Abstract
Objectives
The purpose of this study was to compare the outcomes of non-operative treatment and operative repair of grade III injuries with complete rupture of the collateral ligament of the proximal interphalangeal (PIP) joint.
Patients and methods
Seventeen patients with grade III injuries with at least 6 months of follow-up were included. Seven patients underwent non-operative treatment and 10 patients underwent operative treatment. We evaluated the following clinical outcomes after treatment: 1) range of motion of the PIP and distal interphalangeal (DIP) joints, 2) joint stability, 3) pain score, and 4) amount of fusiform deformity of the PIP joint.
Results
There was no instability in the lateral stress test in either group. The ranges of motion of the PIP and DIP joints were not statistically different between the two groups at final follow-up. However, the ranges of motion recovered more quickly in the operative group than the non-operative group within the first 3 months after treatment. Patients in the operative group had less pain and better cosmetic appearance of the PIP joint.
Conclusion
Our results suggest that operative repair of the PIP collateral ligament can provide good joint stability, rapid functional recovery, and minimize fusiform deformity of the PIP joint.
Level of evidence
Level III, Therapeutic study.
Keywords
Proximal interphalangeal joint ; dislocation ; PIP collateral ligament ; Surgical repair ; Suture anchor
Introduction
Collateral ligament injury of the proximal interphalangeal (PIP) joint is a common injury encountered by orthopedic surgeons. The treatment goals of PIP joint collateral ligament injury are recovery of joint stability and achievement of normal ranges of motion. Patients also desire rapid functional recovery, limited pain during treatment, and good appearance of the PIP joint. The general consensus is that incomplete rupture of the PIP collateral ligament should not be treated operatively; however, for grade III injuries with complete rupture of the ligament, treatment is more controversial. Non-operative treatment is often adopted even for complete rupture of the PIP collateral ligament.1 ; 2 ; 3 However, some hand surgeons recommend operative repair for complete rupture of the PIP collateral ligament due to residual pain, instability, and weakness of pinch strength after non-operative treatment.4 ; 5 ; 6 ; 7 However, there is no convincing evidence that operative repair expedites healing or improves motion.2 The purpose of this study was to evaluate clinical outcomes after operative repair of complete rupture of the PIP collateral ligament compared with those obtained by non-operative treatment.
Patients and methods
We conducted a retrospective, comparative study of patients with grade III collateral ligament injuries of the PIP joint. Our institutional review board granted approval for this study. Inclusion criteria were grade III collateral ligament injuries of the PIP joint with at least 6 months of follow-up. We defined grade III collateral ligament injury of the PIP joint as 1) patients who had no end point in a manual stress test of the PIP joint and 2) greater than 20° in the PA radiograph with lateral stress taken with the PIP joint at 0° of extension (Fig. 1 ).3 ; 4 ; 5 We excluded patients with accompanying injury to the hand and wrist, or with diabetes, rheumatoid arthritis, or degenerative arthritis in the injured hand. Seventeen patients met our criteria, and all injuries were to the radial collateral ligaments. One hand fellowship-trained surgeon treated all patients. Among 17 patients, seven patients underwent non-operative treatment and 10 patients underwent operative repair. Patients' demographics are summarized in Table 1 according to treatment group.
|
|
|
Fig. 1. Plain radiograph with lateral stress of the proximal interphalangeal (PIP) joint showing the angle between the axial line of the middle phalanx and proximal phalanx (α). This angle of more than 20° indicates a grade III lateral collateral ligament injury of the PIP joint. |
| Non-operative group | Operative group | |
|---|---|---|
| Number | 7 | 10 |
| Age (years) | 26.7 | 26.7 |
| Gender (M/F) | 5/2 | 9/1 |
| Volar plate avulsion (yes/no) | 4/3 | 6/4 |
| Injured finger | ||
| Long | 3 | 5 |
| Ring | 3 | 3 |
| Little | 1 | 2 |
Evaluation method and statistical analysis
We evaluated the following clinical outcomes after treatment: 1) range of motion of the PIP and distal interphalangeal (DIP) joints, 2) joint stability, 3) pain score, and 4) amount of fusiform deformity of the PIP joint. We measured the active ranges of motion of the PIP and DIP joints with a finger goniometer at 1, 2, 3, and 6 months after treatment. We assessed the stability of the PIP joint with a manual lateral stress test at final follow-up. Pain was assessed with a visual analog scale (VAS), where 0 indicated no pain and 10 the most severe pain. We assessed fusiform deformity of the PIP joint by measuring the difference between the maximal width of the same finger PIP joint on the contralateral hand and the injured PIP joint with electronic digital calipers (Woodcraft® , Parkersburg, WV, USA). We considered the maximal width as the distance from the ulnar side apex to the radial side apex of the PIP joint (Fig. 2 ). One physician assistant, who was unaware of the radiographic results and independent of the treating surgeon, recorded VAS pain scores. She measured the maximal width of the PIP joint twice, and the average of two measurements was used to determine maximal PIP width. We used the Mann–Whitney U test to evaluate the significance of differences between the two groups. Statistical significance was accepted for P values of <0.05.
