Abstract
Background
In the majority of patients with alcohol use disorder (AUD), the clinical course is characterized by multiple relapses to drinking, frequently preceded by intense craving for alcohol. The present pilot study aimed to assess the effects of a repetitive imaginary cue-exposure protocol in reducing craving in recently abstinent alcohol-dependent patients.
Methods
Sixty-four patients were randomly assigned to six intervention groups and were instructed to repetitively imagine: i) drinking a glass of their preferred alcoholic drink (low vs. high number of repetitions); or ii) drinking a glass of water (low vs. high number of repetitions); or iii) performing an analogous movement or performed no imagination. Additionally, 10 healthy controls were instructed to repetitively imagine drinking a glass of their preferred alcoholic drink (high number of repetitions). The levels of craving before and after intervention were measured using the Alcohol Urge Questionnaire (AUQ) and the Visual Analogue Scale for Craving (VASC).
Results
Repetitive imagination of alcohol consumption did not lead to a significant decrease in craving in alcohol-dependent patients as measured by the AUQ and VASC. In contrast, healthy controls showed a nearly significant decrease of the urge to drink alcohol after applying the protocol with a high number of repetitions.
Conclusions
The findings of this pilot study might indicate an aberrant ability to habituate to alcohol-related stimuli in patients with AUD compared to healthy subjects. Future studies in larger samples are needed to further explore the effectiveness of imaginary cue-exposure interventions in alcohol dependence.
Keywords
Alcohol dependence;Alcohol use disorder;Craving;Repetitive imagination;Cue-exposure;Habituation
1. Introduction
Alcohol dependence is a chronic disorder characterized by multiple relapses to drinking after detoxification treatment in the majority of patients (Bottlender, Spanagel, & Soyka, 2007). To improve mid- and long-term treatment outcome, several therapeutic approaches can be applied to support patients in reducing alcohol consumption or in maintaining alcohol abstinence. With regard to psychotherapy, particularly cognitive-behavioral therapy (CBT) has proven efficacy in alcohol dependence (Magill & Ray, 2009).
According to the theoretical framework of CBT, addictive disorders can be regarded as learned behavioral reactions based on conditioning processes (Kadden, 2001). CBT interventions for alcohol dependence commonly include strategies to reduce craving (Back et al., 2007 ; Naqvi et al., 2015), a strong desire to consume a drug, which has been shown to be an important predictor for relapse in some alcohol-dependent patients (Carter and Tiffany, 1999 ; Niaura et al., 1988). Craving has been described as a conditioned reaction that might be elicited by stimuli (cues) that have previously been associated with the consumption of drugs; thus, alcohol-associated stimuli can become conditioned cues that engender conditioned responses such as alcohol craving (Heinz et al., 2009 ; Ludwig and Wikler, 1974). Besides conditioning models of craving, also cognitive models have been proposed assuming that responses to alcohol-associated stimuli involve cognitive processes (e.g., expectations regarding the positive effects of alcohol) (Anton, 1999). In this context, desire thinking has been described as a voluntary cognitive process including verbal and imaginary elaboration of a desired target (e.g., alcohol consumption) (Caselli and Spada, 2011 ; Caselli et al., 2012). It is based on the so-called Elaborated Intrusion theory of desire which suggests that the occurrence of craving might result from a combination of conditioned and voluntary cognitive processes (Caselli and Spada, 2015 ; Kavanagh et al., 2005). Desire thinking has been reported to contribute to the escalation of craving (Caselli, Soliani, & Spada, 2013).
Exposure therapy is a common CBT technique regularly used in anxiety or obsessive-compulsive disorders (Abramowitz, 2013). Thereby, prolonged exposure to a specific stimulus is used to induce habituation and reduce anxiety-related reactions (Myers, 2008). Habituation is defined as the response occurring when a specific stimulus is repeatedly presented, leading to a decrease of previous reactions that were usually induced by that stimulus (Epstein et al., 2009 ; Myers, 2008). One of the substantial features of habituation is stimulus specifity, i.e., the decrease of responding is specific to the habituating stimulus whereas novel stimuli might evoke recovery of responding (Epstein et al., 2009 ; Myers, 2008). Other stimuli, so called dishabituators, might lead to a weakening of habituation as shown in behavioral experiments using taste or olfactory stimuli (Critchley and Rolls, 1996; Epstein et al., 1992 ; Wisniewski et al., 1992). Regarding food intake, a recent study reported a decrease in craving for chocolate in female participants repetitively exposed to chocolate cues (Coelho, Nederkoorn, & Jansen, 2014).
In substance use disorders, studies on the clinical efficacy of cue-exposure techniques reported mixed results; in in cigarette smokers, one study found an abstinence rate of 36% after 8 cue-exposure sessions, but an abstinence rate of only 7% one month later (Corty & McFall, 1984). A laboratory study in smokers found an increase in craving for cigarettes after in vivo exposure to smoking cues on several days (Miranda, Rohsenow, Monti, Tidey, & Ray, 2008). In alcohol dependence, one study with a follow-up of up to 12 months showed a decrease in alcohol consumption in patients receiving cue-exposure treatment (Rohsenow et al., 2001) whereas a meta-analysis found no evidence for the efficacy of this treatment approach in addictive disorders (Conklin & Tiffany, 2002). On a neurobiological level, a recent functional Magnetic Resonance Imaging (fMRI) study showed that repeated sessions of cue-exposure therapy in alcohol-dependent patients lead to reduced cue-elicited brain activation during the presentation of alcohol-related stimuli (Vollstadt-Klein et al., 2011).
