Summary
Sutureless repair is an effective procedure for acute left ventricular free wall rupture; however, it may be complicated with a left ventricular pseudoaneurysm during the late postoperative period. We present a case of a large ventricular pseudoaneurysm that occurred after the sutureless repair of an inferior myocardial infarction with oozing left ventricular free wall rupture. The patient underwent aneurysmectomy successfully. Serial magnetic resonance imaging (MRI) indicated that the necrotic left ventricular wall, which was covered by Teflon felt, had ruptured and developed a pseudoaneurysm. Therefore, after simple gluing for a left ventricular free wall rupture, patients should undergo careful follow-up evaluation for potential pseudoaneurysm. Moreover, early detection by MRI and prompt surgical repair of the complication are important in patients with left ventricular free wall rupture.
Keywords
left ventricular free wall rupture;magnetic resonance imaging (MRI);pseudoaneurysm
1. Introduction
Left ventricular free wall rupture (LVFWR) is a serious complication of acute myocardial infarction.1 Conventional treatment approaches to LVFWR include ventricular repair with Teflon-buttressed sutures, using the cardiopulmonary bypass (CPB) technique. Coronary artery bypass grafting may be performed concomitantly. The optimal treatment for this lethal condition remains controversial; however, some authors have suggested that sutureless techniques with or without cardiopulmonary bypass may be effective, especially in cases involving oozing ruptures.2 We report a case of sutureless repair with Teflon felt (C R Bard Inc, Billerica, MA, USA) attached using BioGlue (Cryolife Inc., Kennesaw, GA, USA) for acute LVFWR; however, an enlarged left ventricular pseudoaneurysm (LVPA) emerged at the previous rupture site 2 months after the successful sutureless repair. Follow-up serial magnetic resonance imaging (MRI) clearly indicated the ventricular pseudoaneurysm. The patient uneventfully underwent ventricular repair with Teflon-buttressed sutures. In this report, serial MRI provided important information on the pathogenesis of LVPA after a sutureless repair of a LVFWR.
2. Case report
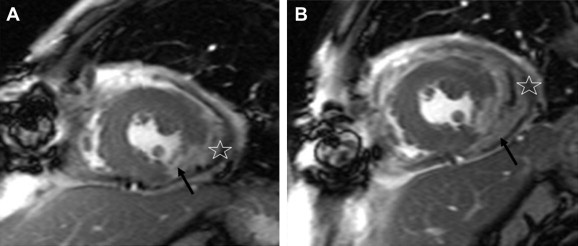
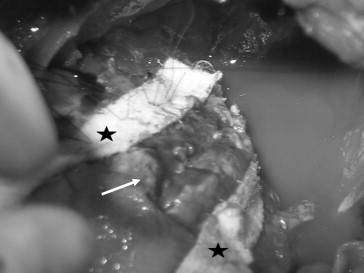
A 49-year-old man presented to our emergency department with chest pain and diaphoresis that had been intermittently occurring for 1 day. His heart rate and blood pressure were 120 beats/minute and only 79/41 mmHg, respectively. An electrocardiogram revealed an ST-segment elevation in the inferior and lateral leads. Elevation in serum creatine kinase and troponin I levels was observed. An emergent coronary angiogram showed total occlusion of the posterolateral branch of the right coronary artery. At that time, no coronary intervention was performed. Owing to the discrepancy between the deteriorating hemodynamics and the coronary lesions, emergent echocardiography was performed, which indicated massive pericardial effusion with cardiac tamponade. Pericardiocentesis was performed, and an outflow of fresh blood was noted. Thus, LVFWR was suspected, and an emergent operation was performed. After sternotomy, severe bloody oozing was observed from the lateral wall of the left ventricle. No major myocardial tear was found. An oozing postinfarct LVFWR was diagnosed. Under intra-aortic balloon pump support, the rupture site was repaired with BioGlue (Cryolife Inc.) applied to a 5 cm × 10 cm diameter Teflon felt, using a sutureless technique. The patient was discharged in a good condition 2 weeks after the operation. One month later, cardiac MRI revealed an infarcted area at the posteroinferior wall of the left ventricle and an asymptomatic localized pericardial effusion between the left ventricle and the Teflon felt (Fig. 1A). Pseudoaneurysm formation in the left ventricle was detected. The follow-up MRI performed after 2 weeks revealed an enlargement of the localized pericardial effusion (Fig. 1B). A second operation was then scheduled to assess the clinical progression of the LVPA. Under cardiopulmonary bypass, ventricular fibrillation was induced and the pseudoaneurysm was extirpated. The fibrous scar tissue around the infarcted area was partially resected. The left ventricle defect was directly closed with reinforcement using Teflon felt strips (Fig. 2). The postoperative course was uneventful, and the patient was discharged home in a stable condition.