|
|
|
Fig. 2. The maximal width of the proximal interphalangeal (PIP) joint was measured as the distance from the ulnar side apex to the radial side apex of the PIP joint. |
Non-operative treatment
The PIP joint of the injured finger was immobilized with a finger palmar splint for 1 week and was buddy-taped to the adjacent radial finger for an additional 3 weeks. Active mobilization of the finger began during buddy taping.
Operative repair
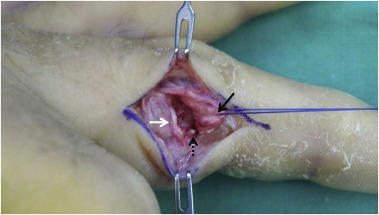
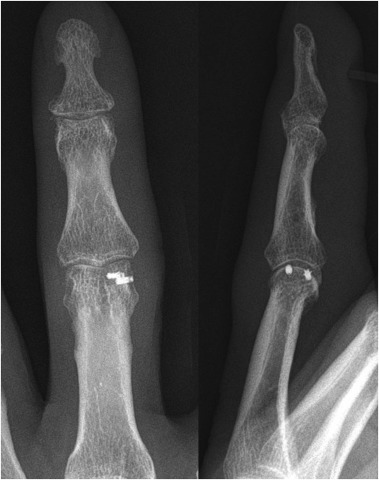
We made a midlateral skin incision of approximately 2 cm on the radial side of the PIP joint. The transverse retinacular ligament was incised and the lateral band was retracted dorsally. We can observe the avulsed collateral ligament and volar plate (Fig. 3 ). Typically, collateral ligaments fail proximally, and volar pate avulses digitally.2 We carefully inspected the remnant of the collateral ligament on the condyle of the proximal phalanx to decide on the repair method. In two cases, the remnant of the collateral ligament on the condyle of the proximal phalanx was enough to suture directly and the collateral ligament was repaired with nylon 4/0 using multiple simple or mattress sutures. In eight cases, the remnant was not enough to suture directly and we used a suture anchor. We used a mini-suture anchor in the first patient, but the patient complained of skin irritation due to the large suture knot. After that, we change the micro-suture anchors (Micro-QUICKANCHOR® Plus, DePuyMitek, Switzerland) to decrease the knot size (Fig. 4 ). The drill hole was made on the original attachment site of the collateral ligament of proximal phalanx condyle. After drilling, the micro-suture anchors was placed the drill hole, and the position of the anchor was confirmed using an image intensifier. The stability of the anchor was checked by pulling the thread. The avulsed end of the collateral ligament was sutured using horizontal mattress sutures and then fixed to the anchor. In addition, the avulsed volar plate was repaired to the remnant of volar plate with 5/0 vicryl suture in six patients with the concurrent volar plate injury, while the remaining four patients had partial ruptures of the volar plate and the joint capsule. After capsular repair, the stability of the repaired ligament was checked by manual stress test. After the operation, the finger was immobilized with a finger palmar aluminum splint for 3 days, and then active flexion and extension exercise of the finger began with buddy tape to the radial adjacent finger for 3 weeks.
