Summary
Hypophysitis is a rare inflammatory disorder that can mimic a pituitary tumor clinically or radiologically. Furthermore, immunoglobulin G4 (IgG4)-related systemic disease is only a just recently characterized disorder. It can manifest as a systemic disease involving multiple organs, including the pancreas, salivary glands, lungs, liver, bile duct, gallbladder, kidneys, and retroperitoneum. It is characterized by a high serum level of IgG4 clinically and dense lymphoplasmacytic infiltration with sclerosis and phlebitis histologically. Herein, we report the case of a man 66 years of age who presented with nausea, vomiting, and poor appetite with a body weight loss of 4 kg. Image study revealed a pituitary infundibulum mass, right-posterior mediastinal and paraspinal masses, as well as infiltrating masses in bilateral kidneys. Therefore, he received a thoracoscopic biopsy for the right-posterior mediastinal and paraspinal masses and a pathologic examination reported an IgG4-related inflammatory pseudotumor. Then, transsphenoidal removal of the infundibulum mass was performed. Histologically, the infundibulum mass represented a IgG4-related hypophysitis manifested as an infiltration of plasma cells, lymphocytes, histiocytes, and some eosinophils with a fair number of IgG4-immunoreactive plasma cells. After the operation was complete, the patient took 5 mg of prednisolone every 2 days for 3 months. A follow-up computed tomography scan revealed improvement of the infiltrating masses in the bilateral kidneys.
Keywords
hypophysitis;hypopituitarism;IgG4-related disease;inflammatory pseudotumor
1. Introduction
Immunoglobulin G4 (IgG4)-related sclerosing disease is a recently identified entity. Pancreatic involvement is the most common manifestation. However, other systemic involvement has also been reported, including the hepatobiliary tract, salivary glands, orbit, lymph nodes, retroperitoneum, aorta, mediastinum, soft tissue, skin, the central nervous system, breasts, kidneys, prostate, upper aerodigestive tract, and lungs.1 ; 2 Hypophysitis is a rare inflammatory disorder and IgG4-related sclerosing disease involving the pituitary glands is especially rare.1 Imaging studies may reveal a mass lesion in the sellar area or a thickening of pituitary stalk, mimicking a pituitary tumor. Clinically, most patients present with hypopituitarism, diabetes insipidus, and/or a local mass effect. Serum IgG4 level is always elevated.3 Histopathologically, IgG4-related sclerosing disease is characterized by dense lymphoplasmacytic infiltration, stromal sclerosis, and the presence of phlebitis.1 Immunohistochemical study can demonstrate increased IgG4-positive plasma cells. In our current report, we describe an elderly Chinese man diagnosed with IgG4-related hypophysitis associated with multiple organ involvement but who lacked pancreatitis. His clinical manifestation improved dramatically after he received steroid treatment.
2. Case report
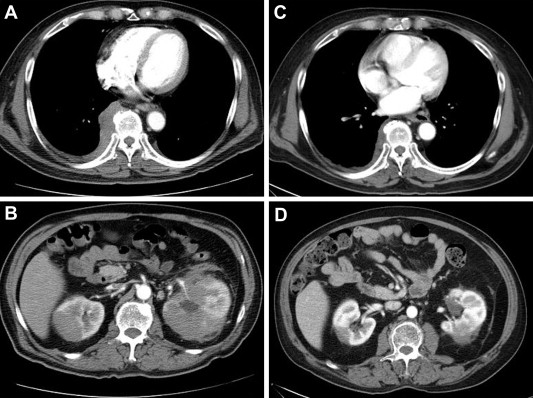
A man aged 66 years presented with nausea, vomiting, poor appetite, and body weight loss of 4 kilograms in 1 month. He had a history of acute cholecystitis status postcholecystectomy and chronic hypertrophic rhinitis. Anorexia and fatigue were also noted. His condition did not improve after he asked help from the Show Chwan Memorial Hospital Changhua, Taiwan and a postmediastinal mass with diffuse mediastinal lymph node enlargement was revealed by chest computed tomography (CT) scan. Then, he was transferred to our hospital. Physical examination revealed no specific findings. The chest CT scan demonstrated a 2.4-cm nodule in the right middle lobe abutting the right pericardial pleura and an infiltrating right-posterior mediastinal and paraspinal masses with pleural extension (Fig. 1A). No extension to bone or intraspinal canals was noted. There were multiple mediastinal lymph node enlargements, with the largest being a diameter of about 17 mm in the aortopulmonary window (AP) window region. In addition, bilateral infiltrating masses were noted in the upper kidney level (Fig. 1B). The stomach also demonstrated focal thickening of the wall over the lesser curvature side.
