Highlights
- A new our self designed TEN was used for clavicular fractures.
- The new TENs were individual designed with various types for different patients.
- Satisfactory clinical therapeutic effects and few complications were obtained.
Abstract
Objectives
The aim of this study was to evaluate clinical results of a new design titanium elastic nail (TEN) for displaced midshaft clavicular fractures.
Patients and methods
Between February 2012 and December 2013, a total 36 patients with displaced midshaft clavicular fractures were treated with intramedullary nailing stabilization with our new design TEN. Blood loss, mean times of operation, postoperative complications, hospital stays and time to bone union was recorded. The outcomes were evaluated with radiographic assessment, visual analog scale (VAS) score, the Constant-Murley, and the disabilities of the arm, shoulder, and hand (DASH) scores.
Results
The mean blood loss was 50.278 ± 10.753 ml, while the mean operation, hospital stay and bone union times were 46.417 ± 9.232 min, 10.056 ± 2.672 days and 11.583 ± 2.729 weeks, respectively. After removal of the TENs at a mean of 10.2 months (range, 8-13 months) after surgery, no re-fracture and nonunion was found in any patient. Two cases of shoulder back stabbing pain were spontaneously resolved later. The mean fracture healing time was 12 weeks. The VAS score and motion ranges of shoulder joint were significantly improved postoperatively (P < 0.001). The shoulder function recovery showed the excellent results with the mean Constant-Murley score of 93.389 ± 2.749 and DASH scores of 2.528 ± 1.567.
Conclusion
Our new TEN design used in intramedullary fixation might be a safe and effective technique for treatment of displaced midshaft clavicular fractures.
Level of evidence: Level IV, therapeutic study .
Keywords
Displaced midshaft clavicular fractures ; Titanium elastic nail ; Minimally invasive treatment
Introduction
Clavicular fracture, constitutes 2.6%–5% of all adult fractures, most are located in the midshaft clavicle with different degrees of displacement.1 ; 2 ; 3 Conservative methods are commonly used for midshaft clavicular fractures treatment, but with various unsatisfactory complications such as nonunion, malunion and shoulders asymmetry.4 ; 5 ; 6 The rate of malunion after conservative treatment for the midshaft clavicular fractures reached 15%, and 30% patients were unsatisfied.7
Recently, early surgical treatment for the midshaft clavicular fractures could greatly reduce the incidence rate of nonunion and malunion.8 Open reduction and plate-screw fixation was considered as the gold standard with the advantages of firm fixation and earlier postoperative mobilization, but also with disadvantages of larger incision and more organizations being exposed, presenting with many postoperative complications.9 ; 10 ; 11 Intramedullary fixation treatment for midclavicular fractures has been favored due to its strengths including small incision, less periosteal striping, dispersion of stress and simple to operate.12 However, early intramedullary implants, such as Hagie pins and Kirschner wires, have been gradually replaced due to insufficient stability.13 ; 14 In addition, various nails such as elastic stable intramedullar nails (ESIN) and locking flexible clavicular nails was widely used.15 ; 16 However, ESIN has been reported with too many complications including radiographic malunion, superficial wound infection and transient neurologic malunion.17 Besides, locking flexible clavicular nails was also with various risks, such as disturbing irritation at the entry point.18 In 2002, titanium elastic nail (TEN) was firstly applied in the treatment of displaced midclavicular fractures, and showed good clinical therapeutic outcomes as an alternative to conservative treatment but with the poor force of anti-rotation and anti-shortening.19 Common TEN might induced various complications including hardware irritations, medial perforations, lateral penetrations, TEN breakage and dislocation.21 In 44% of patients, complications and problems occurred (8 medial migration and 12 clavicular shortening of > or = 5 mm).22 Therefore, the technique of intramedullary nailing should be improved to reduce the postoperative complications.
In order to overcome these problems, a new titanium elastic intramedullary nail was designed and applied in this study to assess the clinical therapeutic outcome for the treatment of displaced midshaft clavicular fractures.