|
|
|
Figure 1. (A) The short-axis, delayed, gadolinium (Gd)-enhanced true fast imaging with steady-state precession (FISP) image revealing a transmural hyperenhancement at the posteroinferior wall of the left ventricle (black arrow), indicating a transmural infarction. Localized leakage of the Gd contrast medium into the pericardial space is observed, suggesting pseudoaneurysm formation (asterisk). (B) The delayed, Gd-enhanced true FISP cine image obtained 2 weeks after, showing the progression of the increasing leakage of the Gd contrast medium into the pericardial space (black arrow) and the complete detachment of the Teflon felt from the epicardium (asterisk). |
|
|
|
Figure 2. The left ventricle after resection of the pseudoaneurysm (white arrow), repaired using Teflon felt strips (asterisks). |
3. Discussion
Myocardial rupture, the most devastating complication of acute coronary syndromes, is rare (3.2–6.2%) owing to the development of early reperfusion therapy in recent years.1 It accounts for 20% of early-death cases and is the second most common cause of death after acute myocardial infarction. The conventional approach, including infarctectomy followed by direct closure under cardiopulmonary bypass and a direct mattress suture buttressed with Teflon felt,3 is occasionally indicated for LVFWR, especially in blowout cases; however, conventional techniques are technically challenging and associated with an in-hospital mortality of approximately 20%.4 Furthermore, the use of cardiopulmonary bypass seems disadvantageous because systemic heparinization can aggravate an oozing type of bleeding from the infarct area. The sutureless technique was first described by Padro et al.2 The procedure is performed using a large Teflon patch and cyanoacrylate glue to cover the rupture site. It requires less time, avoids heparinization for cardiopulmonary bypass, and preserves ventricular geometry.5 It was reported to have a high success rate and associated with a few postoperative complications.6 However, LVPA requiring intervention has been reported, but mostly in case reports.5 ; 7 LVPA requires early diagnosis and subsequent surgical correction because it tends to rupture even in the chronic phase and regardless of size.8 However, patients may be asymptomatic, with the LVPA found incidentally during an imaging study.9 Therefore, a high clinical index of suspicion is required to ensure that the condition is diagnosed. To the best of our knowledge, this is the first report of a sequential MRI documenting the occurrence of a LVPA after the sutureless repair of a LVFWR.
The main reason of using cardiac MRI may be to distinguish LV pseudoaneurysm from LV true aneurysm. The true aneurysms are not likely to rupture in early postinfarct period and often treated conservatively. The LV false LV aneurysms, by contrast, are prone to rupture at any time. Surgical treatment is suggested. There is increasing evidence that cardiac MRI is more superior to ultrasonography and multislice computed tomography scan in detecting LV pseudoaneurysm, especially with delayed contrast enhancement, or FISP. Echocardiography often has a field-of-view limitation, especially in the left ventricular apex, where the majority of aneurysms occurs.
In conclusion, we present a case of LVFWR repaired using a sutureless technique. The initial result was good, but an oozing pseudoaneurysm emerged at a previous rupture site 2 months later. Under cardiopulmonary bypass, the pseudoaneurysm was successfully resected and repaired with sutures using Teflon felt strips. The sutureless technique for acute LVFWR is lifesaving and useful but requires careful patient follow-up. In this report, serial MRI was demonstrated to be the best follow-up evaluation tool for a potential pseudoaneurysm in the patient who underwent simple gluing for an oozing LVFWR.
References
- 1 J. Figueras, O. Alcalde, J.A. Barrabes, et al.; Changes in hospital mortality rates in 425 patients with acute ST-elevation myocardial infarction and cardiac rupture over a 30-year period; Circulation, 118 (2008), pp. 2783–2789
- 2 J.M. Padro, J.M. Mesa, J. Silvestre, et al.; Subacute cardiac rupture: repair with a sutureless technique; Ann Thorac Surg, 55 (1993), pp. 20–24
- 3 E. Anagnostopoulos, S. Beutler, J.M. Levett, J.M. Lawrence, C.Y. Lin, R.L. Replogle; Myocardial rupture: major left ventricular rupture treated by infarctectomy; JAMA, 238 (1997), pp. 2715–2716
- 4 F.A. Atik, J.L. Navia, P.R. Vega, et al.; Surgical treatment of postinfarction left ventricular pseudoaneurysm; Ann Thorac Surg, 83 (2007), pp. 526–531
- 5 S. Yamaguchi, G. Watanabe, S. Yamamoto; Rapid formation of the left ventricular pseudoaneurysm after sutureless repair of a subacute left ventricular free wall rupture; Interact Cardiovasc Thorac Surg, 5 (2006), pp. 462–463
- 6 M. Carnero-Alcázar, A. Alswies, L. Pérez-Isla, et al.; Short-term and mid-term follow-up of sutureless surgery for postinfarction subacute free wall rupture; Interact Cardiovasc Thorac Surg, 8 (2009), pp. 619–623
- 7 S. Fukushima, J. Kobayashi, O. Tagusari, Y. Sasako; A huge pseudoaneurysm of the left ventricle after simple gluing of an oozing-type postinfarction rupture; Interact Cardiovasc Thorac Surg, 2 (2003), pp. 94–96
- 8 K. Iha, R. Ikemura, N. Higa, et al.; Left ventricular pseudoaneurysm after sutureless repair of subacute left ventricular free wall rupture: a case report; Ann Thorac Cardiovasc Surg, 7 (2001), pp. 311–314
- 9 S. Haddadin, A.D. Milano, G. Faggian, et al.; Surgical treatment of postinfarction left ventricular free wall rupture; J Card Surg, 24 (2009), pp. 624–631
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?