|
|
|
Figure 1. (A) Infiltrating right posterior mediastinal and paraspinal masses with pleural extension; (B) bilateral infiltrating masses in both kidneys; (C) after steroid treatment, there was a significant decrease in the size of the previously noted nodule in the posterior mediastinal and right paraspinal masses, (D) as well as in the prior infiltrating masses in both kidneys. |
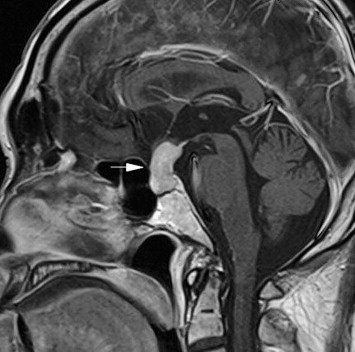
The patient first received a thoracoscopic biopsy, and a pathologic examination reported an inflammatory pseudotumor, suggestive of IgG4-related sclerosing disease. After thoracoscopic biopsy, his condition still did not improve and laboratory tests revealed eosinophilia (7.9%), a low testosterone level (<0.008 ng/ml; reference range, 1.66–8.11 ng/ml) and primary hypoadrenalism with a low cortisol level (0.65 μg/dl before 10 am; reference range, 4.46–22.69 μg/dl) and an elevated adrenocorticotropic hormone (ACTH) level (56.1 pg/ml; reference range, <46 pg/ml), but other pituitary hormones were within the normal range. The brain magnetic resonance imaging (MRI) demonstrated a 2.4-cm, well-defined mass in the sella turcica, showing isointense on a T1- and T2-weighted image with strong enhancement after injection of the contrast medium (Fig. 2). No residual normal pituitary tissue of the posterior lobe was noted. The mass lesion extended upward and compressed the optic chiasm. Macroadenoma was initially suspected. Then, he commenced glucocorticoid replacement therapy and received transsphenoidal removal of the infundibulum mass.
|
|
|
Figure 2. Well-defined mass in the sella turcica with strong enhancement after the injection of contrast medium. |
After the operation, the patient kept taking 5 mg of prednisolone every 2 days for 3 months and a follow-up CT scan revealed a significant decrease in the size of the previously noted nodule in right middle lobe, posterior mediastinal and right paraspinal masses (Fig. 1C) and prior infiltrating masses in both kidneys (Fig. 1D).
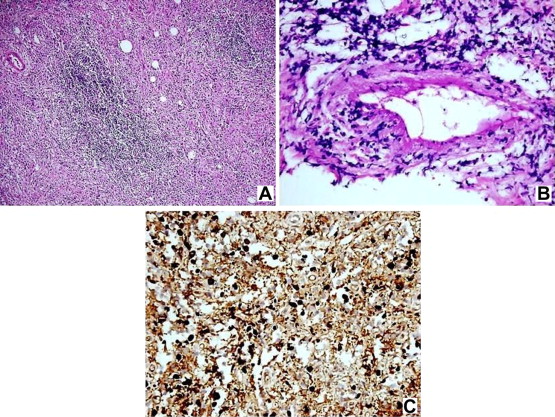
The received specimen of the thoracoscopic biopsy consisted of one tissue fragment measuring 1.3 × 0.6 × 0.2 cm in size. Grossly, it was grayish and firm. Microscopically, the fibrous tissue fragment showed bland-appearing spindle cell proliferation in the fibrotic or sclerotic background with marked infiltration of lymphocytes, plasma cells, as well as eosinophils and focal lymphoid follicle formation (Fig. 3A). Focal vasculitis was also present (Fig. 3B). Immunohistochemistry for the κand λ light chains showed no light chain restriction in these plasma cells. The immunohistochemical study for IgG4 showed abundant positive plasma cells (more than 30 per high power field (400×) HPF). This is shown in Fig. 3C.