Materials and methods
Patients
Between February 2012 and December 2013, a total of 36 patients including 30 males and 6 females with displaced midshaft clavicular fractures were treated with intramedullary nailing stabilization by our self-designed TEN (Puwei Medical Appliances Inc., Shanghai, China) in our hospital for this prospective study.
Inclusion criteria and exclusion criteria
Selection criteria: (1) Type IIA2 (angulation > 45°) or IIB1 (shortening or overlapping displacement length > 2 cm) fresh unilateral midshaft clavicular fractures according to Robinson classification2 ; (2) the range of age were 28–60 years old; (3) patient without underlying diseases such as primary hypertension and cardiac diseases. Exclusion criteria: (1) pathological fractures; (2) multiple injuries of upper limbs; (3) open fractures; (4) combined with injuries of blood vessels or nerves; (5) other diseases which affected the functions of upper limbs.
Standard protocol approvals and patient consents
All human studies were authorized by the Hospital Ethics Committee and conducted in accordance with the ethical standards. The written informed consent was obtained from all study patients.
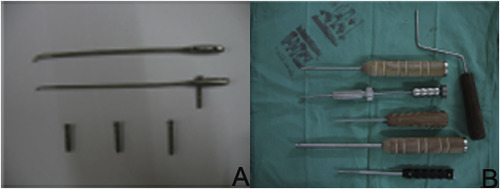
Characteristics of our self-designed TEN
A new TEN (patent number: ZL201220224352.1) was designed by ourselves and made of Titanium alloy (TC4), with the diameter 2.0–3.0 mm and the length of 12–15 cm (Fig. 1 A). The diameter of TEN was selected to be smaller than medullary canal. The nail head, body and tail were short-arc, cylindrical, and swollen cylindrical shaped, respectively. There were two holes (2.8 mm in diameter and 10 mm between two holes) in the tail. The proximal hole was the locking hole, while and the distal hole was used for implanting and extraction the nail. The locking screws with a diameter of 2.6 mm and the length of 20–40 mm locked into the fixation device with its screws. The conical cutter was designed as the shape of sharp triangular ceratoid, while the elastic nail holding device was designed as a hollow cylindrical shape with a hole of 0.3 mm in the diameter at the head. The head end of pulling device was designed as a hooked shape, and the tail end was designed with a sliding hammer (Fig. 1 B).
|
|
|
Fig. 1. The characteristics of our self-designed TEN and operative instruments. (A) the our self designed TEN used in the operation; (B) frequently-used accessories during operation. |
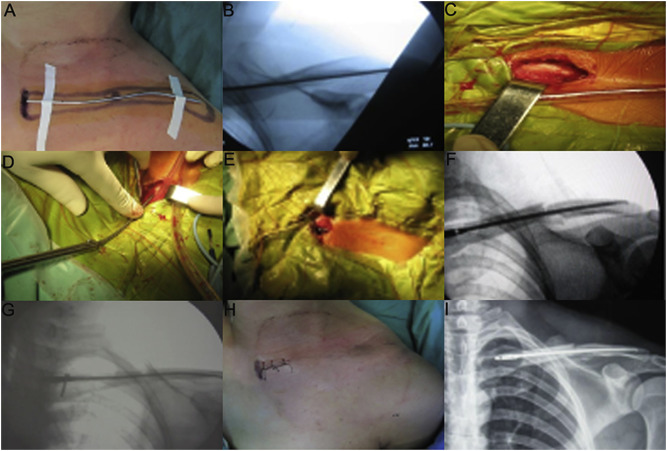
Surgical procedures
All the patients were positioned on a radiolucent operating table and performed by general anesthesia. Preoperatively, preliminarily closed reduction was processed. Then the inner end and outer end of the clavicle were marked outside the skin with Kirschner wire (Fig. 2 A). After confirming that the outer end of Kirschner wire was located at 1.5 cm from the inner part of the clavicular outer end and its long axis was overlapped with the clavicle using C-arm fluoroscopy device. The duration of fluoroscopy use was chosen based on the insert and fixed time of each patient. In addition, pre and postoperative measurements of the clavicle dimensions were taken by the experiment patients under C-arm fluoroscopy device. The initial length of TEN was determined by the length of remained Kirschner wire (Fig. 2 B). A conical cutter was applied for opening aperture of anterior cortex of the clavicle inner part, and the incision was expanded by our self-designed diamond-shaped medullary cavity file (Fig. 2 C). Afterward, the TEN with predicted length was inserted by a holding device, which was advanced gradually under fluoroscopic control (Fig. 2 D and E). If it was too hard to finish the closed reduction, a transverse small incision was made at the fracture site to assist reduction. In this situation, the periosteum of the fracture end was not stripped, and larger free bone fragment