Summary
Objective
Our objective was to compare the perioperative parameters of needle-assisted and conventional laparoendoscopic single-site adrenalectomy (LESS-A).
Methods
We compared 23 patients undergoing needle-assisted LESS-A with 29 patients undergoing conventional LESS-A at Hiroshima University Hospital between November 2009 and February 2014. Needle-assisted LESS-A was performed using a MiniLap instrument (Stryker, San Jose, CA, USA). We used this instrument to protectively retract the liver at the right side of the tumor and the spleen at the left side by grasping with a Securea endoscopic surgical spacer (Hogy Medical Co., Ltd., Tokyo, Japan). Various parameters including insufflation time, estimated blood loss, pain scale, resumption of oral intake, transfusion rate, and complications were analyzed using the Mann–Whitney U test.
Results
In all cases, LESS-A was completed successfully with no major intraoperative complications. Patients in both treatment groups had similar age, body mass index, sex, and laterality. Significantly, needle-assisted LESS-A was performed using the transumbilical approach rather than the subcostal approach. The insufflation time of the needle-assisted LESS-A was shorter than that of the conventional LESS-A (p = 0.0335). No patients required intraoperative or postoperative blood transfusions. Retrospective design and the small sample size are main limitations of this study.
Conclusion
Needle-assisted LESS-A was performed safely and in a manner that mitigated many of the difficulties of LESS surgery.
Keywords
adrenal tumor;laparoendoscopic single-site surgery;needlescopic surgery
1. Introduction
Since the early 1990s, laparoscopic adrenalectomy has been a standard procedure for the majority of patients with a surgical adrenal tumor.1 In conventional laparoscopic adrenalectomy, three or four ports are used. A paradigm shift in the field of minimally invasive surgery is now underway, and laparoscopy is progressing ever closer toward scarless surgery. With the advent of multichannel single ports as well as articulating instruments, laparoendoscopic single-site (LESS) surgery has been reported and the use of LESS surgery has increased. Over the past few years there has been increasing enthusiasm and growing interest in this novel, minimally invasive surgical technique.2 LESS surgery has been performed for various urological diseases, and studies have shown that it results in less pain, shorter hospital stays, and excellent cosmetic outcomes compared to other techniques.3 However, the LESS procedure is a technically challenging approach, which limits broader application of the technique.4 Surgeons are confronted with a number of difficulties not evident in conventional laparoscopy, such as the lack of instrument triangulation, instrument shaft clashing, and the need for ambidexterity. LESS adrenalectomy (LESS-A) through umbilical access can be extremely challenging due to the angle of approach and the difficulty of organ retraction.
Needlescopic-assisted LESS is a variation of LESS. In this approach, instead of introducing conventional LESS instruments through the multichannel port, additional needle-like 2–3 mm instruments are used. This results in minimal trauma to the abdominal wall and is promising for scarless surgery because the abdominal entry points do not necessitate closure of the insertion site after instrument retrieval.5
The main advantage of needlescopic-assisted LESS is that it overcomes one of the basic limitations of LESS, which is the lack of instrument triangulation. Additional instruments are regularly used to retract target tissues, and retracting the liver in the case of right-sided adrenal surgery and the spleen in the case of left-sided adrenal surgery are the most common indications of the placement of the additional instruments.6 In short, needlescopic-assisted LESS surgery avoids many of the major difficulties encountered using the single-site approach. In this study, we compare perioperative parameters between needle-assisted and conventional LESS-A.
2. Patients and methods
2.1. Participants
We compared 23 patients undergoing needle-assisted LESS-A with 29 patients undergoing conventional LESS-A at Hiroshima University Hospital, Hiroshima, Japan between November 2009 and February 2014. All patients consented to LESS-A and additional incisions if necessary. Fifty-two consecutive patients underwent transperitoneal LESS-A by two surgeons (S.I and A.M.). S.I. had experienced only three cases of multiport laparoscopic adrenalectomy and performed most cases of LESS-A (45 cases; 87%). For the first 20 cases, we used only the subcostal approach, but the by transumbilical approach for female patients after that. Various parameters including insufflation time, estimated blood loss, pain scale, resumption of oral intake, transfusion rate, and complications, were analyzed. Convalescence was measured by using a visual analog scale (VAS) ranging from 0 (negligible pain) to 10 (severe discomfort).
