Abstract
Aim
The aim of this study was to describe the accuracy and quality of nursing documentation of the prevalence, risk factors and prevention of pressure ulcers, and compare retrospective audits of nursing documentation with patient examinations conducted in nursing homes.
Design
This study used a cross-sectional descriptive design.
Method
A retrospective audit of 155 patients' records and patient examinations using the European Pressure Ulcer Advisory Panel form and the Braden scale, conducted in January and February 2013.
Results
The prevalence of pressure ulcers was 38 (26%) in the audit of the patient records and 33 (22%) in patient examinations. A total of 17 (45%) of the documented pressure ulcers were not graded. When comparing the patient examinations with the patient record contents, the patient records lacked information about pressure ulcers and preventive interventions.
Introduction
Pressure ulcers (PUs) remain a serious health problem for older adult patients in nursing homes (Kwong et al. 2009, Demarré et al. 2012, Bååth et al. 2014), despite a widespread focus on the prevention of PUs (Fossum et al. 2011, Beeckman et al. 2013, Bååth et al. 2014). Improving risk assessment, planning and documentation is important to help prevent PUs in nursing homes (Moore & Cowman 2012). However, risk assessment tools are not routinely used, and nurses often rely on their own knowledge to conduct skin assessments and judge patients at risk (Hulsenboom et al. 2007, Samuriwo & Dowding 2014). In nursing homes, nurses spend a lot of time on documentation and communication (Munyisia et al. 2011b, Dellefield et al. 2012); however, incomplete documentation remains an issue (Wang et al. 2015), suggesting the need for an increased focus on the accuracy of documentation (Wang et al. 2011).
To avoid the consequences of PUs, it is important to gain knowledge about the accuracy of nursing documentation related to PUs and how nurses in nursing homes communicate PU prevention strategies. An audit of record accuracy may provide important information about the documentation of prevalence, risk factors and prevention of PUs. In addition, patient examinations can provide information about the accuracy of the nursing documentation, and what nurses are actually doing and observing for their patients.
Background
PU prevalence, risk factors and prevention
A recent systematic review highlighted that no single factor can explain the risk for PUs (Coleman et al. 2013). However, increased age, decreased mobility and acute and chronic illnesses increase a patients risk for developing PUs (Bours et al. 2002, McInnes et al. 2011). PUs may cause pain, prolong hospital stays and increase patients' complications as well as social burden. In addition, PUs have an economic cost for patients, institutions and society in general (McInnes et al. 2011).
There is a lack of knowledge in nurses working in nursing homes about PU prevention (Demarré et al. 2012), with several studies noting a gap between research and practice in PU prevention (Pancorbo-Hidalgo et al. 2006, Chang et al. 2010, Meesterberends et al. 2011). A recent review found no evidence that implementing standardized PU risk assessment scales had an impact on clinical practice, although there was rationale for using these scales as quality indicators for the care process (Kottner & Balzer 2010).
Another review found limited evidence for PU prevention interventions in adults (Gillespie et al. 2014). However, a comparison of support surfaces found that foam alternatives reduced the incidence of PUs among at-risk patients compared with standard hospital foam mattresses. Studies have also shown sheepskin to be effective in reducing the incidence of PUs (McInnes et al. 2015). The European Pressure Ulcer Advisory Panel (EPUAP) and the Pressure Ulcer Advisory Panel (NPUAP) have developed international guidelines based on recent evidence. These guidelines provide evidence-based healthcare recommendations to prevent the development of PUs.
Nursing documentation in nursing homes
Documentation is an important information source when judging the quality of nursing care. However, studies have found major limitations in nursing documentation as a tool for planning and evaluating nursing care in nursing homes (Ehrenberg et al. 2001, Wang et al. 2015). An increased focus on the accuracy of nursing documentation was recommended in an extensive review conducted by Wang et al. (2011).
Two studies in hospital settings that conducted patient examinations using the Braden scale (Bergstrom et al. 1987) and the EPUAP form (European Pressure Ulcer Advisory Panel 2009) found differences in the proportion of PUs recorded in an examination compared with the nursing records (Gunningberg 2004, Thoroddsen et al. 2013), with the proportion differing by up to 40% (Gunningberg & Ehrenberg 2004, Thoroddsen et al. 2013). A Swedish study examined 413 electronic health records (EHRs) and assessed the same patients at a university hospital. Only 14·3% of PUs were documented in the EHRs, compared with 33·3% revealed during skin examinations (Gunningberg & Ehrenberg 2004). Despite the increased focus on the importance of accurate nursing documentation in improving patient outcomes, no comparison between documentation and assessment of nursing home residents has been conducted to date. This study aimed to describe the accuracy and quality of nursing documentation of PU prevalence, risk factors and prevention and compare retrospective audits of nursing documentation with patient examinations conducted in nursing homes.
