Summary
Background
Nonpolypoid colorectal neoplasm has been widely recognized in the past few years. Among nonpolypoid colorectal neoplasms, laterally spreading tumor (LST) is a unique and distinct category in that the tumor grows horizontally with a size >1 cm. It may be easily overlooked during colonoscopy. If the size of the colorectal LST is >2 cm, achieving definite management is also another concerning issue. The aim of this study was to improve our understanding of LST by reviewing its clinical manifestations.
Methods
All the large colorectal LSTs that were diagnosed and managed at our hospital in the past 2 years were reviewed. Basic demographic data were recorded. LSTs were divided into granular (G) and nongranular types (NG), then further subdivided into nodular mixed and homogeneous types for the G group and flat elevated and pseudodepressed types for the NG group.
Results
A total of 28 LST in 28 patients were enrolled, with males being more predominant than females (male/female: 18/10). Mean age of the patients and mean size of the LST were 62.6 ± 9.75 years and 3.4 ± 1.257 cm, respectively. Concerning morphology, 14 were diagnosed as NG and 14 as G group. The rate of malignant change was 28.6% (8/28). Twenty-three of our patients received endoscopic treatment (5 for endoscopic piecemeal mucosal resection 18 for endoscopic submucosal dissection) and five for laparoscopy-assisted colectomy. The cost and length of admission analysis between the endoscopic and operation treatment groups showed significant cost reduction (endoscopy/operation: NTD 28172/82516, p < 0.001) and fewer admission days in the endoscopy therapy group (4.74/9.00, days, p < 0.001). Subgroup comparison between the G and NG groups did not reveal statistical significance in age, sex ratio, tumor size, rate of malignant change, or location.
Conclusion
Although long-term outcome comparison was lacking, endoscopic treatment should be considered firstly for colorectal LST under the consideration of shorter hospitalization. Most of our analyses between the G and NG groups were statistically insignificant, which is likely to be due to the small population base.
Keywords
Colorectal laterally spreading tumor ; Endoscopic mucosal resection ; Endoscopic submucosal dissection ; Nonpolypoid colorectal neoplasm
Introduction
Nonpolypoid colorectal neoplasms have been well reported and gradually acknowledged in countries outside Japan. The laterally spreading tumor (LST), defined as a lesion with horizontal growth over 1 cm and relatively limited vertical growth, is a unique endoscopic morphology among nonpolypoid colorectal neoplasms [1] . It also tends to be different from other colorectal neoplasms in genetics analysis [2] ; [3] . There are two morphology classifications for colorectal LST: granular (G) type and nongranular (NG) type. These groups can be further subclassified into homogeneous (HM) and nodular mixed (NM) types for LST-G and flat-elevated (FE) and pseudodepressed (PD) types for LST-NG [1] . These different subclassifications have their own clinicopathological manifestations and may need different treatment strategies. For sizes <2 cm, endoscopic resection should be the mainstay treatment. If the size of LST in the colorectum is >2 cm, endoscopic resection becomes more difficult and challenging. An operation would be suggested for lesions with a larger size, although endoscopic mucosal resection (EMR) and a newly developed technique, endoscopic submucosal dissection (ESD), have become gradually utilized for large LST resection [4] ; [5] ; [6] ; [7] ; [8] . The clinical manifestations and management have seldom been reported in Taiwan. Here, we reviewed our colorectal LST cases with a size over 2 cm during the past 2 years and analyzed the cost and days of hospitalization between operation and endoscopic management.