2.2. Surgery
Under general anesthesia, the patients were placed in the 60° modified flank position and the operators stood facing the abdomen between the arcus costalis on the ipsilateral side and the umbilicus. A 2-cm skin incision and an access into the peritoneal cavity were made by open laparotomy. A single-port device was constructed using Lap Protector (Hakko Co. Ltd., Tokyo, Japan) and a powder-free surgical glove. The wound retractor was inserted into the incision site and the upper part of the wound retractor ring was covered with a size-7½ surgical glove. The three trocars were 5-mm EZ trocars (Hakko Co. Ltd.).
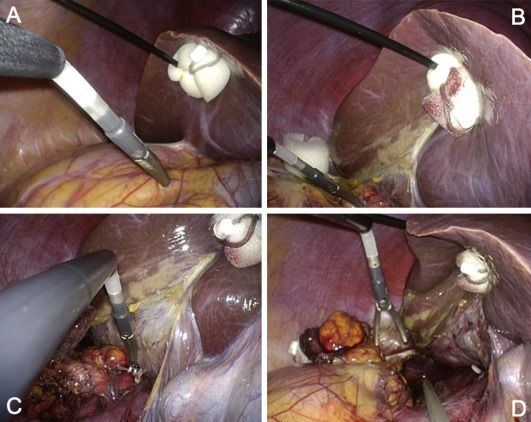
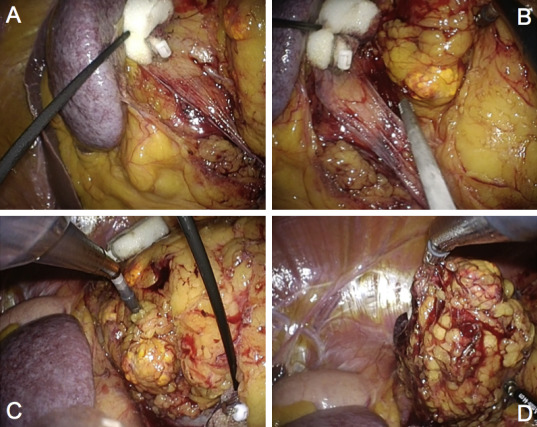
To minimize instrument collision, a flexible 5-mm 0° high-definition laparoscope (Olympus, Tokyo, Japan) was used. Pneumoperitoneum was induced by CO2 gas insufflation to 12 mmHg. The surgical strategy followed that for a conventional transperitoneal adrenalectomy.6 Specifically, the Toldt line and the typical vascular landmarks (inferior vena cava and renal vein for right- and left-sided adrenal tumors, respectively) were dissected and exposed using a bent laparoscopic instrument (Roticulator Endo Dissect; Covidien, Mansfield, MA, USA) and straight standard instruments. For the right-sided adrenal tumor, the right liver lobe was retracted using a snake retractor in the conventional laparoscopic adrenalectomy approach. We used a 2.3-mm MiniLap instrument (Stryker, San Jose, CA, USA) in this series. This instrument protectively retracted the liver on the right side (Fig. 1) and the spleen on the left side of the tumor (Fig. 2) by grasping the endoscopic surgical spacer Securea (Hogy Medical Co., Ltd., Tokyo, Japan) to avoid a traumatic procedure as cushioning to retract.
|
|
|
Figure 1. Needle-assisted laparoendoscopic single-site adrenalectomy (right side). (A, B) MiniLap instrument protectively retracts the liver by grasping the endoscopic surgical spacer Securea. (C) The adrenal veins are clipped with Hem-o-lok. (D) The entire adrenal gland is freed within the abdomen. |
|
|
|
Figure 2. Needle-assisted laparoendoscopic single-site adrenalectomy (left side). (A, B) MiniLap instrument protectively retracts the spleen by grasping the endoscopic surgical spacer Securea. (C) MiniLap instrument protectively retracts the perirenal fat. (D) The large adrenal gland is freed within the abdomen. |
The adrenal veins were identified, controlled with two 5-mm polymer locking clips (Hem-o-lok, Teleflex Medical, Research Triangle Park, NC, USA), one proximally and one distally, and then divided. A 5-mm LigaSure (Covidien) was used to complete the adrenal gland dissection. After hemostasis was ensured, the entire adrenal gland associated with the tumor was freed within the abdomen. In all cases, the specimen was retrieved through the Lap Protector without any further skin incision. A surgical suction drain was left in place through the surgical port. Transperitoneal LESS-A was successfully performed for all patients.