The study
Design
This study used a cross-sectional, descriptive design and was conducted in five nursing homes from three municipalities in southern Norway throughout January - February 2013.
Method
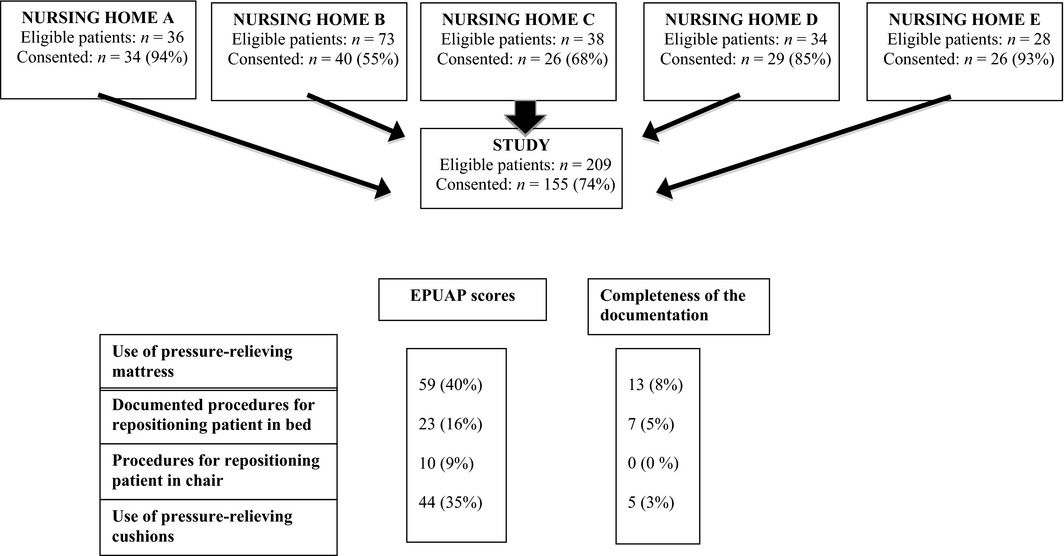
Nursing homes were recruited through an email sent to nursing home managers in the municipalities connected to the Centre for Caring Research, southern Norway. Managers who wished to participate were invited to contact the project manager, one of the present authors (RLH), by phone or email. The inclusion criterion was all patients currently living in the nursing homes. Ethical considerations lead to the exclusion of terminal patients and those considered by nursing staff to be too unwell. In total, 209 patients were invited to participate, and 155 (74%) patients or their proxies gave informed consent. Four of the five nursing homes had permanent-stay patients, including 2-4 patients in residential respite care or short-term stay (Figure 1). One ward refused to participate.
|
|
|
Figure 1. Number of nursing homes and patients included in this study and comparison of the European Pressure Ulcer Advisory Panel (EPUAP) scores with four pressure ulcer prevention interventions documented in patient records. |
Measurements
Three measurement instruments were used: the Braden scale (Bergstrom et al. 1987, Braden & Bergstrom 1994), translated into Norwegian (National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance 2014); the EPUAP form for registering PUs, based on guidelines developed by the EPUAP and the NPUAP (Beeckman et al. 2007); and an audit instrument developed by Gunningberg and Ehrenberg (2004) and translated into Norwegian by Fossum et al.(2011).
The Braden scale covers six different variables: (1) Sensory perception; (2) Degree to which skin is exposed to moisture; (3) Physical activity; (4) Mobility; (5) Food intake, nutrition and (6) Friction and shear. Variables one to five are scored on a scale from 1-4, while variable six is scored from 1-3. The scores for all six variables are added to form a summative total score. The Braden scale has been shown to be both valid and reliable (Bergstrom et al. 1987, Braden & Bergstrom 1994).
The EPUAP form records age, sex, whether the patient lives in his/her own home or a nursing home, whether the patient is in the nursing home short-term or permanently, and the patients height and weight. This form also includes the Braden scale as a separate checklist; however, in this study only data from the separate Braden scale was used because this scale had a more detailed guiding text. The skin inspection details the observed PU categories (grades). The EPUAP form notes the locations of the highest grade PUs (sacrum, heel, hip, other) and all existing PUs, documenting them on an indicator poster. The form also documents whether and what type of preventive measures are used. The EPUAP form showed excellent agreement in tests of inter-rater reliability (Bours et al. 1999, Demarré et al. 2012).