Methods
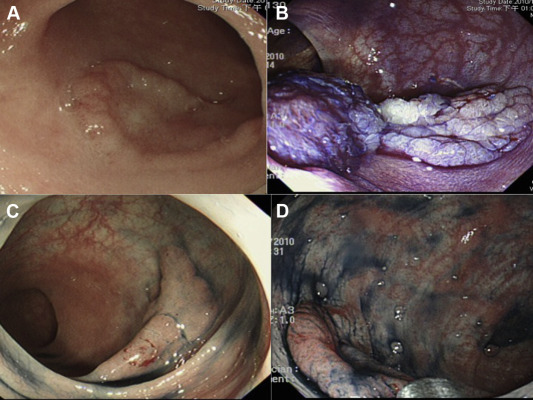
We reviewed our endoscopic electronic report system from July 2010 to August 2012. LSTs with size over 2 cm were selected. Demographic data about age, sex, polyp location and size were identified. All the LST were subgrouped as G and NG types according to the endoscopic morphology. The G group was subclassified into: HM type (Fig. 1 A) if the granular pattern was uniform; and NM type (Fig. 1 B) if a big nodular lesion was noted. The NG group was subclassified into: FE type (Fig. 1 C) if the lesion was flat and evenly raised; and PD type (Fig. 1 D) if a slight central depression was detected. If an initial endoscopic morphology was not given, the endoscopic pictures were reviewed and classified according to the above definition. According to the management, patients were further divided into operation and endoscopic groups. EMR, endoscopic piecemeal mucosal resection (EPMR), and ESD were endoscopic methods used in the endoscopic management group. We began to perform colorectal ESD in July 2010. During the early stages, we fully explained the risks and benefits of each management to patients when a lesion over 2 cm in size was identified. Some patients, therefore, chose an operation as management for their colorectal LST. As our ESD technique improves, it has gradually become the first treatment choice for en-bloc resection. If the pathology disclosed intramucosal carcinoma or T1 above, the tumor was regarded as malignant. Because some of our patients diagnosed as colorectal LST were admitted initially for other purposes, days of hospitalization were calculated from the day prior to endoscopic therapy to the day patients were discharged. We reviewed patients' medical costs according to the cost reported to the National Health Insurance system (NHI), regardless of the fees paid by patients themselves. Due to the hospital policy, patients treated as ESD were not charged extra fees.
|
|
|
Figure 1. (A) Homogeneous and (B) nodular mixed subtypes of granular laterally spreading tumors; (C) flat-elevated and (D) pseudodepressed subtypes in nongranular laterally spreading tumors. |
Statistical analysis
Variable comparison between the G and NG groups was analyzed by Chi-square test. Two-sample t test was utilized to analyze cost and length of hospitalization between patients who received endoscopic and surgical management. Statistical analysis was conducted by PASW Statistics version 18.0 for Windows (SPSS Inc., Chicago, IL, USA). A p value <0.05 was defined as the level of statistical significance.
Results
A total of 28 patients with 28 colorectal LSTs were enrolled for analysis. Males had a percentage of 64.3% with a mean ± standard deviation age of 62.6 ± 9.75 years. Mean lesion size was 3.4 ± 1.257 cm with a rate of malignancy of 28.6% (8/28, 2 for T1 cancer, 6 for intramucosal carcinoma). The numbers of G and NG were equal (G/NG: 14/14). Regarding the subclassification, the numbers for HM, NM, FE, and PD were seven, seven, 13, and one, respectively. Twenty-three (82.1%) of our patients chose endoscopic resection as their management (Table 1 ). The en-bloc resection rate in our ESD group was 83.3% (15/18) with R0 resection to 77.8% (14/18). A perforation case occurring in the very early period of our colorectal ESD was referred for surgical management, and discharged uneventfully. No delayed bleeding or delayed perforation occurred. Furthermore, no major comorbidities were noted in any of our patients. There was no statistical significance between the G and NG groups in terms of male–female ratio, age, lesion size, lesion location, or malignancy rate ( Table 2 ). In the subgroup analysis, the NM and PD groups had a trend with a more malignant change when compared with the HM and FE groups, respectively, although neither difference was statistically significant (NM/HM: 57.1%/14.3%, p = 0.266; PD/FE: 100%/15.4%, p = 0.214). The endoscopic management group had significantly less medical costs (p < 0.001) and fewer admission days (p < 0.001) than the operation group ( Table 3 ).
| Total | |
|---|---|
| Male ratio, % | 64.3 (18/28) |
| Age, mean (±SD) | 62.6 (±9.75) |
| Lesion size, cm (±SD) | 3.4 (±1.257) |
| Morphology, granular ratio, % | 50 (14/28) |
| Subclassification, HM/NM/FE/PD | 7/7/13/1 |
| Rate of malignancy, % | 28.6 (8/28) |
| Endoscopic management, % | 82.1 (23/28) |
| Proximal location, % | 57.4 (16/28) |
FE = flat elevated; HM = homogeneous; NM = nodular mixed; PD = pseudodepressed; SD = standard deviation.
| Granular | Nongranular | p | |
|---|---|---|---|
| Male ratio, % | 78.61 (11/14) | 59 (7/14) | 0.237 |
| Age, mean (±SD) | 64.64 (±8.785) | 60.5 (±10.537) | 0.269 |
| Lesion size, cm (±SD) | 3.71 (±1.267) | 3.07 (±1.207) | 0.181 |
| Rate of malignancy, % | 35.7 (5/14) | 21.4 (3/14) | 0.252 |
| Subclassification rate of malignancy | NM/HM: 57.1%/14.3%, p = 0.266 | PD/FE: 100%/15.4%, p = 0.214 | |
| Proximal location, % | 71.4 (10/14) | 42.9 (6/14) | 0.676 |
FE = flat elevated; HM = homogeneous; NM = nodular mixed; PD = pseudodepressed; SD = standard deviation.
| Surgical, n = 5 | Endoscopic, n = 23 | p | |
|---|---|---|---|
| Days of hospitalization (±SD) | 9 (±2.550) | 4.74 (±2.320) | <0.001 |
SD = standard deviation.
