Summary
Cytomegalovirus (CMV) infection of the gastrointestinal tract involves mostly the colon and rectum and mainly develops in immunocompromised patients. CMV infection in the small intestines has rarely been reported in immunocompetent patients. We report two cases of CMV enteritis that developed in immunocompetent patients and involved the ileum and jejunum, respectively. Both of them were diagnosed with single-balloon enteroscopy (SBE) and further confirmed with histopathology. The first case is a 71-year-old woman with a presentation of obscure gastrointestinal bleeding and severe anemia. Neither esophagogastroduodenoscopy nor colonoscopy identified any active bleeding. SBE and biopsy disclosed multiple scattered ulcers in the distal ileum and histopathology confirmed CMV ileitis. The hemorrhage subsided after conservative medical treatment. The second case is a 59-year-old woman with a presentation of progressive abdominal pain. SBE showed diffuse irregularly-shaped ulcers located from the upper to middle jejunum, and CMV jejunitis was confirmed with endoscopic biopsy and histopathological examination. Antiviral therapy was prescribed and her abdominal pain improved gradually. We discuss the clinical manifestations and management strategies of CMV infection that develops in the small intestines of immunocompetent patients. In addition, we highlight the endoscopic characteristics of CMV enteritis and the clinical utilities of SBE in the evaluation of patients with suspected CMV infection of the small intestines.
Keywords
Cytomegalovirus ; Enteritis ; Enteroscopy ; Ileitis ; Immunocompetent ; Jejunitis
Introduction
Cytomegalovirus (CMV) infection of the gastrointestinal (GI) tract mostly involves the colon and rectum and mainly develops in immunocompromised hosts, such as patients with human immunodeficiency virus (HIV) infection and AIDS, patients who received solid organ or hematopoietic stem cell transplantation, and patients with inflammatory bowel disease [1] ; [2] . The clinical manifestations of CMV infection of the GI tract are nonspecific [3] , and the endoscopic findings are also variable, ranging from mucosal erythema, discrete ulceration, pseudo-tumor formation, to bowel perforation [1] ; [4] . Endoscopic biopsy with histopathology evaluation and immunochemical staining remains the gold standard for definitive diagnosis [1] .
Recently, CMV infection of the GI tract has been increasingly reported in immunocompetent patients, and the most commonly involved locations are also the colon and rectum [5] . The mortality rate of CMV colitis in immunocompetent patients has been reported to be up to 31.8% [6] . However, CMV infection involving the small intestines in immunocompetent hosts has rarely been reported [7] . Here, we report two cases of CMV enteritis which developed in immunocompetent patients. Both cases were diagnosed with single-balloon enteroscopy (SBE) and confirmed with histopathology.
Case Reports
Case 1
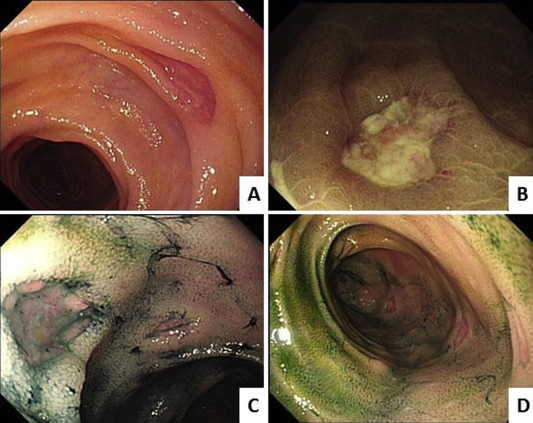
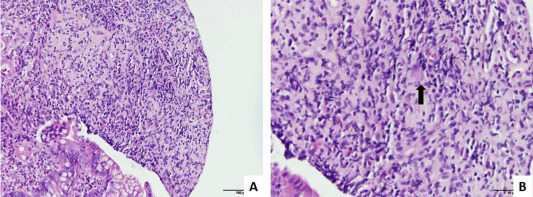
A 71-year-old woman with hypertension, diabetes mellitus (DM), and end stage renal disease (ESRD) under regular hemodialysis was referred to our hospital for obscure gastrointestinal bleeding with intermittent tarry and bloody stool. The physical examination was only remarkable for generalized pallor. Laboratory studies showed a low hemoglobin level of 5.0 g/dL with a mean corpuscular volume of 91.6 fL. Esophagogastroduodenoscopy did not identify any bleeding source and repeated colonoscopy showed only fresh blood in the colon. Intestine-targeted transabdominal ultrasonography disclosed neither mass lesion in the abdomen nor bowel wall abnormality. To investigate a suspected bleeding source in the distal small intestine, we performed SBE (SIF-Q260) with a ST-SB1 splinting tube (Olympus Co., Tokyo, Japan) via the retrograde approach, which showed multiple (∼40–50) 0.3–1.0-cm ulcers scattered over the distal ileum (Figure 1 ). Endoscopic biopsy was done and histopathology showed ulcers with ulcerative debris and granulation tissue. The adjacent villi were mildly blunted but no cryptic distortion or granuloma was found (Figure 2 ). CMV ileitis was confirmed with immunohistochemical staining. HIV serology was negative. Supportive care with component therapy was instituted and her bleeding resolved gradually without further antiviral treatment.