The audit instrument (Gunningberg & Ehrenberg 2004) contains 43 variables, including the patients age, sex, total length of stay in the nursing home (months) and diagnoses (other variables are presented in Tables 3 and 4). Some of these variables require a yes or no answer; if “yes”, follow-up questions must be answered, such as “Can you see any gradation in the patients records? If yes, list the order of degree.”
Data collection
Each nursing home had one or two nurses responsible for data collection. These nurses underwent a 2-hour education session conducted by one of the present authors (RLH) concerning the forms and grading of PUs. One of the present authors (RLH) had overall responsibility for data collection, which was conducted over 1 week in each nursing home.
After the patients or their proxies had given written consent to participate, patient records were printed and de-identified, and the patients were assessed with the Braden scale and the EPUAP form. The patient journal information included nursing care plans, medication charts, progress notes and summaries from the last 3 months. In general, the same nurses completed the assessment instrument for all patients in one ward.
Four nursing homes had the same EHR systems and three of these reported all nursing documentation in progress notes. In one nursing home, only nurses completed documentation using the code ‘nursing documentation’, while nurses, technicians and assistants completed documentation under an ‘assistants’ code. One nursing home used a different EHR system and used progress notes instead of nursing care plans. The patient records varied from four pages to more than 90 pages. Nineteen of the 155 patient records were audited by two of the authors (RLH;MF), and consensus was achieved by discussion. The remaining records were audited by one of the authors (RLH). Data from the audit were recorded on the audit instrument and then entered into the SPSS programme, version 19 (IBM SPSS Statistics for Windows, Version 19·0.; IBM Corp., Armonk, NY, USA).
Data analysis
All analyses were conducted using SPSS, version 19 (IBM SPSS Statistics for Windows, Version 19·0.; IBM Corp.). Most outcome variables were recorded as categorical or ordered categorical data. Thus, frequencies, proportions median (md) and quartiles (Q1;Q3) were used for statistical description (Altman 1991). Based on this study, the prevalence (p %) of PUs in nursing home patients was estimated by the 95% confidence interval (95% CI) of the proportion patients with PU according to the patient examinations, and compared with corresponding estimation of the prevalence based on the content of the nursing documentation. The discrepancy in the proportion findings of within-patient differences between the examination and the nursing documentation was evaluated by sets of paired data, and expressed as the paired proportion patients (p%; 95% CI) with missing nursing documentation in relation to the patient examination or vice versa (Altman et al. 2000).
The PU level in the patient records was rated as: no ulcer, stage I, stage II, stage III or stage IV ulcers (recoded as 0, 1, 2, 3 and 4). If a patient had several PUs, they were all noted in both the patient examinations and patient records.
In total, 19 (12%) of the patient records were assessed by two raters. Their scores were compared, and the inter-rater agreement adjusted for chance was calculated with Cohens kappa. Kappa values between 0·81-1·00 are regarded as indicating a very good agreement, kappa 0·61-0·80 as good, 0·41-0·60 as moderate, 0·21-0·40 as fair and lower values indicate poor agreement (Altman 1991).
Ethics
This study was approved by the Regional Committee for Medical Research Ethics in southern Norway (REK sør, reference number 2012-1642-REK), and by the Norwegian Social Science Data Services (project number 32123). Patients were informed in writing and verbally about the study. Between 70-80% of patients in nursing homes suffer from dementia, although many are not diagnosed (The National Directorate for Health and Sosial Affairs 2009). Accordingly, it is difficult to ensure patient autonomy despite written consent requirements. The high number of patients suffering from dementia was a key reason why nurses on the wards completed the patient examinations. The patients' PU risks were documented in their patient records for follow-up. When patients were not able to give consent to participate, consent was obtained from the person listed as the patients proxy. The research team was not informed about the number of proxies or spouses who consented on a patients behalf.
Results
At baseline, 155 patients participated. Of these, 109 (77%) were aged over 80 years, and 108 (72%) were women. A total of 112 (75%) patients were permanent nursing home residents (Table 1). The agreements between the two raters for all the variables in the audit instrument were between k = 0·58 and 1·00, indicating moderate to very good agreement, with the percentage of agreements between 54% and 100%.