|
|
|
Fig. 3. Intraoperative photograph demonstrating the ruptured radial collateral ligament (black arrow: distal end, white arrow: proximal remnant) and avulsion fragment of the volar plate (dashed arrow). |
|
|
|
Fig. 4. Post-operative anteroposterior and lateral plain radiographs demonstrating two micro-suture anchors on the head of the proximal phalanx. |
Results
Ranges of motion of the PIP and DIP joints
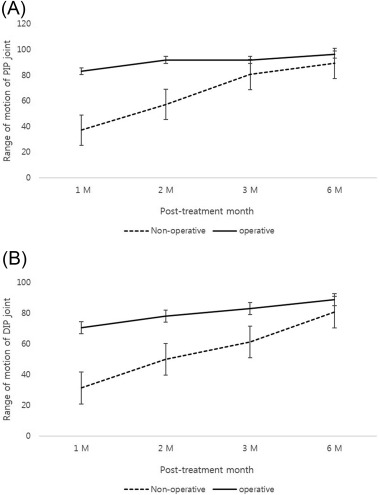
The ranges of motion of the PIP and DIP joints in both groups recovered gradually over 6 months after treatment. The ranges of motion of the PIP and DIP joints recovered more rapidly in the operative group within the first 3 months after treatment than in the non-operative group (P < 0.05). However, the ranges of motion of the PIP and DIP joints were not statistically different at final follow-up between the two groups (Fig. 5 ).
|
|
|
Fig. 5. Graphs showing the range of motion of the proximal (A) and distal interphalangeal joints (B) at 1, 2, 3, and 6 months after treatment. The ranges of motion of the PIP and DIP joints recovered more quickly in the operative group than the non-operative group within the first 3 months after treatment (P < 0.05). |
VAS pain score and difference in the maximal width of the PIP joint
The mean VAS pain score in the non-operative group (3 points) was higher than that in the operative group (1 point) (P < 0.05). The mean maximum-width difference of the finger PIP joint between the injured and contralateral normal finger in the non-operative group (2.85 mm) was wider than that in the operative group (1.75 mm) (P < 0.05) (Table 2 ).
| Non-operative group | Operative group | P -value | |
|---|---|---|---|
| VAS pain score | 3.0 ± 0.8 | 1.0 ± 1.2 | 0.008a |
| Fusiform deformityb | 2.8 ± 0.9 mm | 1.7 ± 0.7 mm | 0.031a |
VAS: Visual analog scale.
a. Statistical significance was accepted for P -values of <0.05.
b. Fusiform deformity of PIP joint was evaluated with width difference of PIP joint between injured and contralateral normal finger.
Complications
At final follow-up, PIP joint stability was maintained and no clinical evidence of residual instability was identified in any of the patients. One surgery performed using a mini-suture anchor was complicated by skin irritation from the suture anchor knot. We removed the knot at the 8-month postoperative check-up due to persistent discomfort.
Discussion
We showed that operative repair of grade III radial collateral ligament injuries of the PIP joint resulted in a lower VAS pain score, more rapid recovery of finger motion, and better cosmetic appearance of the PIP joint than non-operative treatment at short-term follow-up. Our results support the use of operative repair of the collateral ligament in patients with grade III collateral ligament injury.
The general consensus regarding treatment of grade I and II ligament injuries is non-operative treatment; however, for grade III injuries with complete rupture of the ligament, treatment is still controversial. There are some reports that non-operative treatment of grade III ligament injuries can yield good results and that the injuries only require operative repair when the PIP joint exhibits subluxation or when closed reduction is insufficient.1 ; 2 ; 3 ; 8 ; 9 In contrast, Redler reported that operative repair is necessary due to trapping of soft tissue between the distal portion of the avulsed collateral ligament and its point of attachment to the proximal phalanx.7 McCue reported that early surgical repair of injuries yielded good results in young athletes who were cooperative and motivated and who had the benefit of supervised rehabilitation,6 and Isani and Kato recommended operative repair in young workers and athletes.4 ; 5 ; 10 Our results also support operative repair of collateral ligament in patients with grade III collateral ligament injury.
Successful outcomes of treatment of grade III collateral ligament injury are not only joint stability and restored range of motion of the PIP joint, but also rapid recovery of joint motion, less pain, and good appearance of the PIP joint. Previous successful reports after non-operative treatment did not consider rapid functional recovery, pain during treatment, or the cosmetic appearance of the PIP joint.1 ; 2 ; 3 ; 8 ; 9 Although surgeons are satisfied with the functional outcomes of non-operative treatment such as joint stability and range of motion, patients are often unsatisfied with their outcomes due to cosmetic problems and pain; this is especially true for young and middle-aged women. The PIP joint will often remain permanently thicker after injury in spite of optimal care, and tenderness and soreness with use may persist for 6–12 months.1 We found that patients who underwent surgical repair reported less pain and had a PIP joint with a better appearance at the final follow-up than those who did not undergo surgical repair.