In CBT, cue-exposure therapy can be applied both in vivo and in sensu (imaginary cue-exposure). Imagination techniques are a well-known therapeutic approach in anxiety disorders ( Myers, 2008). Imagination of specific, especially phobic stimuli can lead to anxiety-related reactions similar to real confrontations with the specific stimuli and therefore can be applied in exposure treatment ( Lang, 1977 ; Myers, 2008). Regarding substance-related disorders, Tiffany & Drobes found an increase of craving for nicotine in smokers who imagined cigarette smoke (Tiffany & Drobes, 1990). Similarly, one study in smokers reported a craving induction by personalized as well as standardized imaginary smoking scenarios (Conklin & Tiffany, 2001). Recently, Morewedge et al. published a study on the effects of imaginary food consumption (Morewedge, Huh, & Vosgerau, 2010). In several experiments, the study investigated the effects of repetitive imagination of consumption of chocolate balls (up to 30 times) on the consecutive real consumption of chocolate. Control conditions included repetitive imagination of consumption of chocolate balls fewer times (3 times), consuming cheese balls, and performing an analogous movement (inserting a coin into a washing machine). The authors observed a significant decrease in real consumption of chocolate balls after frequent repetitive imagination (30 times). They hypothesized that repetitive imagination of consumption might lead to habituation and consequently to a reduction of real consumption (Morewedge et al., 2010). Consistently, several studies underline the ability of mental imagery to reduce cravings for food (Kemps & Tiggemann, 2014).
The objective of the present study was to examine the effects of repetitive imagination of alcohol consumption on craving in recently detoxified, abstinent alcohol-dependent patients. Based on positive findings in healthy subjects and positive results from in vivo cue-exposure studies in alcohol-dependent patients, we hypothesized that frequent repetitive imagination of alcohol consumption might lead to a reduction in craving for alcohol in patients with AUD.
2. Methods
This study was conducted at the outpatient unit of the Department of Psychiatry and Psychotherapy at the Campus Charité Mitte of the Charité – Universitätsmedizin Berlin. Patients were recruited from the outpatient department between February 2012 and October 2014. Inclusion criteria for men and women were: (a) age of ≥ 18 and < 65 years; (b) diagnosis of alcohol dependence according to ICD-10 (WHO, 1994); (c) a completed in- or outpatient detoxification before randomization; and (d) sufficient German language skills. Exclusion criteria were significant internal, psychiatric (axis I diagnoses other than alcohol or nicotine dependence) or neurological conditions which require immediate treatment (as assessed by an experienced physician) as well as treatment mandated by a legal authority. Healthy controls were recruited at the Campus Charité Mitte. This study was conducted in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice and approved by the local ethics committee. Written informed consent was obtained from all study participants.
2.1. Study design and procedures
Patients were recruited and assigned to six treatment groups by baseline adaptive randomization. All patients attended up to six imagination sessions (three times a week) planned for the two weeks following their alcohol detoxification treatment. The investigator was blinded to the treatment condition. In case of relapse, participants left the study subsequently. Relapse rate was not an outcome measure due to the short duration of the study. During the sessions, participants were seated in front of a monitor showing one picture of an alcoholic drink or water in a glass or a cup of cleaning agent. Each picture appeared for 3 s and was presented several times (depending on the treatment group, see below). Participants were instructed to repetitively imagine: i) drinking a glass of their preferred alcoholic drink (as assessed at baseline); or ii) drinking a glass of water; and/or iii) performing an analogous movement (i.e., filling a cup of cleaning agent into a washing machine; a control condition which includes a motor action similar to drinking) for several times (depending on the treatment group). In group 1, the presentation included a picture of a cup of cleaning agent for three times followed by a picture of the preferred alcoholic drink for 30 times. The same protocol was applied in group 2 except for a picture of a glass of water which was shown instead of the preferred alcoholic drink. In group 3, a picture of a cup of cleaning agent was presented for 30 times, followed by a picture of the preferred alcoholic drink for 3 times. The same protocol was applied in group 4 except for a picture of a glass of water which was shown instead of the preferred alcoholic drink. In group 5, a picture of a cup of cleaning agent was presented for 33 times, group 6 did not receive any of these interventions, but underwent an identical clinical procedure at the outpatient unit. Group 7 consisted of healthy subjects who received the same intervention as group 1 (a picture of a cup of cleaning agent for three times followed by a picture of the preferred alcoholic drink for 30 times). Healthy subjects performed only one session. This group was included to assess differences in the effects of repetitive imagination compared to alcohol-dependent patients. The number of imagined actions was the same in each intervention group (33 repetitions) to keep effort constant across groups.