3. Results
3.1. Demographics
The patient demographics are listed in Table 1. There was no conversion to open surgery for any patient. Two patients, however, were switched to a conventional laparoscopic adrenalectomy by the placement of two additional 12-mm trocars. For the remaining 52 patients, the LESS-A was completed successfully without any intraoperative complications. There was no significant intergroup difference in age, male-to-female ratio, affected side, body mass index (BMI), or tumor size. With growing experience, indications can be expanded to include more challenging cases. The transumbilical approach ratio was used in 65.2% and 10.3% for the needle-assisted and the conventional LESS-A, respectively (p < 0.001). The ratio of pheochromocytoma was 13.0% and 6.9% for the needle-assisted and conventional LESS-A, respectively (p = 0.4552).
| Surgical procedure | Needle-assisted | Conventional | p |
|---|---|---|---|
| No. of patients | 23 | 29 | |
| Sex | |||
| Male | 8 (34.8) | 15 (51.7) | 0.2218 |
| Female | 15 (65.2) | 14 (48.3) | |
| Laterality | |||
| Right | 10 (43.5) | 16 (55.2) | 0.4022 |
| Left | 13 (56.5) | 13 (44.8) | |
| Age (y) | 51.0 (27–75) | 55.5 (35–73) | 0.2118 |
| Body mass index (kg/m2) | 22.7 (18.2–33.0) | 23.7 (18.2–34.4) | 0.3481 |
| Tumor size (mm) | 21.9 (9–45) | 22.0 (9–72) | 0.9850 |
| Preoperative diagnosis | |||
| Primary aldosteronism | 14 (60.9) | 17 (58.6) | |
| Pheochromocytoma | 3 (13.0) | 2 (6.9) | |
| Preclinical Cushings syndrome | 2 (8.7) | 5 (17.2) | |
| Cushings syndrome | 2 (8.7) | 3 (10.3) | |
| Nonfunctional adenoma | 2 (8.7) | 2 (6.9) | |
Data are presented as n (%) or mean (range).
3.2. Surgical outcomes
The surgical outcomes are shown in Table 2. In terms of insufflation time, the needle-assisted LESS-A was significantly shorter than the conventional LESS-A (121.4 minutes vs. 155.9 minutes; p = 0.0335). There was no significant difference in the estimated blood loss of the two groups (31.1 mL vs. 32.8 mL; p = 0.8467). None of the patients in either group required blood transfusion.
| Surgical procedure | Needle-assisted | Conventional | p |
|---|---|---|---|
| Approach | |||
| Transumbilical | 15 (65.2) | 3 (10.3) | < 0.001 |
| Subcostal | 8 (34.8) | 26 (89.7) | |
| Insufflation time (min) | 121.4 (79–234) | 155.9 (61–340) | 0.0335 |
| Estimated blood loss (mL) | 31.1 (6–75) | 32.8 (9–72) | 0.8467 |
| Transfusion | 0 | 0 | N.S. |
| Resumption of oral intake (POD), mean | 1 | 1 | N.S. |
| Visual analog scale | |||
| at POD 1 | 3.26 (0–10) | 2.59 (0–5) | 0.9592 |
| at discharge | 1.56 (0–6) | 0.90 (0–2) | |
| Complication | 0 (0) | 1 (3.4) | 0.3900 |
| Postoperative hospital stay (d) | 6.3 (4–11) | 8.2 (3–14) | 0.0062 |
Data are presented as n (%) or mean (range), unless otherwise indicated.
N.S. = not significant; POD = postoperative day.
The mean visual analog scale was 3.26 and 2.59 on postoperative Day (POD) 1 and 1.56 and 0.90 at discharge in the needle-assisted and the conventional LESS-A, respectively. There was no significant difference in pain relief between the two groups despite the use of needlescopic instruments. Postoperative hospital stay was significantly shorter for patients in the needle-assisted LESS-A group than for those in the conventional LESS-A (6.3 days vs. 8.2 days; p = 0.0062).