Discussion
Our endoscopic procedures for colorectal LST included EMR, EPMR, and ESD. As mentioned above, the management chosen did not fully conform to the Japanese criteria. In Japan, the choice of EMR or ESD depends on the LST morphology classification [9] . LST-G and LST-NG may have different gastrointestinal phenotype and genotype [10] ; [11] . Because of the higher risk of multiple minute invasions, ESD is recommended for all LST-NG to get en-bloc resection for thorough pathological examination [9] . If EMR for LST-G with NM type is performed, the nodular structure should be removed firstly because it carries a higher risk of malignant change [9] . According to Japan’s colorectal ESD standardization implementation working group, ESD is indicated for lesions over 20 mm and difficult-to-obtain en-bloc resection by EMR, lesions with fibrosis, sporadic localized tumors in colon with chronic inflammation, and local residual early carcinoma after endoscopic resection [12] . ESD for colorectal tumors has also been approved by Japans public health insurance system since April 2012. Although the indication of the largest lesion size was refined at 50 mm, the approval by the insurance system validated the feasibility of ESD as the first choice for early colorectal neoplasms (http://recenavi.net/2012/K/K721-4.html , accessed January 13, 2013). By contrast, colorectal ESD is regarded as a difficult technique and should commence after gaining experience of gastric ESD, good colonoscopy manipulation, and diagnostic ability [13] . When comparing with EPMR/EMR, colorectal ESD also carries a longer procedure time and higher complication rate, although it has a lower local recurrence rate and higher en-bloc rate [14] ; [15] . The endoscopic treatment for colorectal LST, regardless of ESD or EMR, should be performed after good training and understanding of these procedures [16] .
The management of endoscopically resected specimen is important. It should be retracted carefully, stretched well, and fixed firmly on a plate. Therefore, the good orientation may make the histological examination more precise. The specimen should be sliced with a 1–2 mm interval. Once the malignancy is diagnosed, the occurrence of invasion to the submucosal layer or the depth of invasion should be clearly defined. If the layer of muscularis mucosa remains, the depth of submucosal invasion is measured from the layer of muscularis mucosa; it should be measured from the tumor surface if the layer of muscularis mucosa is already destroyed by cancer cells [17] . These procedures inevitably increase the workload of the pathology department. The imbalance between the workload and insurance payment may hinder the pathologists to adhere to these steps adequately. Therefore, good communication with the pathologist and an effort to revise the insurance reimbursement are necessary. Any violation against these procedures may result in under-diagnosis of the lesion. Precise and accurate pathological examination could select patients for whom subsequent surgery is necessary to prevent rapid local recurrence. According to the Japanese guidelines, subsequent surgery for lymph node dissection is considered if any one of the following criteria is met: (1) depth of submucosal invasion ≥1000 μm; (2) positive vascular invasion; (3) poorly differentiated adenocarcinoma, signet-ring cell carcinoma, or mucinous carcinoma; or (4) grade 2/3 budding at the site of deepest invasion [18] ; [19] . Subsequent surgery should be highly recommended for patients who meet any one of the above criteria as it is associated with long-term outcome [20] .
Our results show that endoscopic resection for colorectal LST has significantly less medical expense and duration of hospitalization than an operation. However, our cost analysis for the endoscopic group was based on NHI costs, regardless of the fee paid by patients themselves. Endoscopic management, particularly for ESD, is expensive for its instruments and is still not covered by the NHI system. Therefore, the charge for ESD (esophagus, stomach, and colorectum) in Taiwan varies across different hospitals. Colorectal ESD has been fully included in Japans insurance system since April 2012. It was firstly approved as an “advanced medical treatment” system, which is a partial-care service provided by the Japanese public health insurance with individual payment of medical expenses [12] . Since then, the actual medical expenses reported to the insurance system have increased [21] . EMR for gastrointestinal tract polyp over 2 cm, malignant lesion or submucosal tumor has been approved by Taiwans NHI system since 2013. The actual discrepancy of medical expenses between surgical treatment and EMR would be clearly seen in the future. Moreover, due to the foreseeable growing numbers of endoscopic treatment, a large-scale study on the comparison among surgical management, ESD, and EMR would be feasible in Taiwan.