| Characteristics | Frequency n (%) |
|---|---|
| Age (n = 141) | |
| 40-59 years | 1 (0) |
| 60-69 years | 5 (4) |
| 70-79 years | 26 (18) |
| 80-89 years | 69 (49) |
| >89 years | 40 (28) |
| Sex (n = 151) | |
| Female | 108 (72) |
| Male | 43 (29) |
| Type of ward (n = 150) | |
| Residential respite care | 38 (25) |
| Permanent stay | 112 (75) |
Paired comparisons of the record contents and patient examinations
The comparisons between the 155 patient examinations and the content of the nursing documentation showed that the prevalence of PUs was 33 (21%, 95% CI, 21-29%) according to the patient examinations. Correspondingly, the prevalence of PUs according to the content of the nursing documentations was slightly different, 38 (25%; 95% CI, 19-32%), as indicated by the two overlapping confidence intervals. However, according to the paired comparisons of patient examinations and the nursing documentations, only 18 (54·5%) patients with assessed PU in the examinations were also found in the content of the nursing documentations. The remaining 20 patients with documented PU were assessed with ‘no PU’ in the examinations, and another 15 patients (45·5%. 95% CI, 30-62%) with assessed PU in the examinations were not documented as having PU in their patient records. This indicates that based on this study one can expect lack of reporting in 30-62% of patients with PUs. Furthermore, 17 (45%) of the documented 38 PUs were not graded.
When comparing complete pairs of data from patient examinations and the corresponding contents of the patient records, 59 (40%) of 146 patients received pressure-relieving mattress prevention and 10 of these patients had pressure-relieving mattress documented in their patient records. This result shows that 49 (83%, 95% CI, 72-91%) of the pressure-relieving mattresses were not documented. Correspondingly, regarding the prevention of PUs in chairs, 44 (35%, 95% CI 27-44%) of the 126 patients of complete pairs of data had pressure-relief cushions in the chair, but 42 (96%, 95% CI, 86-99%) of these patients did not have pressure-relief cushions in the chair documented in their patient records.
Procedures of repositioning in bed were assessed and identified in 23 (16%) of 140 patient examinations. Eighteen of these identified patients (78%, 95% CI, 58-90%) did not have procedures of repositioning in bed documented. Correspondingly, procedures of repositioning in chair were assessed and identified in 10 (16%) of 118 patient examinations. About ten (100%, 95% CI, 72-100%) patients did not have the repositioning in chair documented.
Patient EPUAP and Braden Scale Evaluations
Braden scores from patient examinations were reported for 149-153 patients; although 155 patients consented to participate, six patients had incomplete data. Table 2 shows that the median and quartile scores for the six Braden scale items differed slightly.
| Characteristics | |
|---|---|
| Braden score: number of residents (an = 153) | |
| Sensory perception (n = 149): mdb (Q1;Q3)c | 3 (3;4) |
| Degree to which skin is exposed to moisture (n = 152): md (Q1;Q3) | 4 (3;4) |
| Physical activity (n = 150): md (Q1;Q3) | 3 (2;4) |
| Mobility (n = 153): md (Q1;Q3) | 3 (2;4) |
| Food intake, nutrition (n = 153): md (Q1;Q3) | 3 (3;4) |
| Friction and shear (n = 149): md (Q1;Q3) | 2 (2;3) |
| Braden score total (n = 149): md (Q1;Q3) | 18 (16;18) |
| Prevalence of pressure ulcers (an = 154) | |
| No pressure ulcer: n (%) | 121 (79) |
| Stage 1: n (%) | 20 (13) |
| Stage 2: n (%) | 6 (4) |
| Stage 3: n (%) | 4 (3) |
| Stage 4: n (%) | 3 (2) |
| Prevention of pressure ulcers in bed (n = 146) | |
| No pressure-relieving mattress: n (%) | 87 (60) |
| Pressure-relieving mattress with or without motor: n (%) | 59 (40) |
| Pressure-relieving pillow for heels in bed (n = 92) | |
| Yes: n (%) | 32 (35) |
| No: n (%) | 60 (65) |
| Prevention of pressure ulcers in a chair (n = 126) | |
| No pressure-relieving cushion: n (%) | 82 (65) |
| Pressure-relieving pillow without motor: n (%) | 44 (35) |
| Repositioning of the patient in bed (n = 140) | |
| Yes: n (%) | 23 (16) |
| No: n (%) | 117 (84) |
| Repositioning of the patient in chair (n = 118) | |
| Yes: n (%) | 10 (9) |
| No: n (%) | 108 (91) |
|
a Missing data. a Missing data. b Median (md). a Missing data. b Median (md). c Inter-quartiles range (Q1;Q3). | |
The number of PUs was 33 (22%), categorized into four stages: stage 1 = 20 (13%), stage 2 = 6 (4%), stage 3 = 4 (3%) and stage 4 = 3 (2%). In total, 59 patients (40%) had a pressure-relieving mattress with or without a motor, and 32 patients (35%) had pressure-relieving pillows on their beds. Forty-four patients (35%) had pressure-relieving cushions in their chairs; 23 (16%) had procedures for repositioning in bed and 10 (9%) chair-bound patients had repositioning procedures.