Before and after this presentation which took approximately 2–3 min, study participants completed the Alcohol Urge Questionnaire (AUQ) (Bohn, Krahn, & Staehler, 1995) and the Visual Analogue Scale for Craving (VASC) (Mottola, 1993) to assess changes in craving. The AUQ consists of 8 items (item 1: “All I want to do now is have a drink”) rated on a 7-point Likert scale from “strong disagreement” to “strong agreement” with higher total scores reflecting a higher level of craving for alcohol. The AUQ has been shown to have a strong internal consistency (α = 0.91) and has been validated for assessing craving in laboratory studies (Bohn et al., 1995). The VASC consists of a continuous horizontal line with 100 mm length and two endpoints [no desire (0) to very strong desire (100) for the question “How strong is your desire for alcohol right now?]. A high correlation (r > 0.99) between visual analogue scales and categorical 5-point scales for measuring pain has been reported (Averbuch & Katzper, 2004). Furthermore, withdrawal symptoms were assessed clinically. Overall, each session lasted for approximately 20 min.
2.2. Statistical analyses
Statistical analyses were performed using IBM® SPSS® Statistics 21, ©SPSS Inc., IBM Corp., Armonk, NY, USA, and SAS® 9.1, ©SAS Institute Inc., Cary, NC, USA. Due to the small sample sizes and/or nonsymmetrically distributed data, only nonparametric statistics were applied.
In order to investigate particular data with repeated measurements over time, we applied a nonparametric multivariate analysis of longitudinal data in a two-factorial design (1st factor: group, 2nd factor: time) [nonparametric RM MANOVA] (Brunner, Domhof, & Langer, 2002) and adjusted for baseline measurements in an analysis of covariance [nonparametric RM MANCOVA] (Bathke & Brunner, 2003). The chosen level of significance was p < 0.05.
Differences in the number of completed study sessions between groups were tested by using the Mann Whitney U test. Due to multiple comparisons in the analysis of the number of sessions, a Bonferroni correction was performed resulting in a level of significance of p < 0.01.
3. Results
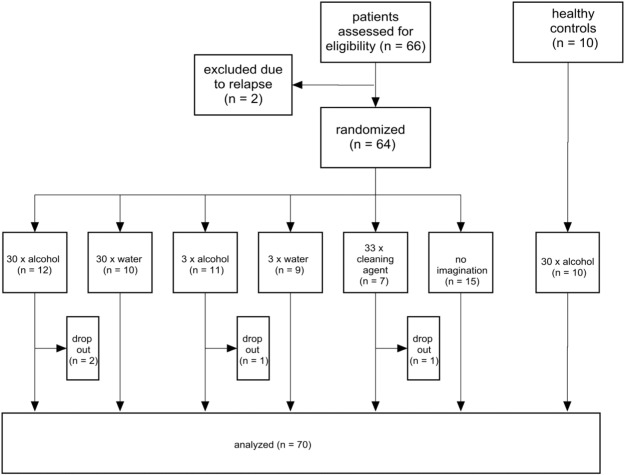
Fig. 1 shows the flow diagram of the study. Sixty-six alcohol-dependent patients were initially assessed for eligibility, two patients dropped-out before randomization due to relapse. Sixty-four patients were randomized to the six intervention groups, four patients dropped out immediately. A total of 60 alcohol-dependent patients and ten healthy controls were finally analysed. The characteristics of the study participants are shown in Table 1.
|
|
|
Fig. 1. Flow diagram of the study. |
| Characteristics of study participants | Alcohol-dependent patients | Healthy controls | |||||
|---|---|---|---|---|---|---|---|
| Group 1 30 × alcohol | Group 2 30 × water | Group 3 3 × alcohol | Group 4 3 × water | Group 5 33 × cleaning agent | Group 6 No imagination | Group 7 30 × alcohol | |
| n = 10 | n = 10 | n = 10 | n = 9 | n = 6 | n = 15 | n = 10 | |
| Age [mean ± SD (range)] | 43.4 ± 13.1 (25–68) | 40.9 ± 10.2 (26–55) | 44.7 ± 8.6 (31–57) | 48.7 ± 10.9 (35–65) | 43 ± 8.7 (30–50) | 44.3 ± 11.6 (27–62) | 37 ± 9.4 (28–58) |
| Sex [n (%)] | |||||||
| Female | 2 (20) | 3 (30) | 1 (10) | 4 (44.4) | 1 (16.7) | 4 (26.7) | 4 (40) |
| Male | 8 (80) | 7 (70) | 9 (90) | 5 (55.6) | 5 (83.3) | 11 (73.3) | 6 (60) |
| Family status [n (%)] | |||||||