Our results fail to show any significant difference of malignant change rate among each subclassifications, probably due to our small population. Although not statistically significant, the result of higher malignancy rate in the NM and PD type groups was similar to other studies [10] ; [22] ; [23] . To improve our understanding of colorectal LST in Taiwan, a multicenter study is necessary.
Although an increasing amount of studies, not only from Japan but also Asian and European countries, have shown that colorectal ESD could be a safe procedure for colorectal neoplasms [24] ; [25] . ESD is still regarded as a difficult, time-consuming, and risky procedure and needs a long learning curve [26] . A multicenter study conducted by Moss et al [27] also showed that EMR could be safe and effective for large sessile colonic polyps. Therefore, the endoscopic choices between ESD and EMR for colorectal LST should depend on the characteristics of the lesions, technique of the endoscopists, and even on the insurance reimbursement system. Given the marked reduction in days of hospitalization and safety, endoscopic treatment for large colorectal LST should be initially considered for every patient without a high risk of deep submucosal invasion and/or risk of lymph node metastasis.
Conflicts of interest
All authors declare no conflicts of interest.
References
- [1] S. Kudo, R. Lambert, J.I. Allen, H. Fujii, T. Fujii, H. Kashida, et al.; Nonpolypoid neoplastic lesions of the colorectal mucosa; Gastrointest Endosc, 68 (4 Suppl.) (2008), pp. S3–47
- [2] A. Noro, T. Sugai, W. Habano, S. Nakamura; Analysis of Ki-ras and p53 gene mutations in laterally spreading tumors of the colorectum; Pathol Int, 53 (2003), pp. 828–836
- [3] S. Hiraoka, J. Kato, M. Tatsukawa, K. Harada, H. Fujita, T. Morikawa, et al.; Laterally spreading type of colorectal adenoma exhibits a unique methylation phenotype and K-ras mutations; Gastroenterology, 131 (2006), pp. 379–389
- [4] D.P. Hurlstone, D.S. Sanders, S.S. Cross, I. Adam, A.J. Shorthouse, S. Brown, et al.; Colonoscopic resection of lateral spreading tumours: a prospective analysis of endoscopic mucosal resection; Gut, 53 (2004), pp. 1334–1339
- [5] O. Urban, P. Vitek, P. Fojtik, M. Kliment, D. Janik, J. Chalupa, et al.; Laterally spreading tumors—experience based on 138 consecutive cases; Hepatogastroenterology, 55 (2008), pp. 351–355
- [6] Y. Saito, T. Uraoka, Y. Yamaguchi, K. Hotta, N. Sakamoto, H. Ikematsu, et al.; A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video); Gastrointest Endosc, 72 (2010), pp. 1217–1225
- [7] T. Toyonaga, M. Man-i, T. Fujita, J.E. East, E. Nishino, W. Ono, et al.; Retrospective study of technical aspects and complications of endoscopic submucosal dissection for laterally spreading tumors of the colorectum; Endoscopy, 42 (2010), pp. 714–722
- [8] N. Yoshida, N. Yagi, Y. Naito, T. Yoshikawa; Safe procedure in endoscopic submucosal dissection for colorectal tumors focused on preventing complications; World J Gastroenterol, 16 (2010), pp. 1688–1695
- [9] T. Uraoka, Y. Saito, T. Matsuda, H. Ikehara, T. Gotoda, D. Saito, et al.; Endoscopic indications for endoscopic mucosal resection of laterally spreading tumours in the colorectum; Gut, 55 (2006), pp. 1592–1597
- [10] B.C. Kim, H.J. Chang, K.S. Han, D.K. Sohn, C.W. Hong, J.W. Park, et al.; Clinicopathological differences of laterally spreading tumors of the colorectum according to gross appearance; Endoscopy, 43 (2011), pp. 100–107
- [11] K. Nakae, H. Mitomi, T. Saito, M. Takahashi, T. Morimoto, Y. Hidaka, et al.; MUC5AC/beta-catenin expression and KRAS gene alteration in laterally spreading colorectal tumors; World J Gastroenterol, 18 (2012), pp. 5551–5559