could be bundled up to the fracture end using double 7th silk suture (Johnson Inc., New Brunswick, NJ, USA). During operation, the reduction of fracture and the location of TEN were examined by C-arm fluoroscopy device which patients were positioned on it (Fig. 2 F). If the tail of TEN was slightly longer, the tail part could be tapped gently using homemade stick to assure it parallel to the cortex of clavicle inner end. Finally, the TEN was locked with screw and the small incision was sewed up (Fig. 2 G and H). X-ray radiography below the shoulder with clavicular fractures was routinely used to examine the reduction of fracture and the location of TEN (Fig. 2 I). In all the operations, surgeons were with at least 10 years' experience. Moreover, similar treatment and nursing methods before and after the operation were used to the patients.
|
|
|
Fig. 2. Surgical procedures of intramedullary nailing using our self-designed TEN. (A) external location with Kirschner wire; (B) the length of TEN measured under the fluoroscopic control of C-arm machine; (C) the medullary cavity opening with a small size incision in the inner end of clavicle; (D) the insertion of TEN from the inner end of clavicle; (E) the outlook after TEN is completely inserted into the medullary cavity; (F) a good position of TEN is seen using C-arm machine; (G) locking the screw at the tail part of TEN; (H) the postoperative outlook of small size incision; (I) a radiograph obtained just after surgery shows a good position of TEN and satisfactory reduction of fracture. |
Postoperative management
All patients were treated with arm sling after operation for 6 weeks. In addition, 3 days after surgery, patients were allowed to do passive anteflexion and abduction motion of shoulder joint under the guidance of physiotherapists, and the motion range could be increased gradually depending on the degree of pain. However, the range of passive anteflexion and abduction motion was kept within 90° in 6 weeks after surgery, and the weight-bearing exercise was not allowed. The range of passive and active motion were increased gradually according to the condition of fracture union and the weight-bearing exercise was begun gradually after 6 weeks postoperatively. The postoperative follow-up visits were scheduled every two weeks until bone union and every 3 months after bone union.
Evaluation of therapeutic efficiency
The operative data were recorded and analyzed, including operation time, blood loss, hospital stays and postoperative complications. The standards of bone union included the formation of continuous callus and the disappearance of fracture line, no tenderness of the fracture ends, and no subjective pain when performing active sports and weight-bearing activities on the clinical examinations. When the nail was advanced laterally by tearing the cortex, X-ray radiography was used to check checked that it did not protrude from the clavicle. The evaluation was made by an independent physician, blinded to the type of surgery and implant. The improvement of subjective pain was assessed using a visual analog scale (VAS) at 1 day before surgery and 3 days after surgery.23 The flexion and abduction motion ranges of shoulder joint were recorded from one day before surgery to the last follow-up.24 Shoulder function was assessed with the Constant-Murley score (range: 0–100 points, best: 100)25 and the Disabilities of the Arm, Shoulder and Hand (DASH) score (range: 0–100 points, best: 0)26 at the last follow-up. In detail, Constant-Murley scores are categorized as follows: excellent (90–100), good (80–89), satisfactory (70–79), and fair (<70). DASH scores of 0–10 are considered as an excellent result, and score >40 is associated with poor shoulder function. When the nail was advanced laterally by tearing the cortex, X-ray radiography was used to check checked that it did not protrude from the clavicle.