| In relationship | 4 (40) | 6 (60) | 6 (60) | 4 (44.1) | 2 (33.3) | 9 (60) | 6 (60) |
| No relationship | 4 (40) | 4 (40) | 3 (30) | 4 (44.1) | 4 (66.7) | 6 (40) | 4 (40) |
| Missing data | 2 (20) | 1 (10) | 1 (11.1) | ||||
| Highest school qualification [n (%)] | |||||||
| None | 1 (10) | ||||||
| School for handicapped children | 1 (10) | 2 (16.3) | |||||
| Secondary modern school-leaving certificate, year 5–9 | 1 (10) | 1 (10) | 1 (16.7) | 3 (20) | |||
| Secondary modern school-leaving certificate, year 5–10 | 4 (40) | 3 (30) | 4 (44.4) | 1 (16.7) | 6 (40) | 1 (10) | |
| University-entrance diploma | 5 (50) | 5 (50) | 6 (60) | 5 (55.6) | 4 (66.7) | 3 (20) | 9 (90) |
| Missing data | 1 (10) | 1 (10) | 1 (10) | 1 (6.7) | |||
| Educational status [n (%)] | |||||||
| None | 2 (20) | ||||||
| Technical college | 7 (70) | 6 (60) | 4 (40) | 5 (55.6) | 3 (50) | 1 (10) | |
| University degree | 2 (20) | 2 (20) | 5 (50) | 4 (44.4) | 3 (50) | 9 (90) | |
| Missing data | 1 (10) | 1 (10) | |||||
| Employment status [n (%)] | |||||||
| Unemployed | 3 (30) | 4 (40) | 4 (40) | 5 (55.6) | 2 (33.3) | 4 (26.7) | |
| Employed | 6 (60) | 6 (60) | 5 (50) | 4 (44.4) | 4 (66.7) | 10 (66.7) | 10 (100) |
| Missing data | 1 (10) | 1 (10) | 1 (6.7) | ||||
| Number of previous detoxifications [n (%)] | |||||||
| None | 5 (50) | 5 (50) | 4 (40) | 5 (55.6) | 1 (16.7) | 6 (40) | |
| Up to two | 1 (10) | 2 (20) | 2 (20) | 2 (22.2) | 1 (16.7) | 3 (20) | – |
| More than three | 2 (20) | 3 (30) | 3 (30) | 2 (22.2) | 3 (50) | 5 (36.3) | |
| Missing data | 2 (20) | 1 (10) | 1 (16.7) | 1 (6.7) | |||
| Years of hazardous alcohol consumption [mean ± SD] | 10.6 ± 6.8 | 8.2 ± 5.4 | 11.6 ± 4.6 | 8.7 ± 8.6 | 9.7 ± 4.5 | 12.9 ± 6.5 | – |
| Alcohol consumption (grams) per day before inclusion [mean ± SD] | 114.4 ± 30 | 178 ± 123.1 | 143.6 ± 53.3 | 215.6 ± 67.3 | 148.3 ± 43.1 | 152.7 ± 82.2 | – |
| Smoking status [n (%)] | |||||||
| Smoker | 5 (50) | 7 (70) | 7 (70) | 7 (77.8) | 4 (66.7) | 11 (73.3) | 5 (50) |
| Nonsmoker | 3 (30) | 3 (30) | 1 (10) | 2 (22.2) | 1 (33.3) | 4 (26.7) | 5 (50) |
| Missing data | 2 (20) | 2 (20) | |||||
| Other psychiatric diagnoses [n (%)] | |||||||
| None | 8 (80) | 6 (60) | 4 (40) | 6 (66.7) | 3 (50) | 9 (60) | 10 (100) |
| Psychiatric comorbidity | 2 (20) | 4 (40) | 4 (40) | 3 (33.3) | 3 (50) | 6 (40) | |
| Missing data | 2 (20) | ||||||
| Other drug use [n (%)] | |||||||
| None | 8 (80) | 6 (60) | 6 (60) | 9 (100) | 4 (66.7) | 11 (73.3) | 10 (100) |
| Cannabis | 2 (20) | 1 (10) | 1 (16.7) | 1 (6.7) | |||
| Other | 2 (20) | 3 (30) | 1 (16.7) | 2 (16.3) | |||
| Missing data | 2 (20) | 1 (6.7) | |||||
| Medication [n (%)] | |||||||
| No psychotropic medication | 7 (70) | 6 (60) | 4 (40) | 6 (66.7) | 3 (50) | 12 (80) | 10 (100) |
| Antidepressants | 1 (10) | 3 (30) | 2 (20) | 1 (11.1) | 2 (33.3) | 2 (16.3) | |
| Naltrexon | 1 (10) | 1 (10) | 1 (11.1) | ||||
| Benzodiazepines | 1 (11.1) | 1 (16.7) | |||||
| Other | 1 (10) | 1 (6.7) | |||||
| Missing data | 1 (10) | 3 (30) | |||||
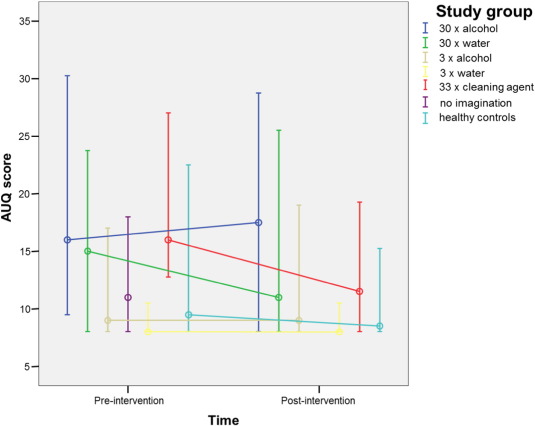
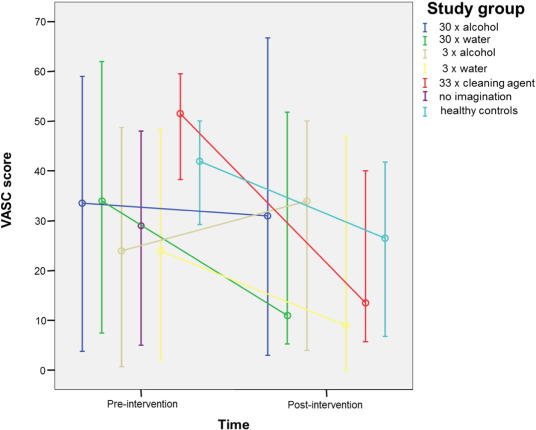
A RM MANOVA of the AUQ before and after intervention showed a significant effect by group (p = 0.002) and a significant interaction of group × time (p < 0.001). Also, a significant effect by group (p = 0.031) and a significant interaction of group × time (p < 0.001) were found for the VASC pre- and post-intervention.
