Abstract
Background
Workplace violence (WPV) is becoming an issue that needs immediate attention in the United States, especially during this period as more states are adopting the “stand your ground laws to promote worker protection.” This study was conducted to investigate how WPV has contributed to an unsafe environment for nurses and nursing assistants who work in long-term medical care facilities.
Methods
A structure questionnaire was used to collect data for the study. Three facilities were sampled and 80 nurses and certified nursing assistants participated in the study. Ninety-two percent (n = 74) were female and 8% (n = 6) were male. Approximately 62% were black or African American, approximately 33% were Caucasians, and only 2% were from other ethnicities.
Results
We found that 65% of the participants had experienced WPV while 41% believed that management shows little or no concern for their safety. Approximately 23% of respondents believed that reporting supervisors WPV act is an unsafe action. In addition, 22% of those who reported that they have experienced WPV believed that the work environment is not safe to perform their duties. This significant difference in perception of workplace safety between those who had experienced WPV and those who had not was significant (t = 3.95, df = 158, p < 0.0001).
Conclusion
WPV is an epidemic problem that affects all health-care professionals. The findings of this study could help long-term medical care facilities' management identify the areas to focus on mitigating, controlling, and/or eliminating incidents of WPV.
Keywords
bullying ; long-term medical care facility ; safety ; terrorism
1. Introduction
Workplace violence (WPV) in the United States is becoming so alarming that many lives, jobs, and self-esteem are being affected. The menace has also taken a toll on workers' productivity to a drastic extent. According to the American Society for Industrial Security (ASIS) and the Society for Human Resource Management, WPV, in its many forms, presents one of the most challenging security and personnel safety problems that an organization can face [1] . Previous studies have revealed that WPV contributed to workers absenteeism, fear levels, morale reduction, increased health insurance premiums, and increased employee turnover [2] . WPV is a growing concern for employers and employees nationwide. Whereas employees face the physical and the emotional consequences, employers only face the monetary loss due to WPV. The 2011 ASIS Healthcare Security Council report [3] revealed that health-care workers are regularly subjected to minor, as well as, major verbal and physical abuses from patients, visitors, and staff members. In 2011, the Occupational Safety and Health Administration (OSHA) [4] reported that approximately two million Americans were victims of WPV each year, costing businesses up to US $120 billion annually. Every day, on average, two people are killed and 87 are injured as a result of a WPV incident [5] . WPV incidents account for 18% of all violent crimes in the United States [5] .
According to the Fidelity Brokerage Investment Services press report [6] , the health-care industry is among the top six industries in the United States notorious for WPV. In the health-care sector, WPV continues to gain acceptance, as it is widely perceived that nurses are expected to tolerate some degree of violence when performing their nursing duties. In 1998, Morrison [7] concluded in his study that whatever the case may be, the fact remains that health-care workers are unreasonably at risk of WPV. To reduce acts of WPV, many establishments have outlined procedures for investigating and resolving acts of WPV while making employment offers. One of the most common procedures includes employee assistance program, which allows employees who may have suffered WPV to seek help. However, due to the lack of trust in administrative ability to appropriately assess and handle WPV, nurses often fail to report incidents when they occur. It is common for employees to refrain from further educating themselves about their rights due to their fear of retaliation or loss of job. Many caregivers assume that WPV is a part of their job and fail to report such incidences, which prevents health-care facilities' management from developing and implementing further training to educate their employees on how to prevent or address violence. In 2004, McPhaul and Lipscomb [8] discussed the number of serious safety and health hazards health-care workers faced in their work environment including WPV. The OSHA policy on the work environment is that workers have a right to a safe workplace. OSHA also prohibits employers from retaliating against employees for exercising their rights under the law. In a forum discussion about WPV, McPhaul and Lipscomb [8] addressed the risk factors of WPV most presented in the health-care sector and the many approaches to prevent them.
Despite the involvement of governmental agencies, research recommendations, and OSHA policies on attempts to eliminate or reduce WPV, reports on WPV still showed that a significant result is yet to be achieved [5] , [7] and [8] . Assaults and violent acts were cited as the 10th leading cause of nonfatal occupational injury in the 2011 annual Workplace Safety Index [9] . These acts represent about 1% of all workplace injuries, which cost US $400 million in that fiscal year. In 2009, the Bureau of Labor Statistic reported “assaults and violent acts” as the third leading cause of fatal work injuries in 2008, constituting 16% of all fatal work injuries. The same report revealed that assaults against workers in state government occurred at a rate of 28.6 cases/10,000 full-time workers, which is much higher than the rates for local government (12.6) and private industry (2.4). In state government, the rate of assaults was especially high in the health-care and social assistance industry, with 122.3 cases/10,000 full-time employees. According to the U.S. Bureau of Labor Statistics, 2006, most of these assaults were injuries caused by health-care patients. A report by the Emergency Nursing Association [10] confirmed that the health-care industry leads all other sectors in the incidence of nonfatal workplace assaults.
