Summary
Ectopic sebaceous glands (ESGs) are benign esophageal lesions that have a lower detection rate than malignant lesions because most patients are asymptomatic. However, this rate can be increased by the widespread use of endoscopes and an increasing awareness of the disease. Through esophagogastroduodenoscopy, ESGs often appear in the middle and lower esophagus in numbers ranging from 1 to more than 100 yellowish plaques measuring 1–2 mm in diameter. Histopathological examination of ESGs would reveal small lobular cluster glands in the lamina propria. Diagnosis is usually confirmed through an endoscopic biopsy. ESGs are best distinguished from other yellowish lesions such as xanthoma via endoscopy. These lesions tend to appear singly scattered, whereas xanthomas tend to be clustered. We present three cases of ESGs in the esophagus. Although their etiologies are still unclear, we present related theories in our review.
Keywords
Ectopic sebaceous glands ; Endoscopy ; Esophagus ; Xanthoma
Introduction
Esophageal benign lesions have been detected less often than malignant lesions, accounting for only 0.5% of autopsy cases, because most patients are asymptomatic [1] . However, benign esophageal lesions can be detected more often by the widespread use of endoscopes and an increasing awareness of the disease. Sebaceous glands are normally found in human hair follicles, but ectopic areas have been reported around the eyes and in the oral cavity, tongue, larynx, palms, soles, and external genitalia, which are lined with squamous cells. Sebaceous glands in the esophagus were first reported in 1962 by De La Pava and Pickren [2] and are rarely found. The apparent low incidence of this condition may be because of the lack of obvious clinical signs and symptoms. Most cases were discovered incidentally by endoscopy in patients referred for gastrointestinal tract examination.
Ectopic sebaceous glands (ESGs) are best distinguished from other yellowish plaques such as xanthoma through endoscopy. Esophageal xanthomas were first reported in 1984 by Remmele and Engelsing [3] . One study showed that the most common location of xanthoma was the stomach (76%), followed by the esophagus (12%) and duodenum (12%) [4] . Coincidently, both ESGs and xanthomas are detected in the lower esophagus and should be confirmed via tissue biopsy.
Understanding the endoscopic and pathological features of esophageal lesions is essential for the detection, differential diagnosis, and management of ESGs and xanthomas. These two rare esophageal benign lesions are difficult to differentiate according to morphology. This study compares the differences between these benign lesions in the esophagus.
Case reports
Case 1
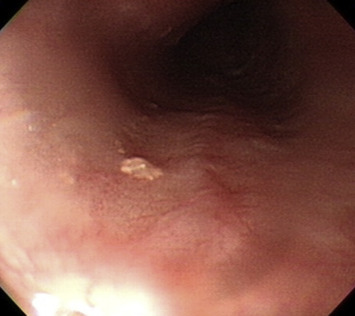
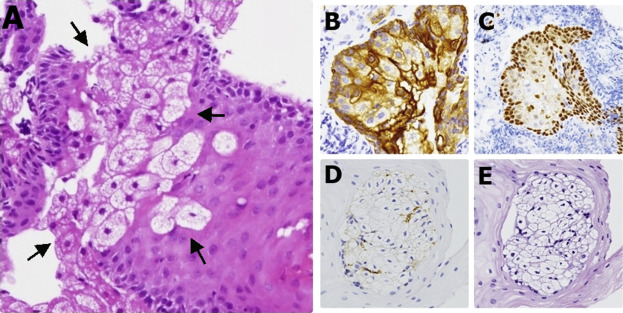
A 67-year-old man presented at our outpatient department with a 10-month history of epigastralgia and abdominal fullness. No significant abnormality was found on physical examination or laboratory tests. Esophagogastroduodenoscopy (EGD) revealed a 0.3 cm, single, yellowish plaque 33 cm from an incisor. The plaque presented as a slightly elevated shape with an uneven surface (Figure 1 A). A mucosal break of about 3 mm was found in the lower esophagus, which was diagnosed as a gastroesophageal reflux disease, Los Angeles class A. Histopathological examination of a resected specimen revealed esophageal mucosa covered by benign squamous epithelium with focal ESGs composed of sebaceous cells (Figure 2 A). The immunohistochemical staining was positive for cytokeratin (Figure 2 B), and a small number of cells were positive for P40 (Figure 2 C) but negative for CD68 (Figure 2 D) and mucin (Figure 2 E). Lymphocyte infiltration was present in adjacent tissue.