Group 1 (imagination of drinking the preferred alcoholic drink, 30 times) did not show significant reductions in craving after intervention as measured by the AUQ (median pre-intervention: 16; median post-intervention: 17.5; p = 0.617) and the VASC (median pre-intervention: 33.5; median post-intervention: 31; p = 0.777). Patients of group 2 (imagination of drinking water, 30 times) did also not show significant changes in craving after intervention (AUQ: median pre-intervention: 15; median post-intervention: 11; p = 0.21; VASC: median pre-intervention: 34; median post-intervention: 11; p = 0.109).
No changes in craving after imagination could be observed in patients of group 3 (imagination of drinking the preferred alcoholic drink, 3 times; AUQ: median pre-intervention: 9; median post-intervention: 9; p = 0.709; VASC: median pre-intervention: 24; median post-intervention: 34; p = 0.891).
Group 4 (imagination of drinking water, 3 times) did also not show significant changes in craving (AUQ: median pre-intervention: 8; median post-intervention: 8; p = 0.717; VASC: median pre-intervention: 24; median post-intervention: 9; p = 0.339).
Patients of group 5 (imagination of filling a cup of cleaning agent into a washing machine, 33 times, control condition) showed a significant decrease in craving after intervention (AUQ: median pre-intervention: 16; median post-intervention: 11.5; p < 0.001; VASC: median pre-intervention: 51.5; median post-intervention: 13.5; p < 0.001).
Patients randomized to group 6 (no imagination, but identical clinical procedure at the outpatient unit), were only included in the analyses of the number of study sessions. A comparison of completed study sessions of each group with this group did not reveal significant differences (Mann Whitney U test, p > 0.01).
In the group of healthy controls (group 7, imagination of drinking the preferred alcoholic drink, 30 times), a significant decrease in the urge to drink, measured by AUQ (median pre-intervention: 9.5; median post-intervention: 8.5; p = 0.004) and VASC (median pre-intervention: 42; median post-intervention 26.5; p = 0.024) was found after imagination.
After adjusting for baseline measurements, a RM MANCOVA only yielded nearly significant differences across groups (AUQ: DF = 4.55, p = 0.11; VASC: DF = 3.72, p = 0.067). However, pairwise comparison of group 1 (imagination of drinking the preferred alcoholic drink, 30 times) with group 5 (imagination of filling a cup of cleaning agent into a washing machine, 33 times, control condition) led to a significant difference in AUQ (DF = 1, p = 0.005) and VASC scores (DF = 1, p = 0.004) and a difference in AUQ compared to group 7 (healthy controls, imagination of drinking the preferred alcoholic drink, 30 times) which fell short of statistical significance (DF = 1, p = 0.146).
Changes in craving during the first intervention (pre-/post-imagination) of all groups as measured by AUQ and VASC are shown in Fig. 2 ; Fig. 3. Table 2 shows the number of completed study sessions in all groups except for healthy controls who performed only one session. Due to the high drop-out rate throughout the study, only the first session has been included in the analysis of the levels of craving. Group 6 (no imagination) was only included in the analysis of the number of study sessions.
|
|
|
Fig. 2. AUQ scores (median and 25%–75% quartiles) of each study group pre- and post-intervention. |
|
|
|
Fig. 3. VASC scores (median and 25%–75% quartiles) of each study group pre- and post-intervention. |
| Study group | Mean | SD | Median | Min | Max |
|---|---|---|---|---|---|
| 30 × alcohol | 3.8 | 2.4 | 4.5 | 1 | 6 |
| 30 × water | 3.4 | 2.2 | 3 | 1 | 6 |
| 3 × alcohol | 5.2 | 1.5 | 6 | 2 | 6 |
| 3 × water | 4 | 2.5 | 6 | 1 | 6 |
| 33 × cleaning agent | 5.7 | 0.8 | 6 | 4 | 6 |
| No imagination | 3.4 | 2.3 | 4 | 1 | 6 |
Descriptive statistics (mean, SD, median and minimum/maximum) of the number of completed study sessions in each study group.