Prevalence, Risk Factors and Prevention of PUs in Nursing Documentation
Table 3 shows the PUs documented in the patient records. Thirty-eight patients (26%) had PUs recorded in the nursing documentation, categorized as: stage 1 = 9 (6%), stage 2 = 10 (7%), stage 3 = 1(1%) and stage 4 = 1(1%). The remaining 17 (11%) patients had an undocumented PU level. Pressure-relieving mattresses with or without a motor were noted in nursing documentation for 13 patients (8%). Seven patients (5%) had pressure-relieving cushions in their chairs; seven (5%) patient records documented procedures for repositioning patients in bed and zero (0%) documented repositioning procedures for a chair-bound patient.
| Variables | n (%) |
|---|---|
| Prevalence of pressure ulcers in patient records | |
| No pressure ulcer | 117 (76) |
| Stage 1 | 9 (6) |
| Stage 2 | 10 (7) |
| Stage 3 | 1 (1) |
| Stage 4 | 1 (1) |
| Undocumented degree of pressure ulcer | 17 (11) |
| Prevention of pressure ulcers in bed | |
| No pressure-relieving mattress | 142 (92) |
| Pressure-relieving mattress with or without motor | 13 (8) |
| Prevention of pressure ulcers in a chair | |
| No pressure-relieving cushion | 150 (97) |
| Pressure-relieving pillow with or without motor | 5 (3) |
| Procedures for repositioning the patient in bed | |
| Yes | 7 (5) |
| No | 148 (96) |
| Procedures for repositioning the patient in chair | |
| Yes | 0 (0) |
| No | 155 (100) |
Table 4 presents the completeness of the nursing documentation in terms of PU risk and prevalence. In 116 patient records (75%), patient discomfort or the need to change positions was described. The degree of sensory perception was described in terms of three of the following four variables: complete deterioration, n = 0 (0%); significantly impaired, n = 5 (4%); somewhat weaker, n = 15 (9%) and no impairment n = 39 (34%).
| Documentation in the patient records (n = 155) | n (%) |
|---|---|
| Sensory perception | |
|
(Description of discomfort or the need to change position) If yes
|
116 (75) |
| Specified degree of sensory perception | |
| Complete deterioration | 0 (0) |
| Significantly impaired | 5 (4) |
| Somewhat weaker | 15 (9) |
| No impairment | 39 (34) |
| Degree to which skin is exposed to moisture | |
| If yes | 109 (70) |
| Degree of moisture | |
| Constantly moist | 0 (0) |
| Often moist | 10 (9) |
| Somewhat damp | 26 (24) |
| Dry or normal moisture | 27 (25) |
| Physical activity | |
| If yes | 148 (96) |
| Level of physical activity | |
| Bedridden | 2 (1) |
| In a wheelchair | 31 (21) |
| Walks with assistance | 42 (28) |
| Walks with and without aids | 56 (38) |
| Mobility | |
| If yes | 148 (96) |
| Specified degree of mobility | |
| Bedridden | 2 (1) |
| Very limited | 28 (19) |
| Slightly limited | 61 (41) |
| Unlimited | 18 (12) |
| Food intake, nutrition | |
| If yes | 119 (77) |
| Specified level of food intake | |
| Less than half the normal portion | 2 (2) |
| Half of the normal portion | 1 (1) |
| Three-fourths of the normal portion | 2 (2) |
| Normal portion | 8 (7) |
| Friction and shear | |
| If yes | 9 (6) |
| Grade not specified | 9 (100) |
Discussion
Our study highlights a gap between the use of preventive strategies documented in patient records and data from patient examinations in nursing homes. Lack of accuracy may challenge the use of patient records as a valid source of information in nursing practice. Our results are similar to findings from a study conducted by Gunningberg and Ehrenberg (2004) in a hospital setting, and other studies conducted in aged care facilities (Schnelle et al. 2004, Fossum et al. 2013, Alexander 2015). The results of this study were derived from an audit of patient records. As nurses in nursing homes frequently use other sources of information, such as oral handover between shifts, a strong tradition of oral communication in nursing may have influenced our results. However, the PU prevalence rate was consistent with those reported in other international studies, but slightly lower for severe PU stages (Vanderwee et al. 2007, Moore & Cowman 2012, Bååth et al. 2014). Although several prevention strategies are commonly implemented in healthcare services, the PU prevalence appears to be at the same level (Bååth et al. 2014).