In 2014, Kvas and Seljak [11] studied different nursing careers in Slovenia to determine which group of nurses is most frequently exposed to WPV. Their study result showed that 61% of nurses had been exposed to violence within the past year. Victims in the study responded to violence through a formal written method. According to the findings, most nurses did not report sexual violence because of the formal method used to report cases and because of their personal beliefs and fear of losing their job. Likewise, a report on WPV [12] documented that the consistency of reporting violence incidents and the format adopted for reporting them can greatly improve violence monitoring and prevention activities.
Nurses and certified nursing assistants (CNAs) are usually at the receiving end of most of these unlawful acts as their responsibilities center on the entire health-care system. Most workplace assaults within the health-care sector occur in nursing-related facilities and are committed by patients or residents of a health-care facility according to OSHA [13] . Nurses and CNAs are found working very closely with doctors, patients, families of the patients as well as their colleagues. Thus, they are subjected to deal with verbal or physical abuse from the patients. Precipitating factors for the risk of violence include status of the behavioral health patient, patients who are under the influence of drugs or alcohol, high patient volume, and prolonged wait time of the patient [14] . Apart from the violence that nurses' face with patients, Gacki-Smith et al [15] found that “the fundamental lack of respect between doctors and nurses is a huge problem that affects every aspect of their jobs” (p. 6). In 2010, The Emergency Nurse Association reported management activities that provide education and guidance to nurses on how to admit that WPV is a severe occupational risk that requires immediate attention from employers, law enforcement officers, and the community [10] .
1.1. Study significance
Although several studies have been conducted on WPV in the health-care industry, many of the authors have only based their findings on descriptive analysis. Perhaps, the strongest piece of evidence in support of the need for a situational analysis of violence in the health-care industry, especially long-term medical care facilities, is the demonstrated statistical relationship between violence toward nurses, CNAs, and the involvement of management. In this study, we hypothesized that WPV experienced by the nurses and CNAs' working in long-term medical care facilities will contribute to an unsafe environment while they are performing their duties.
1.2. Study objectives
This study addresses the following objectives:
- To assess the perspectives of nurses and CNAs in long-term medical care facilities on WPV.
- An analysis of caregivers' responses on WPV in long-term medical care facilities.
- Identification of common perpetrators of WPV and types of WPV practices in long-term medical care facilities.
2. Materials and methods
2.1. Study population and sample size
The study population consisted of nurses and CNAs working in long-term medical care facilities geographically located in the Piedmont Triad region of North Central Carolina. Our sample size included 80 registered male and female nurses and CNAs. Participants were recruited with the help of the participating facilities' management staff along with a support letter from the Institutional Review Board. Informed consent documents and experimental protocol approved by the authors' institution were signed before allowing participants to fill out the questionnaire. Participants were grouped into four age categories 18–25 years (Age Group 1), 26–35 years (Age Group 2), 36–45 years (Age Group 3), and 46 years and above (Age Group 4). Participants identified themselves as black or African American, Caucasians, and others. Access to all caregivers in the selected facilities was restricted because of lack of interest in WPV, fear of their supervisors, and lack of previous knowledge on WPV.
2.2. Procedure
Data were collected using a self-developed questionnaire adapted from a standardized questionnaire retrieved from an online material. The self-developed portions of the questionnaire were based on the interview responses with 10 nurses and five CNAs who worked in long-term medical care facilities for an average of 8 years. The questionnaire was reviewed by a group of certified occupational safety specialists and registered nurses to validate its content. The questions were presented in the form of yes/no options, which was similar to those used in previous studies [15] , [16] and [17] that investigated the effects of violence in the workplace. The study was approved by the Institutional Review Board. Prior to the distribution of the questionnaire to various facilities, each facility was visited to obtain permission for their participation in the study. At each facility, the purpose of the research was explained to each facilitys management and approval was obtained before the distribution date. In each facility, a securely sealed box with a slot only for depositing the completed questionnaire was made available at the reception desk for participants to return completed questionnaires without fear of personal identification by any member of the management (i.e., ensured that every participants privacy was protected). Each facility was visited three times daily (morning, afternoon, and evening) for 1 week. Participation was voluntary, and all surveys had a consent form attached that explained the purpose of the research. After a week, both completed and uncompleted questionnaires were collected from each facility for data compilation and analysis. Data were compiled and analyzed using MS Excel [18] version 2010 (Microsoft, Redmond, WA, USA). Analysis included both descriptive and inferential statistics.
