Summary
Head and neck arteriovenous malformations (AVMs), including lingual AVMs, are unusual and rare. There are many treatment options including sclerotherapy, endovascular or percutaneous embolization, and surgical excision. A combination of preoperative embolization and surgical resection is commonly used for head and neck AVMs. However, in most cases, surgical resection causes significant morbidity. Single-modality approaches such as transarterial embolization are sometimes performed. Herein, we used the copolymer Onyx (ethylene–vinyl alcohol copolymer) as an embolizing agent and obtained satisfactory therapeutic outcomes. To our knowledge, this is the first report of lingual AVMs treated using Onyx embolization.
Keywords
AVMs;onyx;tongue
1. Introduction
Despite the low prevalence of head and neck arteriovenous malformations (AVMs), resection of particularly large lingual AVMs may impair lingual functions. We report the case of a patient with a large lingual AVM. The patient was treated by a novel, previously unreported embolization approach, using the copolymer Onyx. Onyx is a liquid embolizing agent, use of which has become increasingly common in past two decades. Compared with other liquid embolizing agents, including absolute ethanol and n-BCA, Onyx allows better implementation of focal embolization and less ensuing inflammatory response. 1 Using Onyx, complete occlusion was successfully achieved, and no severe complications ensued.
2. Case report
We report the case of a 42-year-old man who mainly complained of a hemorrhagic lingual mass. He had noticed the lingual mass 4–5 years ago. In April 2009, a fish bone had pierced and ruptured his lingual mass, leading to hemorrhage. Subsequently, his tongue was sutured at Taipei Hospital. However, his lingual mass ruptured again 3 days later when he arrived at our hospital for treatment. Oropharyngeal examination, computed tomography (CT) scanning, and angiography were performed.
3. Results
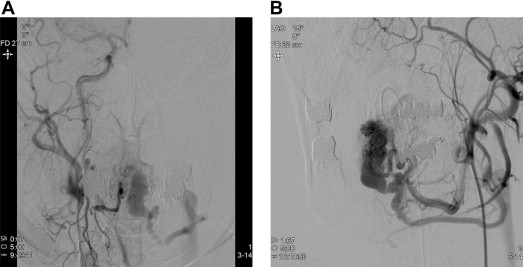
On oropharyngeal examination, a 1.5 × 1.5-cm mass on the dorsal surface of his tongue was noted. The mass extended as a bluish, tubular structure to the ventral portion of the tongue. Subsequent CT examinations revealed a large mass of 1.9 × 1.8 cm in the lingual apex extending ventrodorsally, showing a large vascular sac with prominent venous drainage (Fig. 1). Angiography via external carotid artery demonstrated a disorganized, high-flow vascular nidus with an engorged sac supplied by bilateral lingual arteries and a prominent venous drainage at lingual apex (Fig. 2). CT and angiography results established the diagnosis of lingual AVM. The man was generally healthy otherwise.
|
|
|
Figure 1. Enhanced computed tomography (CT) scanning shows an engorged, vascularized mass extending ventrodorsally. |
|
|
|
Figure 2. (A) Right external-carotid angiogram, anteroposterior (AP) view and (B) left external-carotid angiogram, oblique view showing a disorganized, high-flow vascular nidus with an engorged vascular sac and prominent venous drainage at lingual apex supplied by bilateral lingual arteries. |
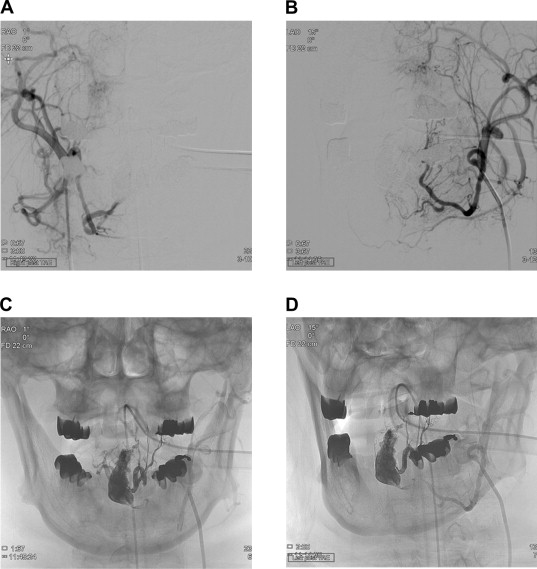
Considering difficulties of resecting such a large lesion, transarterial embolization was indicated. Therefore, after obtaining informed consent from the patient and his family, an ultraselective microcatheterization approach was used to apply a copolymer of ethylene–vinyl alcohol (Onyx) through bilateral lingual arteries to devascularize the AVM (Fig. 3).
|
|
|
Figure 3. Bilateral external-carotid angiogram obtained immediately after embolization shows (A, B) devascularization of the lesion and (C, D) retention of the Onyx copolymer in the vascular nidus and engorged vascular sac. |
Under general anesthesia, percutaneous access was obtained via the right femoral artery. A 6F guiding catheter (Cordis Envoy; Johnson and Johnson Medical, Miami, FL, USA) was positioned in the proximal external carotid artery, proximal to the lingual artery orifice. Next, a flow-directed microcatheter (Marathon, ev3 Neurovascular) was navigated into the lingual arteries as close as possible to the nidus of AVM, with an aid of a 0.008-in. guidewire (Mirage, ev3 Neurovascular). Then, Onyx was slowly and progressively injected into the nidus under continuous visual control using biplane subtracted fluoroscopy. Total procedure time was about 1 hour, and 3 cm3 (1.5 cm3/vial) Onyx was used.