Our results of paired comparisons showed differences between the prevention strategies documented in the patient records and assessed prevention strategies, such as the use of pressure-relieving mattress, repositioning the patient in bed or in a chair and the use of pressure-relieving cushions. Based on the results of this study, it is likely that a lack of recording of procedures of repositioning the patient in bed may be identified in 58-90% of patient records, and a lack of documented pressure-relieving mattresses may be identified in 72-91% of patient records. Patients at high risk for developing PUs should use pressure-relieving mattresses instead of standard hospital foam mattresses (McInnes et al. 2011), and alternating pressure mattresses may be more cost-effective than alternating pressure overlay mattresses (McInnes et al. 2011). An earlier study conducted in a hospital setting showed similar results to our study, with nurses performing more interventions than they recorded in patient records (Gunningberg & Ehrenberg 2004). However, this earlier study also showed similar differences in the number and grades of PUs between the record audits and the patient examinations. These results differed from our results, where nurses documented more pressure injuries but the documentation lacked accuracy and was incomplete. A reason for the discrepancy between the records and examinations may be that nurses in nursing homes do not have time, skills and knowledge to update patient records. A study conducted in nursing homes has shown that nurses and nursing assistants in nursing homes have a lack of knowledge about PU prevention (Demarré et al. 2012), and continuing PU prevention education and use of PU ‘champions’ may improve the accuracy and quality of nursing documentation (Sullivan & Schoelles 2013).
Patients in nursing homes are commonly aged over 80 years and have a variety of additional diseases, making prevention measures important (The National Directorate for Health and Sosial Affairs 2009). The results of our study showed that nurses undertake more PU prevention than they document in patient records. Underreporting of PU prevention efforts may be of concern for nursing home managers in terms of competence (McInnes et al. 2011) and economics (Bennett et al. 2004, Whittington et al. 2004, McInnes et al. 2011). A previous study concluded that documentation did not reflect the use of systematic assessment and research-based instruments to determine whether patients had PUs or were at risk for developing PUs (Gunningberg et al. 2001); findings consistent with the results of our study.
Despite an increased focus on PU prevention, the lack of accuracy in nursing documentation should be addressed. Implementing EHRs with decision support tools may be one way to address this issue and improve the quality and accuracy of documentation in nursing homes (Munyisia et al. 2011a, 2012, Wang et al. 2013).
Methodological limitations
Owing to ethical issues, several nurses completed the data collection rather than one person, which may have had an impact on the reliability of data collected. However, one of the present researchers was in attendance at the nursing homes during data collection to avoid errors in collected data. As PUs are associated with poor care, underreporting of PUs might have occurred; however, the prevalence of PUs was similar to other studies from nursing homes (Vanderwee et al. 2007, Fossum et al. 2011), and the nurses that completed the data collection received instruction and education to develop their data collection techniques.
The validity of the results of this study may be limited because of the exclusion criteria (terminal patients and those unwell to participate). Patients unable to consent and with spouses/proxies that were difficult to contact were not included. As other relevant characteristics such as diagnosis were not collected, non-participating patients may have had worse health conditions than the participants. Overall, the agreement between the two raters was moderate to very good, and our results were consistent with other studies.
Conclusions
There is a gap between nursing practice and nursing documentation in nursing homes. Nurses may need training and education to perform high quality PU prevention and complete accurate nursing documentation for patients in nursing homes. We found inaccuracies in the nursing documentation in nursing homes, indicating that it is necessary to focus on organizing clinical practice to ensure nurses have the opportunity to use available guidelines and document their nursing practice. Further research should explore different EHRs systems and identify standardization that may support nurses to perform more complete and accurate documentation of their practice in nursing homes.
Acknowledgments
We thank the residents and the nursing staff that participated in the study.
Conflict of interest
No conflict of interest.
Author contributions
Study design: RL.H, M.F; data collection: RL.H, M.F; analysis and interpretation of the results: RL.H, M.F; manuscript preparation: RL.H, M.F.
All authors have agreed on the final version and meet at least one of the following criteria [recommended by the ICMJE (http://www.icmje.org/recommendations/)]:
- substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data;
- drafting the article or revising it critically for important intellectual content.
References
- Alexander G.L. (2015) Nurse assistant communication strategies about pressure ulcers in nursing homes. Western Journal of Nursing Research37, 984–1004.
- Altman D.G. (1991) Practical Statistics for Medical Research. Chapman and Hall, London.
- Altman D., Machin D., Bryant T. & Gardner S. (2000) Statistics with confidence: confidence interval and statistical guidelines. Bristol: BMJ Books, London.
- Bååth C., Idvall E., Gunningberg L. & Hommel A. (2014) Pressure-reducing interventions among persons with pressure ulcers: results from the first three national pressure ulcer prevalence surveys in Sweden. Journal of Evaluation in Clinical Practice20, 58–65.