|
|
|
Figure 1. EGD revealed a single 0.3-cm yellowish plaque at 33 cm from the incisor. It presented as a slightly elevated shape with an uneven surface. EGD = esophagogastroduodenoscopy. |
|
|
|
Figure 2. (A) Esophageal mucosa covered by benign squamous epithelium with focal heterotopic sebaceous glands composed of sebaceous cells (arrows) (H&E, 200×). IHC statins: (B) positive for CK; (C) positive for P40; (D) negative for CD68; and (E) negative for mucin. H&E = hematoxylin and eosin; IHC = Immunohistochemistry. |
Case 2
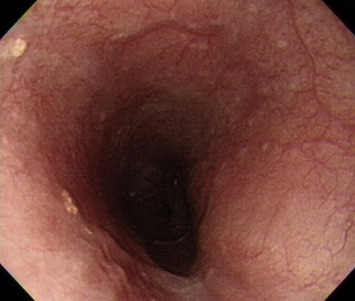
A 65-year-old woman presented at our clinic because of intermittent epigastralgia for some time. She denied smoking or alcohol drinking. EGD revealed two tiny yellowish plaques in her lower esophagus. The plaques presented as slightly elevated shapes with uneven surfaces (Figure 3 ). Histopathological examination revealed that the esophageal mucosa was covered by benign squamous epithelium with focal ESGs.
|
|
|
Figure 3. EGD revealed two tiny yellowish plaques in the lower esophagus. It presented as a slightly elevated shape with an uneven surface. EGD = esophagogastroduodenoscopy. |
Case 3
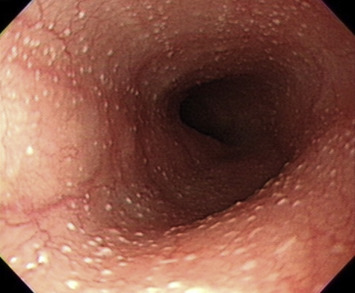
A 44-year-old woman presented at our clinic with intermittent epigastralgia and fullness accompanied by nausea and vomiting. EGD revealed more than 100 tiny yellowish dots of 0.1 cm in diameter scattered throughout the upper and lower esophagi (Figure 4 ). ESGs present as small lobules embedded in the lamina propria on histological examination.
|
|
|
Figure 4. EGD revealed more than 100 tiny yellowish dots, 0.1 cm in diameter, scattered throughout the upper and lower esophagus. EGD = esophagogastroduodenoscopy. |
Discussion
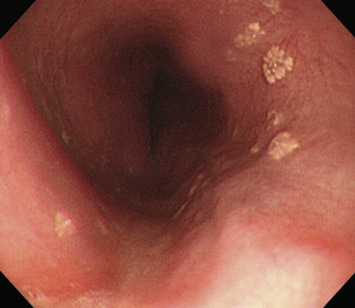
ESGs and xanthomas in the esophagus (Figure 5 ) have similar epidemiology, such as patient age (mean, 50 years), endoscopic features (yellowish, small, mildly elevated lesions), and clinical symptoms (asymptomatic), with good prognoses. To the best of our knowledge, no case reports have discussed their differences. We present three cases of ESGs and one case of xanthoma in the esophagus that had similar endoscopic findings and age distributions. A comparison between the esophageal ESGs and xanthoma is provided in Table 1 .
|
|
|
Figure 5. EGD revealed some well-defined, fern-like, yellowish lesions scattered over the middle and lower esophagus. EGD = esophagogastroduodenoscopy. |
| Ectopic sebaceous gland | Xanthoma | |
|---|---|---|
| Prevalence | Middle age, equal between men and women | Middle age, mild predominance in men |
| Possible pathogenesis | Metaplastic process; may be associated with reflux gastritis | May derive from focal mucosal damage |
| Endoscopic features | Single | Clusters |
| Yellowish | Yellowish | |
| Located in the lower esophagus | Located in the lower esophagus | |
| <5 mm | 2–10 mm | |
| Papular surface with irregular margin | Fern-like plaque | |
| Histopathological features | Small lobules embedded in the lamina propria that contain an excretory duct without hair follicles | Foamy macrophages distributed in the lamina propria with central or eccentric nuclei |
| Clinical significance | Asymptomatic | Asymptomatic |
| Recommended management | Good prognosis | Good prognosis |
| Observation alone | Observation alone |
ESGs and xanthomas are rarely found in the esophagus. For ESGs in the esophagus, the typical mean patient age at onset is 50 years, with almost equal distribution in men and women [5] . For esophageal xanthoma, also known as “xanthelasma” and “lipid island,” the mean patient age at onset is 54 years, with mild predominance in men [6] ; [7] . ESGs are most likely the result of a metaplastic process rather than a congenital anomaly. As ESGs are derived from endodermal tissue, it is unlikely that they are derived from ectodermal tissue [8] . ESGs are rarely found in infants or children, supporting the belief that they are less likely to be a congenital anomaly [9] ; rather, ESGs are suspected to be associated with reflux gastritis. Accordingly, the theory of an acquired metaplastic change of the esophageal epithelium was suggested in a 79-year-old man [10] . Only one of our patients had gastroesophageal reflux disease. All the patients were diagnosed with ESG in the lower esophagus. In our opinion, the theory of acquired metaplastic change is possible, but there is not enough evidence to support it.