A minor serosal injury occurred in Patient 1 during open laparotomy and was in situ repaired with intermittent sutures before access port insertion (Clavien Grade 1). The incision was hidden within the umbilicus, and the scar after insertion of the needlescopic instrument had disappeared at postoperative 6 months ( Fig. 3).
|
|
|
Figure 3. Postoperative appearance of patients abdomen after needle-assisted laparoendoscopic single-site adrenalectomy. |
4. Discussion
Laparoscopic adrenalectomy has become the gold standard for the treatment of adrenal tumors and it comes with a variety of approaches.7 Many investigators have developed techniques for reducing the number of ports required to perform safe laparoscopic surgery.8 Although much effort has been extended to reduce invasiveness in laparoscopic adrenalectomy further, an incision is ultimately required for specimen retrieval.9
To date, the main advantage of LESS surgery over conventional laparoscopic surgery has been the improved cosmetic outcome. We have previously reported that young patients and female patients who had received LESS-A were more satisfied with the scar outcomes than were those who had received conventional laparoscopic adrenalectomy.10 The use of only one incision within the umbilicus renders selected transperitoneal procedures scarless. Therefore, the level of patient scar satisfaction was excellent.11 Zhang et al12 used retroperitoneoscopic LESS-A for diverse adrenal tumors, and they found that LESS-A was comparable with conventional LA perioperatively. However, the most severe problem of retroperitoneoscopic LESS-A is not to realize scarless surgery. Despite this cosmetic advantage, use of LESS is still not widespread due to its technical difficulty. LESS surgery remains a challenging procedure, especially for the transumbilical approach, because incomplete triangulation and more complex motion of the articulating instruments limits effective dissection.13 Moreover, as the target area for dissection becomes more cranial, dissection with the transumbilical LESS procedure will become extremely difficult. We had difficulty driving the instruments and avoiding internal and external collisions.4 These limitations are typical of all LESS procedures, reflecting the small space between the hands of the surgeon and those of the assistant. The introduction of advanced equipment and technical modifications has obscured the concept of an essential triangulation in favor of LESS surgery.14 To achieve optimal dissection and triangulation, we have to use articulating instruments.
Needlescopic instruments partially overcome the main limitation of LESS surgery, namely the lack of instrument triangulation.4 Needlescopic instruments can be easily inserted directly in the abdominal wall through a very small skin incision without the need for abdominal trocar placement and closure of the incision. Using these instruments prevents conversion of the procedure to conventional laparoscopic surgery and frees up one access port in the main abdominal multichannel port that can be used to house other necessary instruments. Additionally, needlescopic-assisted LESS-A potentially diminishes the steep learning curve of conventional LESS-A, even in difficult cases such as the transumbilical approach or pheochromocytoma, since it resembles conventional laparoscopic surgery.4 We used 2-mm needlescopic instruments in our series, which do not require an incision for insertion and do not leave a puncture site scar after the operation. Needlescopic-assisted LESS-A does not compromise the cosmetic outcome in the slightest, which is still considered the main advantage of LESS-A over conventional laparoscopic adrenalectomy.
There were some limitations to this study. The small sample size (52 patients) makes it impossible to state any general conclusion. No studies have compared needle-assisted LESS surgery with conventional LESS surgery. A more extensive randomized comparison between needle-assisted LESS surgery and conventional LESS surgery using tools designed to detect differences in morbidity and to assess cosmetic benefits will ultimately determine the future of LESS surgery.15 Moreover, at this time, needlescopic instruments do not provide enough holding strength, do not have a rotation function, and require more effort and concentration to manipulate because of the small jaw. However, even with these limitations, the instruments provided powerful support during our series and should be particularly helpful for beginners at LESS surgery.
We believe that continuing advances in LESS technology will improve this procedure in the near future.16 LESS surgery still needs to be explored with greater consideration of related ethical and methodological issues. Ultimately, needle-assisted LESS-A was performed safely, and avoided many of the difficulties of LESS surgery.