Statistical analysis
All the statistical analysis was performed with SPSS version 16.0 software (SPSS Inc., Chicago, IL, USA). The values were presented as mean ± SD. The data were analyzed using the method of paired t test and P < 0.05 was considered statistically significant.
Results
According to Robinson classification, there were 4 cases of type IIA2 and 32 cases of type IIB1 . Thereinto, 22 patients were in right midshaft clavicular fracture and 14 in left. The causes of fractures included traffic injuries (16 cases), sports injuries (10 cases), and injuries of falling off bicycles (10 cases) (Table 1 ). The surgeries were carried out in the following first-seventh days after injuries. The mean follow-up time was 15.472 ± 4.872 months. Among of these cases, 7 patients were followed up via telephone or questionnaire because they could not come to our hospital for recheck. And the data of physical examinations and radiographic inspections were provided by the local hospitals during follow-up. All the other patients were evaluated by the clinical function and imaging during the follow-up time. The mean operative time, peri-operative bleeding and hospital stays were 46.417 ± 9.232 min, 50.278 ± 10.753 ml and 10.056 ± 2.672 d, respectively. There were 11 cases performed with closed reduction, while the other 25 cases was operated by open reduction with small-size incision. No nonunion case was found in all the patients. The mean time of bone union was 11.583 ± 2.729 weeks (Table 2 ). Postoperative complications, such as infection, incision numbness, scar hyperplasia, irritation of nail end, withdrawal and breakage of nails, were not found. The mean diameter and length of our self-designed TEN used was 2.6 mm and 14 cm, respectively. The diameter range was 2.2 mm–3.0 mm, while the length range was 12.5 mm–15 mm. After recovery, the implant may cause the aseptic inflammation of muscle tissue around it. Thereby, the TENs were removed after a mean time of 10.2 months after surgery. No re-fracture occurred after removal.
| Items | Values |
|---|---|
| Age (years) | 33.3 ± 8.1 |
| Gender | |
| Male | 30 |
| Female | 6 |
| Fracture type | |
| Type IIA2 | 4 |
| Type IIB1 | 32 |
| Affected side | |
| Right clavicle | 22 |
| Left clavicle | 14 |
| Injury cause | |
| Traffic injury | 16 |
| Sports injury | 10 |
| Falling off bicycles | 10 |
Data are presented as mean ± SD or number.
| Items | Values | t | P |
|---|---|---|---|
| Operative time (min) | 46.417 ± 9.232 | ||
| Blood loss (ml) | 50.278 ± 10.753 | ||
| Bone union time (week) | 11.583 ± 2.729 | ||
| Constant-Murley scores | 93.389 ± 2.749 | ||
| DASH scores | 2.528 ± 1.567 | ||
| VAS scores | 26.216 | <0.001 | |
| Pre- | 8.139 ± 1.334 | ||
| Post- | 2.139 ± 1.496 | ||
| Flexion range | −26.007 | <0.001 | |
| Pre- | 24.167 ± 8.409 | ||
| Post- | 83.194 ± 12.372 | ||
| Abduction range | −30.979 | <0.001 | |
| Pre- | 19.306 ± 7.942 | ||
| Post- | 87.917 ± 12.557 |
Data are presented as mean ± SD. TEN, titanium elastic nail; DASH, disabilities of the arm, shoulder, and hand; VAS, visual analog scale.
Two patients complained of pain in back of shoulder postoperatively because the nail heads went through the lateral cortex during operation, and the pain symptoms were spontaneously resolved after 3 months. A 56-year-old female patient with osteoporosis presented with cortical dehiscence with defects at the opening site of the inner side of the clavicle in 1 week after surgery. The patient complained that the TEN tail could be touched under the skin, but with no skin irritation. The active and passive activities of this patient were immediately limited. 2 weeks after operation, the angular displacement at the fracture end aggravated with 10°, but without shortening displacement. Postoperative fracture healing time was 12 weeks. The remaining patients were found with no reduction failure or displacement aggravation during postoperative follow-up. One patient with cortical splitting and defect at the opening of TEN tail and one patient with shoulder joint outreach <90° were unsatisfied with the treatment, while the rest of the patients expressed satisfaction with the treatment outcome.
