical prostheses and endplate size was 12–19 mm and 8.28–27.95 mm, respectively (Table 4 ). According to our findings, 46.75% of cervical endplates did not match the available sizes of prostheses, and 28.50% of endplates exceeded the largest footprint of all implant devices, while 18.25% of endplates were smaller than the smallest diameter of the prostheses. Additionally, 38.75% of Bryan and Prodisc-C footprints, 47.00% of Discover, and 42.25% of Prestige footprints did not match anatomic dimensions.
|
|
|
Table 4. Center Mediolateral (CML) diameter of vertebral endplates at levels C4–C7. Relationship between vertebral endplates and cervical total disc prosthesis sizes. Yellow lines mark CML diameters of available sizes of cervical total disc prostheses. |
Discussion
For decades, anterior cervical discectomy and fusion has been a successful treatment method of cervical degenerative disc disease with high clinical outcomes. During the last decade, TDR has been shown as an efficient reliable alternative method to anterior cervical discectomy and fusion, its observed advantages including greater physiologic distribution of range of motion, reduced adjacent level stresses, and lowered rate of adjacent segment degeneration.9 ; 10 ; 11
Due to these reasons, the use of TDR is growing rapidly both in Turkey and worldwide. While use of this surgical method rises in popularity, typical complications that are still observed include subsidence, anterior migration of the disc, lateral subluxation, evidence of polyethylene wear, and loosening with osteolysis.6 ; 7 Some studies suggest that one of the most prevalent reasons for such TDR failure is incorrect positioning of the implant,6 ; 12 which can be exacerbated due to the fact that every patients anatomy and condition requiring surgery is unique.
Some biomechanical studies have shown that implants with the largest possible surface area yield the best performance for avoiding subsidence due to the circumferential strongest areas in the periphery.13 The most important points are that the regional anatomic and biomechanical variations of the endplates are well understood. It has been shown that the posterior and lateral aspects of the cervical endplate are thicker and stronger than the anterior aspect and middle of the endplate.
Inadequate endplate design can equally contribute to subsidence as a result of extremely concentrated stress,5 which can increase the prevalence of adjacent segment degeneration. Rates of heterotrophic ossification (HO) following TDR have been reported as high as 76.2% at 3-year follow-up.8 Reports in the literature present many reasons for HO, including small prosthesis size in relation to vertebral endplate dimension.8
Size of implant can change COR, which can affect cervical alignment and kinematics. In our opinion, malposition of the CTDP is a direct cause of HO at the treated segment, and decrease in range of motion due to smaller CTDP could be an indirect cause of HO.
However, larger implants can cause complications (bleeding, lesions of adjacent structures such as laryngeal nerve, oesophagus, and trachea), which can occur in the surgical field during insertion of larger implants. A cervical disc device should be placed close to the ring apophysis because of its mechanical properties and the biomechanics of the cervical motion segment.14 ; 15
There may be differences in anatomical dimension between races. One study showed that width of the upper cervical endplate is larger in Caucasians than Koreans.16
In a study of 192 cervical endplates of 24 patients, a significant difference was found between implant and anatomic measurements,17 similar to findings in the present study.
One study found a large discrepancy between footprints of prostheses and Chinese cervical anatomic data in 414 segments.18 In the present study, measurements of 400 segments produced similar results.
In the present study, the endplates of the largest and smallest available disc prostheses were matched by a small percentage of endplates.
Conclusion
Large disparity has been found between sizes of CTDP and cervical anatomic data in our cohort. Our recommendation to CTDP manufacturers is to take into account anatomical sizes and produce CTDPs of different sizes for both upper and lower endplates. Spine surgeons should be aware that size mismatch in CTDP may affect the clinical and radiological outcomes of the procedure.
Conflict of interest
None declared.