4. Discussion
The present pilot study evaluated repetitive imaginary cue-exposure to reduce craving in recently abstinent alcohol-dependent patients. Previous studies focussed on the effects of in vivo cue-exposure ( Rohsenow et al., 2001) or thinking about negative consequences of drinking (Naqvi et al., 2015) on the level of craving. We hypothesized a reduction of craving in subjects who imagined drinking their preferred alcoholic drink repetitively since a previous study in healthy subjects found a significant decrease in real chocolate consumption as a result of repetitive imagination of chocolate consumption (Morewedge et al., 2010). The authors concluded that these findings were a consequence of habituation which has also been explored in the research area of food intake ( Epstein et al., 2009; Morewedge et al., 2010 ; Wisniewski et al., 1992).
Intriguingly, alcohol-dependent patients showed no reductions in craving scores after the first imagination session, whereas, in line with the findings of Morewedge and co-workers (Morewedge et al., 2010), healthy subjects showed a nearly significant decrease in the urge to drink alcohol after applying the same imagination protocol in our study. Control groups imagining drinking of water did not show any significant changes in craving. Interestingly, the group imagining performing an analogous movement without cues of alcohol or drinking (filling a washing machine with cleaning agent) showed a reduction in craving. It is possible that this finding is related to the absence of the desired target within this protocol (i.e., alcohol). However, conclusions cannot be drawn due to the small sample size of this group (n = 6).
More importantly, craving was not reduced in patients of both groups that imagined the consumption of alcohol repetitively (3 vs. 30 times), potentially indicating that even a high number of repetitions might not be sufficient to engender habituation. These preliminary results might indicate an aberrant ability to habituate to alcohol-related stimuli in abstinent alcohol-dependent patients. Findings from studies investigating cue-reactivity in alcohol-dependent patients using fMRI suggest an altered central processing of alcohol-related stimuli in alcohol dependence (Myrick et al., 2004 ; Wrase et al., 2002). Also, our preliminary results are partially in line with the findings of a study in moderate to heavy smokers, who reported constant craving for cigarettes in consequence of cue-exposure on several days (Miranda et al., 2008).
Desire thinking has been reported to have a significant effect on the occurrence of craving (Caselli et al., 2013). However, since we did not assess desire thinking by questionnaires such as the DTQ (Caselli & Spada, 2011) in our study, no clear conclusions on the role of desire thinking in the modulation of craving can be made.
Our preliminary results indicate that repetitive in sensu cue-exposure therapy might not reduce craving in alcohol-dependent patients. Possibly, a different protocol including a higher number of repetitions during a longer period of time is needed to induce habituation to alcohol-related stimuli in patients with AUD. On the contrary, an aberrant ability to habituate to alcohol-related stimuli might be a key component of the pathology in alcohol dependence. One might argue that habituation is only relevant in the modification of responses related to aversive stimuli and not applicable to appetitive stimuli. However, research regarding food intake suggests that habituation also occurs after repeated presentation of appetitive stimuli ( Coelho et al., 2014 ; Morewedge et al., 2010).
Park and co-workers recently investigated the efficacy of virtual reality cue-exposure techniques on craving in gamblers (Park et al., 2015). In contrast to our study, a significant reduction in urges to gamble after repetitive virtual cue-exposure was found. Interestingly, the study was not conducted in individuals who fulfilled the diagnostic criteria for pathological gambling. Thus, one might speculate that subjects with addictive disorders might have shown divergent responses. A recent review of studies on the use of virtual reality in the assessment of craving and the treatment of substance use disorders revealed craving induction during virtual cue-exposure in most studies (Hone-Blanchet, Wensing, & Fecteau, 2014). However, results concerning the therapeutic potential of virtual reality were inconsistent and mainly hard to compare. Also, most of these studies only investigated nicotine abuse/dependence. Nevertheless, in line with our preliminary findings, craving was not significantly decreased by therapeutic use of virtual reality cue-exposure in the majority of the reviewed trials (Hone-Blanchet, Wensing, et al., 2014).
Several limitations of our pilot study need to be addressed. First, we only assessed effects of repetitive imagination of alcohol consumption in abstinent patients after detoxification treatment; the degree to which these findings also extend to other phases of alcohol dependence (e.g., currently drinking patients) remains unclear. Second, the sample size of each group was far too small to draw clear conclusions, although several control conditions were integrated in the study design.
Taken together, our preliminary results indicate that the repetitive imagination of alcohol consumption does not lead to a consecutive craving reduction in patients with AUD. It is possible, that the ability to habituate to alcohol-related stimuli during in sensu cue-exposure is impaired in alcohol-dependent patients. Future clinical trials with larger samples and varying imagination protocols are needed to evaluate the effects of repetitive imaginary alcohol consumption on craving in alcohol-dependent patients.