3. Results
3.1. Data analysis
Eighty nurses and CNAs returned fully completed questionnaires of which 74 (92%) were female and six were male (8%). Sixty-two percent of participants were black or African American, approximately 33% were Caucasians, and only 2% were from other ethnicities. Approximately 58% of the participants indicated that their patients were predominantly Caucasians, and 28% of the participants listed their patients as black or African American, and Caucasians. Eleven percent of participants had patients who were only black or African Americans, whereas less than 1% of the participants had patients who were predominantly Hispanic or Latino, Asian/Pacific Islander (i.e., others). There were 11% in Age Group 1, 24% in Age Group 2, 25% in Age Group 3, and 40% in Age Group 4. Table 1 shows participants' ethnicity, age group, and sex by both ethnicity and age group distributions.
| Ethnicity | Age group (y) | ||||||
|---|---|---|---|---|---|---|---|
| Black | Caucasian | Other | 18–25 | 26–35 | 36–45 | ≥ 46 | |
| Population | 52 | 26 | 2 | 9 | 19 | 20 | 32 |
| Sex | |||||||
| Female | 48 | 24 | 2 | 9 | 18 | 20 | 27 |
| Male | 4 | 2 | 0 | 0 | 1 | 0 | 5 |
The analysis involved basic descriptive statistics concerning caregivers' perspectives on safety. Inferential statistical analysis was also performed on participants' exposure to WPV. When the respondents were asked about their experience relative to WPV, approximately 65% of the respondents reported to have experienced WPV in one form or the other, whereas only 35% reported that they had not experienced WPV.
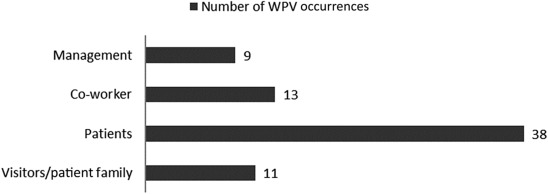
Further analysis was done on the questions relative to the management support/concern for the participants. Forty-one percent of the participants who reported WPV believed that management shows little or no concern for their safety. Analysis on whether the participants believe that reporting supervisors' WPV acts is a safe action was also conducted. The result revealed that 23% of the participants who had experienced WPV believed that the action is unsafe. Approximately 22% of those who reported having experienced WPV believed that the environment is not safe to perform their duties. On the question of whether participants report WPV when it occurred, approximately 33% of the participants responded “No.” About 88% of those who indicated that they did not report the incident failed to do so because of the fear of losing their jobs and the belief that the incident would not be handled appropriately. Only 12% said that they did not report the incident of WPV because of fear of retaliation. Fig. 1 shows the distribution of the sources of WPV as reported by the nurses and CNAs sampled.
|
|
|
Fig. 1. Frequency distributions of the sources of workplace violence (WPV) occurrences. |
Table 2 shows the sources of WPV rates in percentage as indicated by the participants. Approximately 54% of the violent acts were perpetrated by the patients, followed by co-workers (19%) and management (13%). Work context factors might be one major reason why co-workers were ranked second in WPV perpetrators. d'Ettorre and Greco [19] revealed that work context factors among health-care workers contributed a medium-level risk of work-related stress that could lead to violent acts.
| Sources | WPV (n ) | Rate (%) |
|---|---|---|
| Visitors/patient family | 11 | 15.5 |
| Patients | 38 | 53.5 |
| Co-worker | 13 | 18.3 |
| Management | 9 | 12.7 |
WPV, workplace violence.