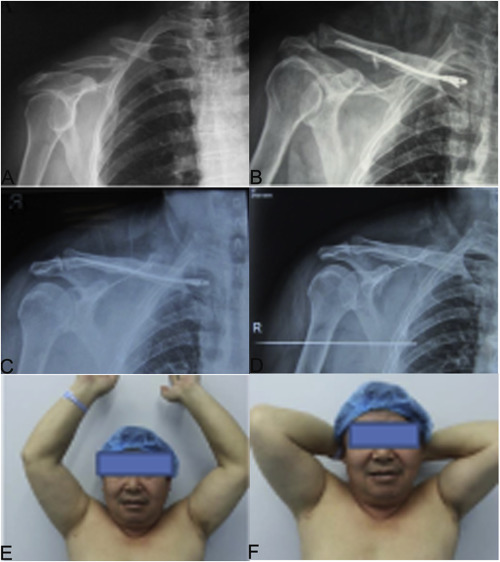
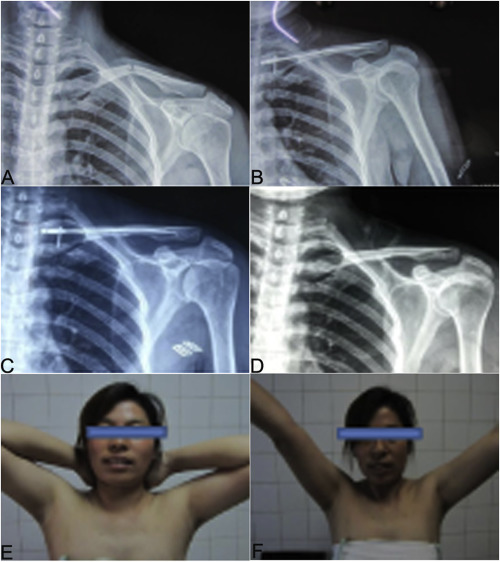
The mean VAS scores in 3d after operation were significantly lower (P < 0.001). The flexion and abduction motion ranges of shoulder joint were improved significantly at 2 weeks after surgery (P < 0.001). At the last follow-up, the mean Constant-Murley scores were 93.389 ± 2.749 ( Table 2 ). 86.11% patients showed excellent results and 13.89% showed good results. The mean DASH scores were 2.528 ± 1.567 (Table 2 ), and all the 36 patients showed excellent comprehensive recovery results. The typical cases were shown in Fig. 3 ; Fig. 4 .
|
|
|
Fig. 3. A 46 years old man with right-sided displaced midshaft clavicular fracture underwent intramedullary nailing using our self-designed TEN. (A) the preoperative radiograph shows a midclavicular fracture (Robinson type IIB1 ); (B) the postoperative radiograph of the implanted TEN shows good position; (C) a radiograph obtained at 4 months postoperatively shows bone healing; (D) a radiograph obtained at 10 months after surgery shows the restoration of the normal clavicular shape after TEN removal; (E) the maximum abduction motion range of shoulder joint after operation; (F) the maximum flexion motion range of shoulder joint after operation. |
|
|
|
Fig. 4. A 32 years old woman with left-sided displaced midshaft clavicular fracture was treated with intramedullary nailing using our self-designed TEN. (A) the preoperative radiograph shows a midclavicular fracture (Robinson type IIA2 ); (B) the postoperative radiograph of the implanted TEN shows good position; (C) a radiograph obtained 3 months postoperatively shows bone healing; (D) a radiograph obtained ar 12 months after surgery shows the restoration of the normal clavicular shape after TEN removal; (E) the excellent flexion motion range of shoulder joint after operation; (F) the good outcome of abduction motion range of shoulder joint after operation. |
Discussion
Compared with plate fixation, intramedullary fixation especially TEN fixation showed better clinical outcomes in the terms of operative time, wound size, subjective time to pain relief, and the postoperative functional scores of shoulder joint during the treatment of displaced midshaft clavicular fractures.27 In addition, TEN fixation provided a shorter average period of bone union, faster functional recovery, higher patient satisfaction, and a higher satisfaction with appearance.28 Common TENs anchored only with the arc-shaped nail head, and thereby leading to the poor dislocation capacity of anti-rotation and anti-axis.29 In addition, collar bone has characters including S-shaped, irregularity and narrow bone marrow cavity. Therefore, the large diameter of TEN was difficult to insert and even lead to split at the distal part of fracture. For the treatment of midshaft clavicular fractures, the average diameter of common used TEN was 2 mm.30 Besides, postoperative complications after intramedullary fixation with common TENs occurred frequently, including nail withdrawal, skin irritation, lateral perforation, and even shortening or dislocation at the fracture site.21 ; 22
Besides TEN, nails such as ESIN and the locking flexible clavicular nails are currently used in clavicular intramedullary fixation but with various problems. However, Lu et al reported that there are significantly displaced clavicle fractures with ESINs treatment.31 In order to solve these problems, Kaiser et al adopt pre-bending with more than 30° to improve the stability of the nail and also reduce the complications.32 In addition, the end caps used for elastic stable intramedullary nailing could also reduce the risk of altering construct stability.33 In this study, the new TEN could also solve this problem with more convenience.