- [12] S. Tanaka, M. Terasaki, H. Kanao, S. Oka, K. Chayama; Current status and future perspectives of endoscopic submucosal dissection for colorectal tumors; Dig Endosc, 24 (Suppl. 1) (2012), pp. 73–79
- [13] K. Ohata, T. Ito, H. Chiba, Y. Tsuji, N. Matsuhashi; Effective training system in colorectal endoscopic submucosal dissection; Dig Endosc, 24 (Suppl. 1) (2012), pp. 84–89
- [14] A. Repici, C. Hassan, D. De Paula Pessoa, N. Pagano, A. Arezzo, A. Zullo, et al.; Efficacy and safety of endoscopic submucosal dissection for colorectal neoplasia: a systematic review; Endoscopy, 44 (2012), pp. 137–150
- [15] T. Toyonaga, M. Man-i, J.E. East, E. Nishino, W. Ono, T. Hirooka, et al.; 1,635 Endoscopic submucosal dissection cases in the esophagus, stomach, and colorectum: complication rates and long-term outcomes; Surg Endosc, 27 (2013), pp. 1000–1008
- [16] S. Tanaka, M. Terasaki, N. Hayashi, S. Oka, K. Chayama; Warning for unprincipled colorectal endoscopic submucosal dissection: accurate diagnosis and reasonable treatment strategy; Dig Endosc, 25 (2013), pp. 107–116
- [17] K. Kitajima, T. Fujimori, S. Fujii, J. Takeda, Y. Ohkura, H. Kawamata, et al.; Correlations between lymph node metastasis and depth of submucosal invasion in submucosal invasive colorectal carcinoma: a Japanese collaborative study; J Gastroenterol, 39 (2004), pp. 534–543
- [18] T. Watanabe, M. Itabashi, Y. Shimada, S. Tanaka, Y. Ito, Y. Ajioka, et al.; Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2010 for the treatment of colorectal cancer; Int J Clin Oncol, 17 (2012), pp. 1–29
- [19] H. Ueno, H. Mochizuki, Y. Hashiguchi, H. Shimazaki, S. Aida, K. Hase, et al.; Risk factors for an adverse outcome in early invasive colorectal carcinoma; Gastroenterology, 127 (2004), pp. 385–394
- [20] H. Ikematsu, Y. Yoda, T. Matsuda, Y. Yamaguchi, K. Hotta, N. Kobayashi, et al.; Long-term outcomes after resection for submucosal invasive colorectal cancers; Gastroenterology, 144 (2013), pp. 551–559 quiz e514
- [21] Y. Takeuchi, T. Ohta, F. Matsui, K. Nagai, N. Uedo; Indication, strategy and outcomes of endoscopic submucosal dissection for colorectal neoplasm; Dig Endosc, 24 (Suppl. 1) (2012), pp. 100–104
- [22] S. Oka, S. Tanaka, H. Kanao, S. Oba, K. Chayama; Therapeutic strategy for colorectal laterally spreading tumor; Dig Endosc, 21 (Suppl. 1) (2009), pp. S43–S46
- [23] M.D. Xu, X.Y. Wang, Q.L. Li, P.H. Zhou, Y.Q. Zhang, Y.S. Zhong, et al.; Colorectal lateral spreading tumor subtypes: clinicopathology and outcome of endoscopic submucosal dissection; Int J Colorectal Dis, 28 (2013), pp. 63–72
- [24] S. Farhat, S. Chaussade, T. Ponchon, D. Coumaros, A. Charachon, T. Barrioz, et al.; Endoscopic submucosal dissection in a European setting. A multi-institutional report of a technique in development; Endoscopy, 43 (2011), pp. 664–670
- [25] Y. Saito, H. Kawano, Y. Takeuchi, K. Ohata, S. Oka, K. Hotta, et al.; Current status of colorectal endoscopic submucosal dissection in Japan and other Asian countries: progressing towards technical standardization; Dig Endosc, 24 (Suppl. 1) (2012), pp. 67–72
- [26] H.M. Chiu, J.T. Lin; Clinical application and standardization of colorectal endoscopic submucosal dissection: is it a viable approach?; J Gastroenterol Hepatol, 28 (2013), pp. 391–393
- [27] A. Moss, M.J. Bourke, S.J. Williams, L.F. Hourigan, G. Brown, W. Tam, et al.; Endoscopic mucosal resection outcomes and prediction of submucosal cancer from advanced colonic mucosal neoplasia; Gastroenterology, 140 (2011), pp. 1909–1918
Document information
Published on 15/05/17
Submitted on 15/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?