References
- 1 J. Goffin, E. Geusens, N. Vantomme, et al.; Long-term follow-up after interbody fusion of the cervical spine; J Spinal Disord Tech, 17 (2004), pp. 79–85
- 2 J. Goffin, F. Van Calenbergh, J. van Loon, et al.; Intermediate follow-up after treatment of degenerative disc disease with the Bryan Cervical Disc Prosthesis: single-level and bi-level; Spine (Phila Pa 1976), 28 (2003), pp. 2673–2678
- 3 P.V. Mummaneni, R.W. Haid; The future in the care of the cervical spine: interbody fusion and arthroplasty. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004; J Neurosurg Spine, 1 (2004), pp. 155–159
- 4 C. Wigfield, S. Gill, R. Nelson, I. Langdon, N. Metcalf, J. Robertson; Influence of an artificial cervical joint compared with fusion on adjacent-level motion in the treatment of degenerative cervical disc disease; J Neurosurg, 96 (1 Suppl.) (2002), pp. 17–21
- 5 C.Y. Lin, H. Kang, J.P. Rouleau, S.J. Hollister, F.L. Marca; Stress analysis of the interface between cervical vertebrae end plates and the Bryan, Prestige LP, and ProDisc-C cervical disc prostheses: an in vivo image-based finite element study; Spine (Phila Pa 1976), 34 (15) (2009), pp. 1554–1560 http://dx.doi.org/10.1097/BRS.0b013e3181aa643b
- 6 S.Y. Fong, S.J. DuPlessis, S. Casha, R.J. Hurlbert; Design limitations of Bryan disc arthroplasty; Spine J, 6 (2006), pp. 233–241
- 7 A. van Ooij, F.C. Oner, A.J. Verbout; Complications of artificial disc replacement: a report of 27 patients with the SB Charité disc; J Spinal Disord Tech, 16 (2003), pp. 369–383
- 8 J.M. Cao, Y.Z. Zhang, Y. Shen, W.Y. Ding; Complications of Bryan cervical disc replacement; Orthop Surg, 2 (2010), pp. 86–93
- 9 L. Pimenta, P.C. McAfee, A. Cappuccino, F.P. Bellera, H.D. Link; Clinical experience with the new artificial cervical PCM (Cervitech) disc; Spine J, 4 (2004), pp. 315S–321S
- 10 R.C. Sasso, J.D. Smucker, R.J. Hacker, J.G. Heller; Clinical outcomes of BRYAN cervical disc arthroplasty: a prospective, randomized, controlled, multicenter trial with 24-month follow- up; J Spinal Disord Tech, 20 (2007), pp. 481–491
- 11 D. Murrey, M. Janssen, R. Delamarter, et al.; Results of the prospective, randomized, con- trolled multicenter Food and Drug Administration investigational device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease; Spine J, 9 (2009), pp. 275–286
- 12 R. Bertagnoli; Complications and rescue strategies in TDR procedures; 20th Annual Meeting of the North American Spine Society (NASS) (2005) Philadelphia, PA
- 13 S.H. Zhou, I.D. McCarthy, A.H. McGregor, R.R. Coombs, S.P. Hughes; Geometrical dimensions of the lower lumbar vertebrae analysis of data from digitised CT images; Eur Spine J, 9 (3) (2000), pp. 242–248
- 14 C.C. Cheng, N.R. Ordway, X. Zhang, Y.M. Lu, H. Fang, A.H. Fayyazi; Loss of cervical endplate integrity following minimal surface preparation; Spine (Phila Pa 1976), 32 (17) (2007), pp. 1852–1855
- 15 T. Steffen, A. Tsantrizos, M. Aebi; Effect of implant design and endplate preparation on the compressive strength of interbody fusion constructs; Spine (Phila Pa 1976), 25 (9) (2000), pp. 1077–1084
- 16 M.K. Kim, D.S. Kwak, C.K. Park, et al.; Quantitative anatomy of the endplate of the middle and lower cervical vertebrae in Koreans; Spine (Phila Pa 1976), 32 (2007), pp. E376–E381
- 17 M. Thaler, S. Hartmann, M. Gstöttner, R. Lechner, M. Gabl, C. Bach; Footprint mismatch in total cervical disc arthroplasty; Eur Spine J, 22 (2013), pp. 759–765
- 18 L. Dong, M.S. Tan, Q.H. Yan, et al.; Footprint mismatch of cervical disc prostheses with Chinese cervical anatomic dimensions; Chin Med J (Engl), 128 (2) (2015 Jan 20), pp. 197–202 http://dx.doi.org/10.4103/0366-6999.149200
Document information
Published on 31/03/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?