- Beeckman D., Schoonhoven L., Fletcher J., Furtado K., Gunningberg L., Heyman H., Lindholm C., Paquay L., Verdu J. & Defloor T. (2007) EPUAP classification system for pressure ulcers: European reliability study. Journal of Advanced Nursing60, 682–691.
- Beeckman D., Clays E., Van Hecke A., Vanderwee K., Schoonhoven L. & Verhaeghe S. (2013) A multi-faceted tailored strategy to implement an electronic clinical decision support system for pressure ulcer prevention in nursing homes: a two-armed randomized controlled trial. International Journal of Nursing Studies50, 475–486.
- Bennett G., Dealey C. & Posnett J. (2004) The cost of pressure ulcers in the UK. Age and Ageing33, 230–235.
- Bergstrom N., Braden B.J., Laguzza A. & Holman V. (1987) The Braden scale for predicting pressure sore risk. Nursing research36, 205–210.
- Bours G., Halfens R., Lubbers M. & Haalboom J. (1999) The development of a national registration form to measure the prevalence of pressure ulcers in the Netherlands. Ostomy/Wound Management45, 28–40.
- Bours G., Halfens R., Abu-Saad H. & Grol R. (2002) Prevalence, prevention and treatment of pressure ulcers: descriptive study in 89 institutions in the Netherlands. Research in Nursing and Health25, 99–110.
- Braden B. & Bergstrom N. (1994) Predictive validity of the Braden scale for pressure sore risk in a nursing home. Research in Nursing and Health17, 459–470.
- Chang H.C., Russell C. & Jones M.K. (2010) Implementing evidence-based practice in Taiwanese nursing homes: attitudes and perceived barriers and facilitators. Journal of Gerontological Nursing36, 41–48.
- Coleman S., Gorecki C., Nelson E.A., Closs S.J., Defloor T., Halfens R., Farrin A., Brown J., Schoonhoven L. & Nixon J. (2013) Patient risk factors for pressure ulcer development: systematic review. International Journal of Nursing Studies50, 974–1003.
- Dellefield M.E., Harrington C. & Kelly A. (2012) Observing how RNs use clinical time in a nursing home: a pilot study. Geriatric Nursing33, 256–263.
- Demarré L., Vanderwee K., Defloor T., Verhaeghe S., Schoonhoven L. & Beeckman D. (2012) Pressure ulcers: knowledge and attitude of nurses and nursing assistants in Belgian nursing homes. Journal of Clinical Nursing21, 1425–34.
- Ehrenberg A., Ehnfors M. & Smedby B. (2001) Auditing nursing content in patient records. Scandinavian Journal of Caring Sciences15, 133–141.
- European Pressure Ulcer Advisory Panel (2009) EPUAP-NPUAP Guidelines – 2009 Version & Translations [Online]. Retrieved from http://www.epuap.org/guidelines/guidelines-old/on 20 October 2015.
- Fossum M., Alexander G.L., Ehnfors M. & Ehrenberg A. (2011) Effects of a computerized decision support system on pressure ulcers and malnutrition in nursing homes for the elderly. International Journal of Medical Informatics80, 607–617.
- Fossum M., Ehnfors M., Svensson E., Hansen L.M. & Ehrenberg A. (2013) Effects of a computerized decision support system on care planning for pressure ulcers and malnutrition in nursing homes: an intervention study. International Journal of Medical Informatics82, 911–921.
- Gillespie B.M., Chaboyer W.P., McInnes E., Kent B., Whitty J.A. & Thalib L. (2014) Repositioning for pressure ulcer prevention in adults. Cochrane Database Systematic Review Issue 4. Art. No.: CD009958.
- Gunningberg L. (2004) Pressure ulcer prevention: evaluation of an education programme for Swedish nurses. Journal of Wound Care13, 85–89.
- Gunningberg L. & Ehrenberg A. (2004) Accuracy and quality in the nursing documentation of pressure ulcers: a comparison of record content and patient examination. Journal of Wound, Ostomy, and Continence Nursing31, 328–335.
- Gunningberg L., Lindholm C., Carlsson M. & Sjoden P. (2001) Risk, prevention and treatment of pressure ulcers - nursing staff knowledge and documentation. Scandinavian Journal of Caring Sciences15, 257–263.
- Hulsenboom M., Bours G. & Halfens R. (2007) Knowledge of pressure ulcer prevention: a cross-sectional and comparative study among nurses. BMC Nursing6, 1–11.