In our study, strong repair of the collateral ligament provided sufficient mechanical stability for early joint motion. However, we could not recommend the patients in the non-operative treatment group to start active motion exercise of PIP joint 3 days after operation because of concern about joint instability. In cases where there was a remnant of the collateral ligament to suture strongly, we used suture anchors, as these provide strong mechanical stability for early motion exercises, consistent with the findings of mechanical and clinical studies.4 ; 5 ; 11 ; 12 ; 13 We started active motion exercises of the PIP joint 3 days after the operation. Early exercise of the PIP joint is related to rapid functional recovery of PIP joint motion.
The lateral collateral ligament is an important structure that maintains lateral stability, and the volar plate is an important structure for maintaining anterior and posterior stabilities; it also contributes partially to lateral stability.2 ; 3 ; 8 The volar plate is a secondary stabilizer against lateral deviation, especially when the collateral ligaments are incompetent. More than 20° of deformity on the lateral stress test in extension indicates complete collateral ligament injuries and injury to at least one other secondary stabilizer such as the volar plate, bony anatomy, and/or accessory collateral ligament.2 ; 3 We found that all 10 patients in the operative group had concurrent injury to the volar plate. Six of these patients had complete rupture of the volar plate, while the remaining four patients had partial ruptures of the volar plate and the joint capsule.
This study had several limitations. First, the number of cases was small and the follow-up period was short. Second, it was not a randomized case control study. It was retrospective comparative study, thus there was bias that can affect out results. Future prospective randomized studies with large number of cases are required to address the limitations of the current study.
In conclusion, our results suggest that operative repair of grade III PIP collateral ligament injuries can provide good joint stability, rapid functional recovery, and minimize fusiform deformity of the PIP joint.
Conflicts of interest and financial support
None.
References
- 1 A.J. Vicar; Proximal interphalangeal joint dislocations without fractures; Hand Clin, 4 (1) (1988), pp. 5–13
- 2 G. Merrel, J.F. Slade; Dislocations and ligament injuries in the digits; S.W. Wolfe (Ed.), Greens Operative Hand Surgery (6th ed.), vol. 1, Elsevier, Philadelphia (2011), pp. 291–332
- 3 T.R. Kiefhaber, P.J. Stern, E.S. Grood; Lateral stability of the proximal interphalangeal joint; J Hand Surg Am, 11 (1986), pp. 661–669
- 4 H. Kato, A. Minami, M. Takahara, et al.; Surgical repair of acute collateral ligament injuries in digits with the Mitek bone suture anchor; J Hand Surg Br, 24 (1) (1999), pp. 70–75
- 5 N. Kato, K. Nemoto, H. Nakajima, T. Motosuneya, K. Fujikawa; Primary repair of the collateral ligament of the proximal interphalangeal joint using a suture anchor; Scand J Plast Reconstr Surg Hand Surg, 37 (2003), pp. 117–120
- 6 F.C. McCue, R. Honner, M.C. Johnson, et al.; Athletic injuries of the proximal interphalangeal joint requiring surgical treatment; J Bone Jt Surg Am, 52 (1970), pp. 937–956
- 7 I. Redler, J.T. Williams; Rupture of a collateral ligament of the proximal interphalangeal joint of the finger. Analysis of eighteen cases; J Bone Jt Surg Am, 49 (1967), pp. 322–326
- 8 J. Andrew; Proximal interphalangeal joint dislocation without fractures; Hand Clin, 4 (1988), pp. 5–13
- 9 G.L. Woods, R.I. Burton; Avoiding pitfalls in the diagnosis of the acutely injured proximal interphalangeal joint; Clin Plast Surg, 8 (1981), pp. 95–105
- 10 A. Isani; Small joint injuries requiring surgical treatment; Orthop Clin North Am, 17 (1986) 407–119
- 11 W.W. Dzwierzynski, F. Pintar, H.S. Matloub, N. Yoganandan; Biomechanics of the intact and surgically repaired proximal interphalangeal joint collateral ligaments; J Hand Surg Am, 21 (4) (1996), pp. 679–683
- 12 S.F. Morris, D. Yang, A.D. Milne, B.A. Smyth; Reconstruction of the proximal interphalangeal joint collateral ligaments using the Mitek Micro Arc Anchor: an in vitro biomechanical assessment; Ann Plast Surg, 42 (2) (1999), pp. 124–128
- 13 J.I. Lee, W.J. Jeon, D.H. Suh, et al.; Anatomical collateral ligament reconstruction in the hand using intraosseous suture anchors and a free tendon graft; J Hand Surg Eur, 37 (9) (2012), pp. 832–838
Document information
Published on 31/03/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?