|
|
|
Figure 1. (A) Single-balloon enteroscopy shows multiple 0.3–1.0-cm discrete ulcers scattered over the distal ileum; (B) narrow band imaging shows a well-defined ulcer; (C, D) indigo carmine spray further discloses multiple tiny ulcers over the distal ileum. |
|
|
|
Figure 2. (A) Histopathology shows ulcerative debris and granulation tissue under hematoxylin and eosin stain with ×200 power field; (B) histopathology shows enlarged nucleus with dense inclusion body (arrow) under hematoxylin and eosin stain with ×400 power field. |
Case 2
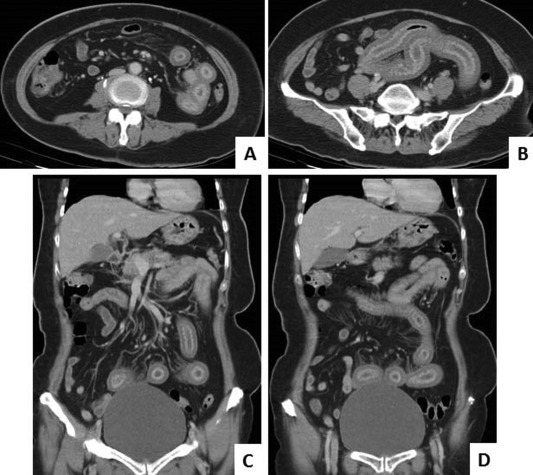
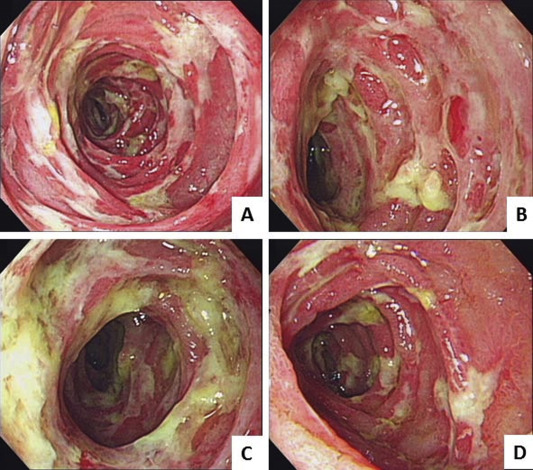
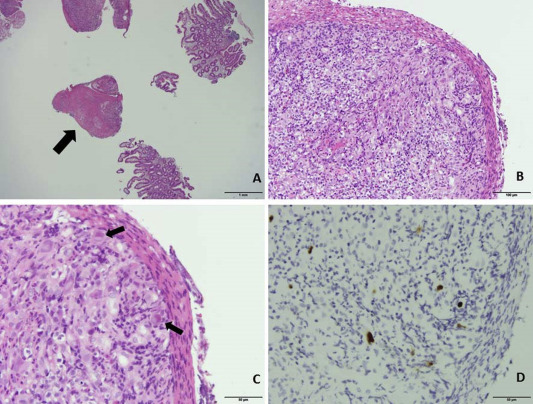
A 59-year-old woman with hypertension and DM presented with progressive abdominal pain over the upper abdomen. Esophagogastroduodenoscopy, colonoscopy, and transabdominal ultrasonography revealed no significant findings. Contrast-enhanced abdominal computed tomography revealed segmental small bowel wall thickening (∼1.0 cm in thickness) with fair mucosal enhancement and engorged mesenteric vessels (Figure 3 ). The small bowel follow-through showed continuous mucosal irregularity and thickening extending from the proximal jejunum to ileum. SBE (SIF-Q260) with ST-SB1 splinting tube (Olympus Co.) via the antegrade approach was performed and showed diffuse irregularly-shaped ulcers with exudative coating and geographic distribution extending from the upper to middle jejunum (Figure 4 ). Biopsy was performed and histopathology showed mucosa ulceration with several nuclear inclusion bodies and positive CMV immunoreactivity (Figure 5 ). CMV jejunitis was confirmed. The serum CMV immunoglobulin-M antibody was negative, immunoglobulin-G antibody was positive, and the serum viral load test detected CMV viremia (2280 copies/mL). Both autoimmune profile and HIV screening test were negative. Antiviral therapy with ganciclovir (250 mg every 12 hours) for 10 days was prescribed, followed by oral valganciclovir (900 mg/d) for 1 month. Her abdominal pain subsided gradually and subsequent serum CMV viral load was undetectable.