Role of the funding source
Not applicable.
The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Contributors
Study idea and design: OG and CM.
Data collection and analysis: MS, JB, OG, KDW, CM.
Data interpretation: MS, JB, OG, KDW, CM.
Writing of the first draft: OG.
All authors contributed to the writing of the manuscript and approved the final version before submission.
Declaration of interest
O. Geisel has received travel grant support from Lundbeck. C.A. Müller has received research grant support and speaker honoraria from Lundbeck. Julia Behnke, Michael Schneider and Klaus-Dieter Wernecke reported no conflicts of interest.
Acknowledgements
We thank all patients who contributed to this study and our clinical study staff for their work.
References
- Abramowitz, 2013 J.S. Abramowitz; The practice of exposure therapy: Relevance of cognitive-behavioral theory and extinction theory; Behavior Therapy, 44 (4) (2013), pp. 548–558
- Anton, 1999 R.F. Anton; What is craving? Models and implications for treatment; Alcohol Research & Health, 23 (3) (1999), pp. 165–173
- Averbuch and Katzper, 2004 M. Averbuch, M. Katzper; Assessment of visual analog versus categorical scale for measurement of osteoarthritis pain; Journal of Clinical Pharmacology, 44 (4) (2004), pp. 368–372
- Back et al., 2007 S.E. Back, S. Gentilin, K.T. Brady; Cognitive-behavioral stress management for individuals with substance use disorders: pilot study; The Journal of Nervous and Mental Disease, 195 (8) (2007), pp. 662–668
- Bathke and Brunner, 2003 A. Bathke, E. Brunner; A nonparametric alternative to analysis of covariance; Elsevier B.V, Amsterdam (2003)
- Bohn et al., 1995 M.J. Bohn, D.D. Krahn, B.A. Staehler; Development and initial validation of a measure of drinking urges in abstinent alcoholics; Alcoholism, Clinical and Experimental Research, 19 (3) (1995), pp. 600–606
- Bottlender et al., 2007 M. Bottlender, R. Spanagel, M. Soyka; One drink, one drunk—controlled drinking by alcoholics? 3-year-outcome after intensive outpatient treatment; Psychotherapie, Psychosomatik, Medizinische Psychologie, 57 (1) (2007), pp. 32–38
- Brunner et al., 2002 E. Brunner, S. Domhof, F. Langer; Nonparametric analysis of longitudinal data in factorial experiments; Wiley & Sons, New York (2002)
- Carter and Tiffany, 1999 B.L. Carter, S.T. Tiffany; Meta-analysis of cue-reactivity in addiction research; Addiction, 94 (3) (1999), pp. 327–340
- Caselli and Spada, 2011 G. Caselli, M.M. Spada; The desire thinking questionnaire: Development and psychometric properties; Addictive Behaviors, 36 (11) (2011), pp. 1061–1067
- Caselli and Spada, 2015 G. Caselli, M.M. Spada; Desire thinking: What is it and what drives it?; Addictive Behaviors, 44 (2015), pp. 71–79
- Caselli et al., 2012 G. Caselli, M. Ferla, C. Mezzaluna, F. Rovetto, M.M. Spada; Desire thinking across the continuum of drinking behaviour; European Addiction Research, 18 (2) (2012), pp. 64–69
- Caselli et al., 2013 G. Caselli, M. Soliani, M.M. Spada; The effect of desire thinking on craving: An experimental investigation; Psychology of Addictive Behaviors, 27 (1) (2013), pp. 301–306
- Coelho et al., 2014 J.S. Coelho, C. Nederkoorn, A. Jansen; Acute versus repeated chocolate exposure: Effects on intake and cravings in restrained and unrestrained eaters; Journal of Health Psychology, 19 (4) (2014), pp. 482–490
- Conklin and Tiffany, 2001 C.A. Conklin, S.T. Tiffany; The impact of imagining personalized versus standardized urge scenarios on cigarette craving and autonomic reactivity; Experimental and Clinical Psychopharmacology, 9 (4) (2001), pp. 399–408
- Conklin and Tiffany, 2002 C.A. Conklin, S.T. Tiffany; Applying extinction research and theory to cue-exposure addiction treatments; Addiction, 97 (2) (2002), pp. 155–167
- Corty and McFall, 1984 E. Corty, R.M. McFall; Response prevention in the treatment of cigarette smoking; Addictive Behaviors, 9 (4) (1984), pp. 405–408
- Critchley and Rolls, 1996 H.D. Critchley, E.T. Rolls; Hunger and satiety modify the responses of olfactory and visual neurons in the primate orbitofrontal cortex; Journal of Neurophysiology, 75 (4) (1996), pp. 1673–1686
- Epstein et al., 1992 L.H. Epstein, J.S. Rodefer, L. Wisniewski, A.R. Caggiula; Habituation and dishabituation of human salivary response; Physiology & Behavior, 51 (5) (1992), pp. 945–950