The etiology of esophageal xanthomas is still unknown. One study reported a theory that gastric xanthoma is derived from focal mucosal damage in which the lipids were derived from broken-down cell membranes and captured by interstitial histiocytes [11] . This may explain why the esophageal mucosa has a better tolerance to damage than the gastric mucosa and the fewer reports of xanthoma in the esophagus [4] . No significant associated clinical symptoms or signs have been reported.
For ESGs in the esophagus, the number of occurrences has ranged from 1 to more than 100 (which was consistent with the findings in our patients), and lesion sizes have ranged from 1 mm to 20 mm, with the majority of cases being smaller than 0.5 cm [12] . Factors that affect the pattern and distribution of ESGs in the esophagus require further study. They have several different shapes and a yellowish appearance; smaller lesions are flat or dome shaped, or have a papular surface with irregular margins. Esophageal xanthomas are located most often in the lower esophagus and are about 2–10 mm in size [7] . They appear as well-defined, fern-like yellowish plaques scattered over the middle or lower esophagus, with the plaques being composed of clusters or groups.
Coincidently, both ESGs and xanthomas are detected in the lower esophagus and should be confirmed via tissue biopsy. On histological examination, ESGs present as small lobules embedded in the lamina propria that contain an excretory duct without hair follicles. Immunohistochemical staining shows keratin expression, especially for antikeratin [10] . In Case 1, the immunohistochemical stain was positive for cytokeratin but negative for CD68, mucin, periodic acid Schiff, or periodic acid Schiff with diastase. We also found a small number of cells positive for P40. The xanthoma presented as foamy macrophages distributed in the lamina propria of the mucosa, with small nuclei located centrally or eccentrically [7] .
We are still unsure of the detailed etiology of benign esophageal ESGs and xanthomas, in which patients have similar age at onset, endoscopic morphology, and clinical symptoms. ESGs tend to appear singly scattered, whereas xanthomas tend to be clustered. However, distinguishing them according to endoscopic findings alone remains a challenge. Most cases had no significant overall changes in ESG number, size, or shape during follow-up. We suggest that ESGs do not need further treatment.
Conflicts of interest
All authors declare no conflicts of interest.
References
- [1] A. Plachta; Benign tumors of the esophagus. Review of literature and report of 99 cases; Am J Gastroenterol, 38 (1962), pp. 639–652
- [2] S. De La Pava, J.W. Pickren; Ectopic sebaceous glands in the esophagus; Arch Pathol, 73 (1962), pp. 397–399
- [3] W. Remmele, B. Engelsing; Lipid island of the esophagus. Case report; Endoscopy, 16 (1984), pp. 240–241
- [4] R. Gencosmanoglu, E. Sen-Oran, O. Kurtkaya-Yapicier, N. Tozun; Xanthelasmas of the upper gastrointestinal tract; J Gastroenterol, 39 (2004), pp. 215–219
- [5] Y.S. Kim, S.Y. Jin, C.S. Shim; Esophageal ectopic sebaceous glands; Clin Gastroenterol Hepatol, 5 (2007), p. A23
- [6] M. Hirokawa, R. Takenaka, A. Takahashi, K. Sugihara, H. Wada, T. Tashiro, et al.; Esophageal xanthoma: report of two cases and a review of the literature; J Gastroenterol Hepatol, 18 (2003), pp. 1105–1108
- [7] G. Becheanu, M. Dumbrava, T. Arbanas, M. Diculescu, N. Hoyeau-Idrissi, J.F. Fléjou; Esophageal xanthoma—report of two new cases and review of the literature; J Gastrointestin Liver Dis, 20 (2011), pp. 431–433
- [8] A.A. Guiducci, A.B. Hyman; Ectopic sebaceous glands. A review of the literature regarding their occurrence, histology and embryonic relationships; Dermatologica, 125 (1962), pp. 44–63
- [9] L.E. Rector, M.L. Connerley; Aberrant mucosa in esophagus in infants and in children; Arch Pathol, 31 (1941), p. 285
- [10] Y. Nakanishi, A. Ochiai, T. Shimoda, H. Yamaguchi, Y. Tachimori, H. Kato, et al.; Heterotopic sebaceous glands in the esophagus: histopathological and immunohistochemical study of a resected esophagus; Pathol Int, 49 (1999), pp. 364–368
- [11] J. Lechago; Lipid islands of the stomach: an insular issue?; Gastroenterology, 110 (1996), pp. 630–632
- [12] I.F. Wei, C.C. Chang, C.L. Fang, C.R. Hsieh, J.J. Wang, H.Y. Lou, et al.; Education and imaging. Gastrointestinal: ectopic sebaceous glands in the esophagus; J Gastroenterol Hepatol, 23 (2008), p. 338
Document information
Published on 15/05/17
Submitted on 15/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?