|
|
|
Figure 3. (A, B) Coronal view of contrast-enhanced computed tomography reveals segmental small bowel wall thickening with fair mucosal enhancement; (C, D) sagittal view of contrast-enhanced computed tomography also reveals small bowel wall thickening with engorged mesenteric vessels. |
|
|
|
Figure 4. (A–D) Single-balloon enteroscopy shows diffuse irregularly shaped ulcers with exudative coating and geographic distribution extending from the upper to middle jejunum. |
|
|
|
Figure 5. (A) Histopathology shows mucosa ulceration (arrows) under hematoxylin and eosin (H&E) stain with ×20 power field; (B) histopathology shows neutrophil infiltration and granulation tissue (fibrin and neovascularity) under H&E stain with ×100 power field; (C) histopathology shows enlarged nucleus with eosinophilic inclusion body (arrows) under H&E stain with ×400x power field; (D) immunohistochemical stain shows positive cytomegalovirus immunoreactivity. |
Discussion
The diagnosis of CMV infection of the GI tract, especially the small intestines, in immunocompetent hosts is challenging. Among the rarely reported cases in the literature, most present with nonspecific symptoms, including poor appetite, abdominal pain, vomiting, and ileus, and were usually diagnosed with laparotomy for profuse bleeding or bowel perforation [4] ; [7] . Most cases with CMV ileitis over terminal ileum were diagnosed using colonoscopy [2] and only one case of CMV jejunitis was diagnosed with SBE [8] . A high index of clinical suspicion for CMV enteritis and early institution of SBE is necessary to avoid delaying the correct diagnosis.
Endoscopic findings of CMV enterocolitis were mostly reported from immunocompromised patients and those from immunocompetent patients were seldom reported. In a study of 51 HIV patients with CMV colitis, 72.5% showed a heterogeneous ulcerative pattern, 21.6% with inflammatory process of the mucosa, and 5.9% with normal mucosa. The ulceration can be shallow or deep, isolated or covered with fibrin, or present with a hyperemic border [9] . Besides, CMV enterocolitis can also present with pseudo-tumor formation [1] or submucosal tumor with overlying mucosal ulceration [10] . In the literature, only one case has been diagnosed as CMV jejunitis using SBE, which showed multiple geographically-shaped ulcers covered with exudates over the proximal jejunum [8] . Both of our cases showed diffusely scattered ulcers, which were difficult to differentiate endoscopically with enteritis or ulcers arising from other etiologies, such as Crohns disease, and required histopathological for final confirmation.
Risk factors for CMV infection of the small intestine in immunocompetent individuals remain unclear. Previous case reports of CMV involvement of the small intestine in immunocompetent hosts mostly included cases older than 70 years and some of them even had no comorbidity, suggesting age to be an important risk factor [3] ; [6] . In a meta-analysis of CMV colitis, which developed in 44 immunocompetent hosts, defined as absence of congenital or acquired immune deficiency, transplantation, or immunosuppressive medication, the mean age was 61.1 years and 73.3% of patients presented with comorbidities, such as renal failure, DM, and untreated nonhematologic cancer [6] . In another review of 33 immunocompetent patients with CMV enterocolitis, the mean age was 68 years and 75.8% of patients were older than 60 years [3] . Both of our cases were at a relatively old age (71 years and 59 years) and had comorbidities of DM or ESRD under dialysis, which were similar to those individuals described in the literature [6] ; [11] ; [12] . Therefore, these coexisting illnesses, such as endocrinopathies (e.g., DM), lymphoproliferative and nonhematological malignancies, ESRD, autoimmune diseases, and pregnancy may be potential immune-modulating factors in the immunocompetent group, which has some inherent limitations to be well defined [6] ; [12] . With the increasing prevalence of these comorbidities of DM and ESRD in the general population, further studies are warranted to clarify the underlying pathophysiology of CMV diseases in these “immunocompetent” (or “nonimmunocompromised”) but high-risk populations.