|
|
|
Figure 3. (A) Bland-appearing spindle cell proliferation in a fibrotic or sclerotic background with infiltration of lymphocytes, plasma cells, and focal lymphoid aggregates (40×); (B) focal vasculitis is present (400×); (C) abundant IgG4-positive plasma cells (more than 30 per HPF) according to immunohistochemical study (400×). HPF = high power field (400×); Ig = immunoglobulin. |
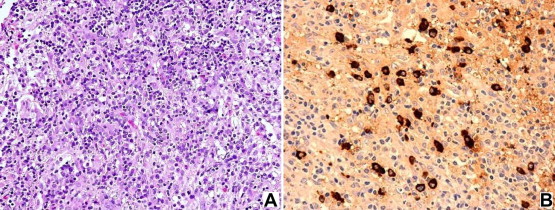
Seven tiny pieces of tan-soft tissue specimens, measuring up to 0.2 × 0.1 × 0.1 cm in size, werereceived for pathologic examination. Microscopic examination revealed the specimen consisted mainly of neurohypophysial tissue by lymphocytes, plasma cells, and eosinophils with stromal edema and mild fibrosis (Fig. 4A). The reticulin highlighted a fragment of adenohypophysial tissue.The immunohistochemical study of the IgG4 stain highlighted a fair number of IgG4 immunoreactive plasma cells (Fig. 4B). Taken together, IgG4-related hypophysitis was diagnosed.
|
|
|
Figure 4. (A) Specimen mainly consisting of neurohypophysial tissue by lymphocytes, plasma cells, and eosinophils with stromal edema and mild fibrosis (100×); (B) a fair number of IgG4 immunoreactive plasma cells according to immunohistochemical study (400×). Ig = immunoglobulin. |
3. Discussion
In 1961, Sarles and colleagues1 first raised the concept that some cases of chronic pancreatitis resulted from an autoimmune etiology. In 1995, Yoshida and coworkers 4 introduced the term “autoimmune pancreatitis (AIP)”, characterized by mass lesions in the pancreas, narrowing of the pancreatic duct, painless obstructive jaundice, and favorable response to steroid therapy. In 2001, Hamano and others5 first found elevated serum IgG4, increased IgG4-positive plasma cells, and lymphoplasmacytic sclerosing change in a specific subtype of sclerosing pancreatitis. Then, a distinct subtype of AIP, named “IgG4-related sclerosing pancreatitis,” was designated. However, other sites of involvement have subsequently also been noted, including hepatobiliary tract, salivary glands, orbit, lymph nodes, retroperitoneum, aorta, mediastinum, soft tissues, lymph nodes, bone marrow, skin, the central nervous system, breasts, kidneys, prostate, upper aerodigestive tract, and lungs.1 ; 2 For this reason, the concept of the IgG4-related systemic disease was proposed. IgG4-related sclerosing disease is defined as a systemic syndrome and characterized by mass-forming lesions clinically. The histologic triad includes lymphoplasmacytic infiltrates, sclerosis, and obliterative phlebitis.1 There are numerous IgG4-positive plasma cells in the affected tissues, and the serum IgG4 level is also increased.3 Most IgG4-related sclerosing diseases occur with AIP, but some lacking pancreatic involvement have also been reported.6 These diseases predominantly affect elderly men and, clinically, such patients generally respond well to steroid treatment.
IgG4-related sclerosing disease involving the central nervous system is very rare and the pituitary gland is the most commonly reported site.1 To date, only 25 cases (including the present case) have been reported.6; 7 ; 8 There were 23 men and two women patients with an obvious male predominance. The age of the patients ranged from 42–77 years of age with a mean age of 64.76 years. Most patients presented with hypopituitarism, diabetes insipidus (DI), and/or a local mass effect. Serum IgG4 were all elevated during the active stage if checked. Most cases were associated with other systemic involvement. Some cases had concomitant pachymeningitis or parasinusitis with extension to sellar and parasellar structures.1 ; 6 Only one patient was manifested as an isolated pituitary lesion.6 Most patients were diagnosed by clinical correlation and imaging, while only six cases had been proven through pathologic examination.
Imaging study often reveals a thickening or mass formation on the pituitary stalk and the thickening may occur up to the level of infundibulum. Sometimes, it may present as a swelling of pituitary gland or a mass formation in the pituitary gland.
The diagnostic criteria for IgG4-related sclerosing disease is still a controversy issue since there are a variety of diagnostic criteria for AIP that have been proposed by different groups. In addition, an agreement has still not been reached on the cut-off number of IgG4+ plasma cells. A number greater than 30 per high-power field has been reported to be reasonably specific,1 while Dhall and colleagues9 recently suggested diffuse and dense infiltrate of IgG4+ cells, numbering more than 50 per high-power field, to be of high specificity. Afterward, Wah and others1 proposed the histologic criteria of IgG4-related sclerosing disease, including absolute number of IgG4+ cells > 50/HPF, percentage of IgG4+/IgG+ cells >40%, and characteristic morphology, such as lymphoplasmacytic infiltration ± lymphoid follicles, sclerosis, and phlebitis.