5. Conclusion
Needle-assisted LESS-A is a technically feasible and safe procedure that overcomes many of the technical difficulties of conventional LESS surgery, especially in complex cases. Our main finding in this study is that the insufflation time of needle-assisted LESS-A was significantly shorter than that of conventional LESS-A. In the near future, prospective and randomized long-term follow-up data are needed to establish whether needle-assisted LESS-A should be the standard option for adrenalectomy.
References
- 1 G. Guazzoni, A. Cestari, F. Montorsi, et al.; Current role of laparoscopic adrenalectomy; Eur Urol, 40 (2001), pp. 8–16
- 2 R. Autorino, J.A. Cadeddu, M.M. Desai, et al.; Laparoendoscopic single-site and natural orifice transluminal endoscopic surgery in urology: a critical analysis of the literature; Eur Urol, 56 (2011), pp. 26–45
- 3 J.H. Kaouk, R. Autorino, F.J. Kim, et al.; Laparoendoscopic single-site surgery in urology: worldwide multi-institutional analysis of 1,076 cases; Eur Urol, 60 (2011), pp. 998–1005
- 4 S. Inoue, K. Ikeda, M. Kajiwara, J. Teishima, A. Matsubara; Laparoendoscopic single-site adrenalectomy sans transumbilical approach: initial experience in Japan; Urol J, 11 (2014), pp. 1172–1176
- 5 E. Liatsikos, I. Kyriazis, P. Kallidonis, M. Do, A. Dietel, J.U. Stolzenburg; Pure single-port laparoscopic surgery or mix of techniques?; World J Urol, 30 (2012), pp. 581–587
- 6 M. Zacharias, A. Haese, A. Jurczok, J.U. Stolzenburg, P. Fornara; Transperitoneal laparoscopic adrenalectomy: Outline of the preoperative management, surgical approach, and outcome; Eur Urol, 49 (2006), pp. 448–459
- 7 L.R. McCauley, M.M. Nguyen; Laparoscopic radical adrenalectomy for cancer: Long-term outcomes; Curr Opin Urol, 18 (2008), pp. 134–138
- 8 W.K. Han, Y.H. Park, H.G. Jeon, et al.; The feasibility of laparoendoscopic single-site nephrectomy: initial experience using home-made single-port device; Urology, 76 (2010), pp. 862–865
- 9 L. Cindolo, S. Gidaro, F. Neri, F.R. Tamburro, L. Schips; Assessing feasibility and safety of laparoendoscopic single-site surgery adrenalectomy: initial experience; J Endourol, 24 (2010), pp. 977–980
- 10 S. Inoue, K. Ikeda, K. Kobayashi, M. Kajiwara, J. Teishima, A. Matsubara; Patient-reported satisfaction and cosmesis outcomes following laparoscopic adrenalectomy: laparoendoscopic single-site adrenalectomy vs. conventional laparoscopic adrenalectomy; Can Urol Assoc J, 8 (2014), pp. E20–E25
- 11 A. Miyajima, S. Hattori, T. Maeda, et al.; Transumbilical approach for laparo-endoscopic single-site adrenalectomy: initial experience and short-term outcome; Int J Urol, 19 (2012), pp. 331–335
- 12 X. Zhang, T.P. Shi, H.Z. Li, X. Ma, B.J. Wang; Laparo-endoscopic single site anatomical retroperitoneoscopic adrenalectomy using conventional instruments: initial experience and short-term outcome; J Urol, 185 (2011), pp. 401–406
- 13 S.H. Ju, D.G. Lee, J.H. Lee, et al.; Laparoendoscopic single-site pyeloplasty using additional 2-mm instruments: a comparison with conventional laparoscopic pyeloplasty; Korean J Urol, 52 (2011), pp. 616–621
- 14 D. Canes, M.M. Desai, M. Aron, et al.; Transumbilical single-port surgery: evolution and current status; Eur Urol, 54 (2008), pp. 1020–1029
- 15 M.M. Desai, A.K. Berger, R. Brandina, et al.; Laparoendoscopic single-site surgery: initial hundred patients; Urology, 74 (2009), pp. 805–812
- 16 L. Cindolo, F. Berardinelli, R. Bellocci, L. Schips; Laparoendoscopic single-site unclamped nephron-sparing surgery: a case report; Eur Urol, 60 (2010), pp. 591–594
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?