In the present study, intramedullary fixation with our self-designed TEN was performed for the treatment of displaced midshaft clavicular fractures. During operation, the occurrence of the skin irritation was greatly reduced by TEN with appropriate diameters and length. In the previous study, the end and hook of nails should be cut off after implantation.27 Thereby, this new TEN could effectively reduce the stimulation of tail end. Moreover, the smaller radian design of our TEN head was in favor of nail insertion in the lateral end of the flat collar bone. In addition, the rotational and axial stability of nail body in the clavicular bone marrow cavity was enhanced and the postoperative complications was significantly reduced resulted in the tail part was designed as swollen cylindrical shaped with two holes. In addition, the TEN was designed with lock screw of full thread tapping type, and also retained the three-point-fixation methods. Therefore, the stability was more enhanced. As expected, all the 36 patients undergoing intramedullary fixation using our self-designed TEN obtained bone union with no withdrawal and breakage of nails after a mean follow up of 15.5 ± 4.9 months. Postoperative fracture healing time was 12 weeks. In addition, the mean Constant-Murley score (93.389 ± 2.749) the last follow-up was similar to the study by Jubel et al34 (mean 95) and Muller et al22 (95 ± 1.9), while the mean DASH scores in our study were lower than that in Mullers report22 (2.528 ± 1.567 vs 5 ± 2.3). Therefore, the clinical outcomes of our self designed TEN might be better in the intramedullary fixation for the treatment of displaced midshaft clavicular fracture. In addition, plate internal fixation should be prepared if the TEN IS failed to insert.
There are some limitations in the present study. Due to lack of randomized control group, the problems of whether our self-designed can be used in the treatment of Robinson IIB2 midshaft clavicular fracture should be further studied in the future clinical practice. And the equipment of assisting closed reduction should be designed. Besides, the small number of patients and short follow-up time were also the limitation in our study. Thus, a study of large population and long follow-up time should be conducted to further assess the clinical values of our self-designed TEN used in the intramedullary fixation for the treatment of displaced midshaft clavicular fracture. In addition, the difference between type IIA2 and IIB1 groups in respect of radiological and clinical will be researched. More biomechanical study of the rotational and axial stability of the implant would also be designed in the further. In the previous studies, various intramedullary implants including Hagie pins, Kirschner wires and ESIN were applied for medial clavicle but with many complications. In order to overcome these problems, this new TEN was designed in this study. However, there are also many other implants need to be researched. Comparative study of more implants would also be showed.
Conclusion
Intramedullary fixation with our self-designed TEN might be a safe and effective treatment for displaced midshaft clavicular fractures with few complications and satisfactory clinical therapeutic effects.