The pathogenesis of IgG4-related sclerosing disease is still under intense investigation.6 It has been believed that autoimmune mechanism plays a role in this condition. First of all, serum IgG as well as IgG4 levels are often elevated and most patients show a good clinical response to corticosteroid treatment.2 ; 6 It is also reported that possession of a particular HLA genotype (HLA DRB1*0405- DQB1*0401) is related to an increased risk of disease development.2 ; 5 Besides, immune complex deposition has been identified with tissue affected by IgG4-related systemic sclerosing disease ultrastructurally.2 ; 5 It is also known that disease induction occurs due to the development of an immune response to self-antigens and in association with a decrease in naive regulatory T cells in peripheral blood and increased infiltration of memory regulatory T cells in involved tissue. Disease progression results from a switch to a T helper 2 (Th2) response with expression of Th2 cytokines and regulatory cytokines2; 3 ; 5; however, there are no precise triggers identified for initiation to date. Furthermore, the role of IgG4-positive plasma cells is not yet clear. Whether these cells play a role in the development of the disease or solely represent an epiphenomenon and a diagnostically useful marker is still not well understood.
In the presenting case, pathologic examination proved IgG4-related pleuritis and hypophysitis. The imaging study also revealed mass/nodular lesions in the right lung, paraspinal region, and bilateral kidneys, and mediastinal lymph node enlargement, as well as a focal wall thickening of the stomach. After steroid treatment, the regression of all lesions was evidenced by image follow-up. Although a serum IgG4 test was not performed, we suggest the patient manifested with IgG4-related sclerosing disease, complicating hypophysitis, pleuritis, multifocal fibrosclerosis, lymphadenopathy, zonal tubulointerstitial nephritis, gastritis, and pulmonary inflammatory pseudotumor.
References
- 1 W. Cheuk, J.K. Chan; IgG4-related sclerosing disease: a critical appraisal of an evolving clinicopathologic entity; Adv Anat Pathol, 17 (2010), pp. 303–332
- 2 S. Yasuharu, N. Kenji, K. Masaru, T. Katsuyoshi, M. Yasufumi, Y. Tadashi; IgG4-related disease: historical overview and pathology of hematological disorders; Pathol Int, 60 (2010), pp. 247–258
- 3 A.C. Bateman, M.G. Deheragoda; IgG4-related systemic sclerosing disease - an emerging and under-diagnosed condition; Histopathology, 55 (2009), pp. 373–383
- 4 K. Yoshida, F. Toki, T. Takeuchi, S. Watanabe, K. Shiratori, N. Hayashi; Chronic pancreatitis caused by an autoimmune abnormality. Proposal of the concept of autoimmune pancreatitis; Dig Dis Sci, 40 (1995), pp. 1561–1568
- 5 H. Hamano, S. Kawa, A. Horiuchi, et al.; High serum IgG4 concentrations in patients with sclerosing pancreatitis; N Engl J Med, 344 (2001), pp. 732–738
- 6 A. Shimatsu, Y. Oki, I. Fujisawa, T. Sano; Pituitary and stalk lesions (infundibulo-hypophysitis) associated with immunoglobulin G4-related systemic disease: an emerging clinical entity; Endocr J, 56 (2009), pp. 1033–1041
- 7 S. Osawa, Y. Ogawa, M. Watanabe, T. Tominaga; Hypophysitis presenting with atypical rapid deterioration: with special reference to immunoglobulin G4-related disease-case report-; Neurol Med Chir (Tokyo), 49 (2009), pp. 622–625
- 8 M. Hori, N. Makita, T. Andoh, et al.; Long-term clinical course of IgG4-related systemic disease accompanied by hypophysitis; Endocr J, 57 (2010), pp. 485–492
- 9 D. Dhall, A.A. Suriawinata, L.H. Tang, J. Shia, D.S. Klimstra; Use of immunohistochemistry for IgG4 in the distinction of autoimmune pancreatitis from peritumoral pancreatitis; Hum Pathol, 41 (2010), pp. 643–652
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?