After Onyx embolization, no complication except lingual pain was noted. The patient’s condition improved within 3 days. A follow-up CT 1 month later showed retention of the copolymer within the vascular lesion. The prominent venous drainage had resolved.
4. Discussion
Mulliken and Glowacki initially classified vascular anomalies into vascular tumors (e.g., the paradigmatic infantile hemangiomas) and non-tumorous vascular malformations.2 These lesions are also subdivided into slow-flow (e.g., capillary, venous, and lymphatic malformations) and fast-flow vascular malformations (e.g., AVMs).3 These classifications apply also to head and neck vascular malformations, which may occur due to rare errors in vascular morphogenesis,1 affecting various sites.4 The most common head-and-neck AVMs include buccal (31%), followed by aural (16%) and nasal (11%) AVMs, whereas mandibular (5%) or maxillary (4%) AVMs are less common.1 Focal lingual AVMs are extremely rare.4
Low prevalence of lingual AVMs has prevented systematic studies to establish standard treatment protocols.5 Generally, various therapeutic strategies, including surgical resection, endovascular embolization, stereotactic radiosurgery, or percutaneous sclerotherapy,3 have been used to treat symptomatic AVMs.
Of the treatment approaches discussed above, success of endovascular AVM treatments is not well documented. Some authors have reported endovascular approaches only to supplement surgery for definitive treatment outcomes.5 Other groups have reported successful application of embolization alone, but these studies have been limited to smaller AVMs with no long-term follow-up.1 ; 6 Nevertheless, embolization of external carotid-artery AVMs has been indicated in the following cases: (1) AVMs are deemed surgically inoperable; (2) AVM clinical manifestations are minimal; (3) surgery may likely cause significant morbidity; or (4) the patient is unwilling or unfit to undergo surgery.7
Embolization-only treatments use soluble agents capable of permeating a targeted AVM. These agents include absolute ethanol, n-BCA, and Onyx. 1 ; 8 In 1990, Onyx was first reported as an embolizing agent for cerebral AVMs.8 Onyx is a liquid embolizing agent. Upon contacting blood, Onyx congeals on the surface while maintaining a liquid core, allowing the formation of a nonadhesive, lava-like, contiguous mass.1 This property allows better implementation of focal embolization, ensuring successful and facile treatment. Onyx elicits less inflammatory response and causes less endothelial damage or necrosis than other agents such as n-BCA or absolute ethanol. 1 Because of the large size of AVM in this case, we choose Onyx for embolization, which provides better penetration into the lesion, that a high successful rate of total occlusion would be achieved.
Despite these advantages, Onyx is black and may cause unsightly discolorations of superficial lesions such as dermal lesions.1 Catheter entrapment is another potential complication, which has been reported in intracranial or extracranial AVM treatments. Currently, Onyx has been mainly applied to the cerebral or, to some extent, the peripheral AVMs, including limb and visceral AVMs.5 Surprisingly, use of Onyx for lingual AVMs has not been recorded so far. Here, we present the case of a lingual, high-flow AVM in an adult who was treated solely with endovascular Onyx embolization. In this case, our patient tolerated Onyx treatment without any significant complication.
In conclusion, the best strategy for treating head-and-neck AVMs should be based on personalized medicine. Various therapeutic approaches include sclerotherapy, endovascular or percutaneous application of embolizing agents, surgery, or a combination of these modalities. Treatment approaches should be based on the clinical and angiographic outcomes as well as economic cost. Herein, we report a case of a lingual arteriovenous malformation with the Onyx embolization. Onyx is a more controllable embolized agent compared with other options such as n-NBCA and ethanol. This advantage provides a high successful rate of total occlusion of the lesion, less procedure time, less target vessels, and potentially less tissue damage. Moreover, Onyx embolization could be an alternative choice for head and neck AVMs.
References
- 1 I.C. Wu, D.B. Orbach; Neurointerventiaonal management of high-flow vascular malformations of the head and neck; Neuroimag Clin N Am, 19 (2009), pp. 219–240
- 2 D.J. Choi, A.I. ALomari, G. Chaudry, D.B. Orbach; Neurointerventional management of low-flow vascular malformations of the head and neck; Neuroimag Clin N Am, 19 (2009), pp. 199–218
- 3 K. Honda, S. Tanaka, K. Nakazawa, T. Ohita; Surgical treatment of a rare sublingual intramuscular arteriovenous malformation; J Craniofac Surg, 18 (2007), pp. 1496–1499
- 4 G.T. Richter, J. Suen, P.E. North, C.A. James, M. Waner, L.M. Buckmiller; Arteriovenous malformations of the tongue: a spectrum of disease; Laryngoscope, 117 (2007), pp. 328–335
- 5 A. Arat, B.E. Cil, I. Vargel, et al.; Embolization of high-flow craniofacial vascular malformations with Onyx; AJNR Am J Neuroradiol, 28 (2007), pp. 1409–1414
- 6 W. Taki, Y. Yonekawa, H. Iwata, A. Uno, K. Yamashita, H. Amemiya; A new liquid material for embolization of arteriovenous malformations; AJNR Am J Neuroradiol, 11 (1990), pp. 163–168
- 7 P.D. Righi, M.A. Bade, J.J. Coleman III, M. Allen; Arteriovenous malformation of the base of tongue: case report and literature review; Microsurgery, 17 (1996), pp. 706–709
- 8 M.S. Persky, H.J. Yoo, A. Berenstein; Management of vascular malformations of the mandible and maxilla; Laryngoscope, 113 (2003), pp. 1885–1892
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?