Acknowledgement
This study was supported by the leader of Shanghai Pudong New Area health system training plan (No. PWRd2012-12), Shanghai municipal bureau of health research topic (No. 20124311) and Shanghai Pudong New Area of science and technology commission project (No. PKJ2012-Y25).
References
- 1 F. Postacchini, S. Gumina, P. De Santis, F. Albo; Epidemiology of clavicle fractures; J Shoulder Elb Surg, 11 (2002), pp. 452–456
- 2 C.M. Robinson; Fractures of the clavicle in the adult epidemiology and classification; J Bone Jt Surg Br Vol, 80 (1998), pp. 476–484
- 3 C.R. Rowe; 4 an atlas of anatomy and treatment of midclavicular fractures; Clin Orthop Relat Res, 58 (1968), pp. 29–42
- 4 K.J. Jeray; Acute midshaft clavicular fracture; J Am Acad Orthop Surg, 15 (2007), pp. 239–248
- 5 A. Eskola, S. Vainionpää, P. Myllynen, H. Pätiälä, P. Rokkanen; Outcome of clavicular fracture in 89 patients; Arch Orthop Trauma Surg, 105 (1986), pp. 337–338
- 6 D. Stanley, S. Norris; Recovery following fractures of the clavicle treated conservatively; Injury, 19 (1988), pp. 162–164
- 7 J.M. Hill, M.H. McGuire, L.A. Crosby; Closed treatment of displaced middle-third fractures of the clavicle gives poor results; J Bone Jt Surg Br Vol, 79 (1997), pp. 537–538
- 8 P.J. Denard, K.J. Koval, R.V. Cantu, J.N. Weinstein; Management of midshaft clavicle fractures in adults; Am J Orthop (Belle Mead, NJ), 34 (2005), pp. 527–536
- 9 O. Verborgt, K. Pittoors, F. Van Glabbeek, G. Declercq, R. Nuyts, J. Somville; Plate fixation of middle-third fractures of the clavicle in the semi-professional athlete; Acta Orthop Belg, 71 (2005), pp. 17–21
- 10 F.-J. Wijdicks, M. Houwert, M. Dijkgraaf, et al.; Complications after plate fixation and elastic stable intramedullary nailing of dislocated midshaft clavicle fractures: a retrospective comparison; Int Orthop, 36 (2012), pp. 2139–2145
- 11 F.J. Wijdicks, R.M. Houwert, P.J. Millett, E.J. Verleisdonk, O.A. Van der Meijden; Systematic review of complications after intramedullary fixation for displaced midshaft clavicle fractures; Can J Surg, 56 (2013), pp. 58–64
- 12 R.M. Houwert, F.-J. Wijdicks, C.S. Bisschop, E.-J. Verleisdonk, M. Kruyt; Plate fixation versus intramedullary fixation for displaced mid-shaft clavicle fractures: a systematic review; Int Orthop, 36 (2012), pp. 579–585
- 13 J. Leppilahti, P. Jalovaara; Migration of Kirschner wires following fixation of the clavicle-a report of 2 cases; Acta Orthop, 70 (1999), pp. 517–519
- 14 E.J. Strauss, K.A. Egol, M.A. France, K.J. Koval, J.D. Zuckerman; Complications of intramedullary Hagie pin fixation for acute midshaft clavicle fractures; J Shoulder Elb Surg, 16 (2007), pp. 280–284
- 15 M.M. Kaiser, C. Stratmann, G. Zachert, et al.; Modification of elastic stable intramedullary nailing with a 3rd nail in a femoral spiral fracture model–results of biomechanical testing and a prospective clinical study; BMC Musculoskelet Disord, 15 (2014), p. 3
- 16 C.P. Dougherty, K.J. Gallen, D.K. Shuler; Clavicle Nail with Locking End Cap; (2013) [Google Patents]
- 17 P. Osateerakun, N. Limpaphayom; Elastic stable intramedullary nail: the viable technique for pediatric long bone fixation; Thai J Orthop Surg, 38 (2014), pp. 31–37