- Kottner J. & Balzer K. (2010) Do pressure ulcer risk assessment scales improve clinical practice?Journal of Multidiciplinary Healthcare3, 103–11.
- Kwong E.W., Pang S.M., Aboo G.H. & Law S.S. (2009) Pressure ulcer development in older residents in nursing homes: influencing factors. Journal of Advanced Nursing65, 2608–2620.
- McInnes E., Jammali-Blasi A., Bell-Syer S.E., Dumville J.C. & Cullum N. (2011) Support surfaces for pressure ulcer prevention. The Cochrane Library Issue 4. Art. No.: CD001735.
- McInnes E., Jammali-Blasi A., Bell-Syer S. E., Dumville J. C., Middleton V. & Cullum N. (2015) Support surfaces for pressure ulcer prevention. Cochrane Database of Systematic Reviews Issue 9. Art. No.: CD001735.
- Meesterberends E., Halfens R., Heinze C., Lohrmann C. & Schols J. (2011) Pressure ulcer incidence in Dutch and German nursing homes: design of a prospective multicenter cohort study. BMC Nursing [Online] 10. Retrieved from http://www.biomedcentral.com/1472-6955/10/8 on 22 January 2012.
- Moore Z. & Cowman S. (2012) Pressure ulcer prevalence and prevention practices in care of the older person in the Republic of Ireland. Journal of Clinical Nursing21, 362–371.
- Munyisia E.N., Yu P. & Hailey D. (2011a) Does the introduction of an electronic nursing documentation system in a nursing home reduce time on documentation for the nursing staff?International Journal of Medical Informatics80, 782–792.
- Munyisia E.N., Yu P. & Hailey D. (2011b) How nursing staff spend their time on activities in a nursing home: an observational study. Journal of Advanced Nursing67, 1908–1917.
- Munyisia E.N., Yu P. & Hailey D. (2012) The impact of an electronic nursing documentation system on efficiency of documentation by caregivers in a residential aged care facility. Journal of Clinical Nursing21, 2940–2948.
- National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance (2014) Prevention and Treatment of Pressure Ulcers: Quick Reference Guide. Emily Haesler (Ed.). Cambridge Media: Osborne Park, Western Australia.
- Pancorbo-Hidalgo P.L., Garcia-Fernandez F.P., Lopez-Medina I.M. & Alvarez-Nieto C. (2006) Risk assessment scales for pressure ulcer prevention: a systematic review. Journal of Advanced Nursing54, 94–110.
- Samuriwo R. & Dowding D. (2014) Nurses' pressure ulcer related judgements and decisions in clinical practice: a systematic review. International Journal of Nursing Studies51, 1667–1685.
- Schnelle J.F., Bates-Jensen B.M., Chu L. & Simmons S.F. (2004) Accuracy of nursing home medical record information about care-process delivery: implications for staff management and improvement. Journal of the American Geriatrics Society52, 1378–1383.
- Sullivan N. & Schoelles K.M. (2013) preventing in-facility pressure ulcers as a patient safety strategy a systematic review. Annals of Internal Medicine158, 410–416.
- The National Directorate for Health and Sosial Affairs (2009) Samhandlingsreformen: rett behandling – på rett sted – til rett tid [Report nr 47 ((2008–2009)) The Collaboration Reform, right treatment-at the right place -at the right time] Helse- og omsorgsdepartementet, Oslo.
- Thoroddsen A., Sigurjónsdóttir G., Ehnfors M. & Ehrenberg A. (2013) Accuracy, completeness and comprehensiveness of information on pressure ulcers recorded in the patient record. Scandinavian Journal of Caring Sciences27, 84–91.
- Vanderwee K., Clark M., Dealey C., Gunningberg L. & Defloor T. (2007) Pressure ulcer prevalence in Europe: a pilot study. Journal of Evaluation in Clinical Practice13, 227–235.
- Wang N., Hailey D. & Yu P. (2011) Quality of nursing documentation and approaches to its evaluation: a mixed-method systematic review. Journal of Advanced Nursing67, 1858–1875.
- Wang N., Yu P. & Hailey D. (2013) Description and comparison of documentation of nursing assessment between paper-based and electronic systems in Australian aged care homes. International Journal of Medical Informatics82, 789–797.
- Wang N., Yu P. & Hailey D. (2015) The quality of paper-based versus electronic nursing care plan in Australian aged care homes: a documentation audit study. International Journal of Medical Informatics84, 561–569.
- Whittington K.T., Briones R., Whittington K.T. & Briones R. (2004) National prevalence and incidence study: 6-year sequential acute care data. Advances in Skin & Wound Care17, 490–4.
Document information
Published on 09/06/17
Submitted on 09/06/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?