Currently, whether antiviral treatment, such as ganciclovir or foscarnet, should be used in immunocompetent patients with CMV infection of the GI tract remains unclear [1] . In the present report, one case improved by conservative medical treatment without any antiviral medication while the other case improved after antiviral treatment. In a meta-analysis by Galiastsatos et al [6] , spontaneous resolution of CMV colitis occurred in 31.8% and most of them were younger than 55 years of age. By contrast, individuals with advanced age (older than 55 years), male sex, coexisting immune-modulating disease, and colectomy were associated with a higher mortality rate. In another recent review of 33 immunocompetent patients with CMV enterocolitis, 24.2% of the patients had spontaneous remission. No significant differences in age or specific symptoms could be identified between the treated and untreated groups [3] . More prospective interventional studies to identify the indications of initiating the antiviral treatment are warranted.
In conclusion, we reported two cases of CMV enteritis in immunocompetent patients, both diagnosed with SBE and histopathology. CMV enteritis should be included in the list of differential diagnoses when observing enteritis and ulcers during endoscopic work-up, even if the patient had no apparent immunity disorders. In addition, with increasing prevalence and technical maturation, SBE may help to identify and confirm CMV infection of the small intestines in immunocompetent hosts to prevent serious complications.
Conflicts of interest
All authors declare no conflicts of interest.
References
- [1] D.M. You, M.D. Johnson; Cytomegalovirus infection and the gastrointestinal tract; Curr Gastroenterol Rep, 14 (2012), pp. 334–342
- [2] K.H. Ryu, S.Y. Yi; Cytomegalovirus ileitis in an immunocompetent elderly adult; World J Gastroenterol, 12 (2006), pp. 5084–5086
- [3] D. Lancini, H.M. Faddy, R. Flower, C. Hogan; Cytomegalovirus disease in immunocompetent adults; Med J Aust, 201 (2014), pp. 578–580
- [4] D. Karigane, S. Takaya, Y. Seki, Y. Mastumoto, A. Onose, A. Kosakai, et al.; Cytomegalovirus enteritis in immunocompetent subjects: A case report and review of the literature; J Infect Chemother, 20 (2014), pp. 325–329
- [5] P.I. Rafailidis, E.G. Mourtzoukou, I.C. Varbobitis, M.E. Falagas; Severe cytomegalovirus infection in apparently immunocompetent patients: a systematic review; Virol J, 5 (2008), p. 47
- [6] P. Galiatsatos, I. Shrier, E. Lamoureux, A. Szilagyi; Meta-analysis of outcome of cytomegalovirus colitis in immunocompetent hosts; Dig Dis Sci, 50 (2005), pp. 609–616
- [7] J.M. Cha, J. Lee, J.W. Choe, K.R. Joo, S.W. Jung, H.P. Shin, et al.; Cytomegalovirus enteritis causing ileal perforation in an elderly immunocompetent individual; Yonsei Med J, 51 (2010), pp. 279–283
- [8] E.J. Lee, H.S. Yoon, C.I. Lee, Y.S. Lee, S.N. Hong, S.Y. Lee, et al.; Cytomegalovirus jejunitis diagnosed with single-balloon enteroscopy; Korean J Gastroenterol, 62 (2013), pp. 238–242 [in Korean]
- [9] O. Marques Jr., M. Averbach, E.C. Zanoni, P.A. Corrêa, J.L. Paccos, R. Cutait; Cytomegaloviral colitis in HIV positive patients: endoscopic findings; Arq Gastroenterol, 44 (2007), pp. 315–319
- [10] W.R. Lin, M.Y. Su, C.M. Hsu, Y.P. Ho, K.W. Ngan, C.T. Chiu, et al.; Clinical and endoscopic features for alimentary tract cytomegalovirus disease: report of 20 cases with gastrointestinal cytomegalovirus disease; Chang Gung Med J, 28 (2005), pp. 476–484
- [11] S.H. Kim, Y.S. Kim, H.W. Kim, H.E. Yoon, H.K. Kim, Y.O. Kim, et al.; A case of cytomegalovirus colitis in an immunocompetent hemodialysis patient; Hemodial Int, 15 (2011), pp. 297–300
- [12] J.H. Ko, K.R. Peck, W.J. Lee, J.Y. Lee, S.Y. Cho, Y.E. Ha, et al.; Clinical presentation and risk factors for cytomegalovirus colitis in immunocompetent adult patients; Clin Infect Dis, 60 (2015), pp. e20–e26
Document information
Published on 15/05/17
Submitted on 15/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?