- 18 M. Kettler, M. Schieker, V. Braunstein, M. König, W. Mutschler; Flexible intramedullary nailing for stabilization of displaced midshaft clavicle fractures: technique and results in 87 patients; Acta Orthop, 78 (2007), pp. 424–429
- 19 A. Jubel, J. Andermahr, A. Prokop, J. Isenberg, K. Rehm; Minimal invasive biological osteosynthesis of the clavicle with a titanium nail; Kongressband/Deutsche Gesellschaft fur Chirurgie Deutsche Gesellschaft fur Chirurgie Kongress (2001)
- 21 A. Frigg, P. Rillmann, T. Perren, M. Gerber, C. Ryf; Intramedullary nailing of clavicular midshaft fractures with the titanium elastic nail problems and complications; Am J Sports Med, 37 (2009), pp. 352–359
- 22 M.C. Muller, C. Burger, A. Florczyk, N. Striepens, C. Rangger; Elastic titanium nails in minimally invasive osteosynthesis for mid-clavicular fractures; Chir Z alle Geb Oper Medizen, 78 (2007), pp. 349–355
- 23 E. Huskisson; Measurement of pain; The Lancet, 304 (1974), pp. 1127–1131
- 24 C. Ryf, A. Weymann; The neutral zero method—a principle of measuring joint function; Injury, 26 (1995), pp. 1–11
- 25 C. Constant, A. Murley; A clinical method of functional assessment of the shoulder; Clin Orthop Relat Res, 214 (1987), pp. 160–164
- 26 D.E. Beaton, J.N. Katz, A.H. Fossel, J.G. Wright, V. Tarasuk, C. Bombardier; Measuring the wole or the parts?: Validity, reliability, and responsiveness of the disabilities of the arm, shoulder and hand outcome measure in different regions of the upper extremity; J Hand Ther, 14 (2001), pp. 128–142
- 27 Y.-W. Tarng, S.-W. Yang, Y.-P. Fang, C.-J. Hsu; Surgical management of uncomplicated midshaft clavicle fractures: a comparison between titanium elastic nails and small reconstruction plates; J Shoulder Elb Surg, 21 (2012), pp. 732–740
- 28 Y.-F. Chen, H.-F. Wei, C. Zhang, et al.; Retrospective comparison of titanium elastic nail (TEN) and reconstruction plate repair of displaced midshaft clavicular fractures; J Shoulder Elb Surg, 21 (2012), pp. 495–501
- 29 A. Mahar, E. Sink, F. Faro, R. Oka, P.O. Newton; Differences in biomechanical stability of femur fracture fixation when using titanium nails of increasing diameter; J childrens Orthop, 1 (2007), pp. 211–215
- 30 A.P. Kadakia, R. Rambani, F. Qamar, S. McCoy, L. Koch, B. Venkateswaran; Titanium elastic stable intramedullary nailing of displaced midshaft clavicle fractures: a review of 38 cases; Int J shoulder Surg, 6 (2012), p. 82
- 31 C.C. Lu, P.C. Liu, S.H. Huang, C.H. Hsieh, Y.C. Tien, S.H. Chien; Complications and technical pitfalls of titanium elastic nail fixation for midclavicular fractures; Orthopedics, 37 (2014), pp. e377–e383
- 32 M.M. Kaiser, G. Zachert, R. Wendlandt, et al.; Increasing stability by pre-bending the nails in elastic stable intramedullary nailing: a biomechanical analysis of a synthetic femoral spiral fracture model; J Bone Jt Surg Br, 94 (2012), pp. 713–718
- 33 M. Windolf, M.F. Fischer, A.W. Popp, et al.; End caps prevent nail migration in elastic stable intramedullary nailing in paediatric femoral fractures: a biomechanical study using synthetic and cadaveric bones; Bone Jt J, 97-B (2015), pp. 558–563
- 34 A. Jubel, J. Andermahr, G. Schiffer, K. Tsironis, K.E. Rehm; Elastic stable intramedullary nailing of midclavicular fractures with a titanium nail; Clin Orthop Relat Res, 408 (2003), pp. 279–285
Document information
Published on 31/03/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?