- Epstein et al., 2009 L.H. Epstein, J.L. Temple, J.N. Roemmich, M.E. Bouton; Habituation as a determinant of human food intake; Psychological Review, 116 (2) (2009), pp. 384–407
- Heinz et al., 2009 A. Heinz, A. Beck, S.M. Grusser, A.A. Grace, J. Wrase; Identifying the neural circuitry of alcohol craving and relapse vulnerability; Addiction Biology, 14 (1) (2009), pp. 108–118
- Hone-Blanchet et al., 2014 A. Hone-Blanchet, T. Wensing, S. Fecteau; The use of virtual reality in craving assessment and cue-exposure therapy in substance use disorders; Frontiers in Human Neuroscience, 8 (2014), p. 844
- Kadden, 2001 R.M. Kadden; Behavioral and cognitive-behavioral treatments for alcoholism: Research opportunities; Addictive Behaviors, 26 (4) (2001), pp. 489–507
- Kavanagh et al., 2005 D.J. Kavanagh, J. Andrade, J. May; Imaginary relish and exquisite torture: The elaborated intrusion theory of desire; Psychological Review, 112 (2) (2005), pp. 446–467
- Kemps and Tiggemann, 2014 E. Kemps, M. Tiggemann; A role for mental imagery in the experience and reduction of food cravings; Frontiers in Psychiatry, 5 (2014), p. 193
- Lang, 1977 P. Lang; Imagery in therapy: An information processing analysis of fear; Behavioral Therapy, 8 (1977), p. 862
- Ludwig and Wikler, 1974 A.M. Ludwig, A. Wikler; ‟Craving” and relapse to drink; Quarterly Journal of Studies on Alcohol, 35 (1) (1974), pp. 108–130
- Magill and Ray, 2009 M. Magill, L.A. Ray; Cognitive-behavioral treatment with adult alcohol and illicit drug users: A meta-analysis of randomized controlled trials; Journal of Studies on Alcohol and Drugs, 70 (4) (2009), pp. 516–527
- Miranda et al., 2008 R. Miranda Jr., D.J. Rohsenow, P.M. Monti, J. Tidey, L. Ray; Effects of repeated days of smoking cue exposure on urge to smoke and physiological reactivity; Addictive Behaviors, 33 (2) (2008), pp. 347–353
- Morewedge et al., 2010 C.K. Morewedge, Y.E. Huh, J. Vosgerau; Thought for food: Imagined consumption reduces actual consumption; Science, 330 (6010) (2010), pp. 1530–1533
- Mottola, 1993 C.A. Mottola; Measurement strategies: The visual analogue scale; Decubitus, 6 (5) (1993), pp. 56–58
- Myers, 2008 D.G. Myers; Psychologie; Springer Medizin Verlag, Heidelberg (2008)
- Myrick et al., 2004 H. Myrick, et al.; Differential brain activity in alcoholics and social drinkers to alcohol cues: Relationship to craving; Neuropsychopharmacology, 29 (2) (2004), pp. 393–402
- Naqvi et al., 2015 N.H. Naqvi, et al.; Cognitive regulation of craving in alcohol-dependent and social drinkers; Alcoholism, Clinical and Experimental Research, 39 (2) (2015), pp. 343–349
- Niaura et al., 1988 R.S. Niaura, D.J. Rohsenow, J.A. Binkoff, P.M. Monti, M. Pedraza, D.B. Abrams; Relevance of cue reactivity to understanding alcohol and smoking relapse; Journal of Abnormal Psychology, 97 (2) (1988), pp. 133–152
- Park et al., 2015 C.B. Park, et al.; The effect of repeated exposure to virtual gambling cues on the urge to gamble; Addictive Behaviors, 41 (2015), pp. 61–64
- Rohsenow et al., 2001 D.J. Rohsenow, et al.; Cue exposure with coping skills training and communication skills training for alcohol dependence: 6- and 12-month outcomes; Addiction, 96 (8) (2001), pp. 1161–1174
- Tiffany and Drobes, 1990 S.T. Tiffany, D.J. Drobes; Imagery and smoking urges: The manipulation of affective content; Addictive Behaviors, 15 (6) (1990), pp. 531–539
- Vollstadt-Klein et al., 2011 S. Vollstädt-Klein, et al.; Effects of cue-exposure treatment on neural cue reactivity in alcohol dependence: A randomized trial; Biological Psychiatry, 69 (11) (2011), pp. 1060–1066
- World Health Organization (WHO), 1994 World Health Organization (WHO); Internationale Klassifikation psychischer Störungen ICD-10 Kapitel V (F) Forschungskriterien; H. Dilling, W. Mombour, M.H. Schmidt, E. Schulte‐Warkwort (Eds.)Huber, Bern (1994)
- Wisniewski et al., 1992 L. Wisniewski, L.H. Epstein, A.R. Caggiula; Effect of food change on consumption, hedonics, and salivation; Physiology & Behavior, 52 (1) (1992), pp. 21–26
- Wrase et al., 2002 J. Wrase, et al.; Development of alcohol-associated cues and cue-induced brain activation in alcoholics; European Psychiatry, 17 (5) (2002), pp. 287–291
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?