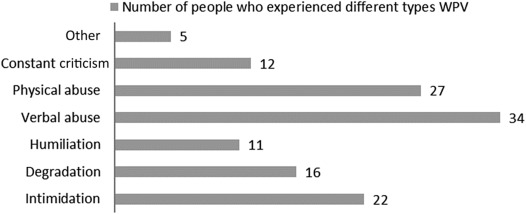
Forms of WPV experienced by participants were also analyzed. Fig. 2 illustrates the frequency distribution of types of WPV that participants have experienced. It can be seen from Fig. 2 that verbal abuse is the major type of WPV in long-term medical care facilities, followed by physical abuse and intimidation. Intimidation can easily affect human beings psychologically, and thus lead to performance degradation.
|
|
|
Fig. 2. Frequency distributions of different types of workplace violence (WPV) perpetuated in long-term medical care facility. |
Table 3 shows the frequency distributions of WPV types noticed in long-term medical care facilities and the rates at which each violent act was perpetrated as reported by the surveyed participants. The rate of verbal abuse was 27%, whereas that of physical abuse was about 22%. The rates of intimidation and degradation were 18% and 13%.
| WPV type | WPV type (n ) | Rate (%) |
|---|---|---|
| Intimidation | 22 | 17.32 |
| Degradation | 16 | 12.60 |
| Humiliation | 11 | 8.66 |
| Verbal abuse | 34 | 26.77 |
| Physical abuse | 27 | 21.26 |
| Constant criticism | 12 | 9.45 |
| Other | 5 | 3.94 |
WPV, workplace violence.
An inferential analysis test using Statistical Analysis Software (SAS Institute Inc., Cary, NC, USA) was conducted with unpaired t test comparison on the number of participants who had experienced WPV in the last 3 years. The unpaired t test revealed a statistically significant difference in perceptions of workplace safety between those who had experienced WPV and those who had not (t = 3.95, df = 158, p < 0.0001). No statistically significant difference was found in the numbers of nurses and CNAs who know their legal right to prosecute perpetrators of WPV.
4. Discussion
We found that WPV remains high despite several studies that have been carried out on prevention programs. Findings revealed that management shows little or no concern about the safety of the caregivers as revealed from their attitudes toward the WPV report. This is verified by the findings of other studies [20] and [21] . The finding in this study, which showed that patients were the common perpetrators of WPV followed by co-workers, agrees with other studies in this area [14] and [22] . The need for tailored interventions will be helpful to ensure that co-workers' violent acts at the workplaces are totally eliminated. Our results are also consistent with the findings of the councils study in 2011 [3] that health-care workers are regularly subjected to minor as well as major verbal and physical abuse from patients, visitors, and other staff, and corroborate those of previous investigations that have identified verbal abuse as the most common violence found among the caregivers [4] , [15] and [23] .
Our findings also reveal that 88% of the sampled participants failed to report WPV because of the fear of losing their job and the inappropriate way management will handle the situation, which agrees well with the report of the Emergency Nurses Association [10] . Another important finding was the fear of retaliation reported by the nurses and CNAs. We believe that workers safety training should be developed and disseminated with consideration of various levels to ensure training efficiency. WPV could be reduced if workers are given proper training on how to handle situations.
Employers should be required to establish a WPV prevention program or incorporate the information into an existing accident prevention program, employee handbook, or manual of standard operating procedures. In addition, OSHA should ensure that all employer and employees understand that all claims of WPV will be investigated and remedied promptly.
4.1. Limitations
This study had the following limitations: (1) Participants were from only three facilities operating in the Southeast United States. (2) Only registered nurses and CNAs were included in the study. (3) Lack of WPV awareness among caregivers in long-term medical care facilities and fear of loss of their jobs reduced the number of people who participated in the study.
4.2. Future research recommendations
- Research should be expanded to include a broader range of long-term medical care facility settings beyond North Carolina. There is also a need to examine how risk factors may vary across facilities and examine the effectiveness of violence intervention program.
- Because long-term medical care facilities were used, emphasis on employee conflict/bullying with patients was not adequate. It is recommended that employee bullying should be considered a priority in WPV research.
- Future research should pay more attention on how absenteeism of nurses may contribute to WPV on other nurses.
Many studies have concluded that the health-care industry is one of the major areas needing immediate intervention to prevent WPV. In 2010, Child et al [24] concluded in their study that more research needs to be conducted to synthesize widely agreed upon effects of WPV on caregivers. This study investigated nurses' perceptions on how WPV has contributed to an unsafe work environment in long-term medical care facilities. WPV is still at a high rate and the work environment is hostile. Facilities' management support for nurses and CNAs is not encouraging. WPV prevention and intervention processes should be adopted to help prevent threatening behavior and violence affecting the workplace. These processes should also outline procedures for detecting, investigating, managing, and addressing threatening behavior or violent episodes that occur in the workplace. Future studies should examine how risk factors vary across facilities and address the effectiveness of violence intervention programs.
Conflicts of interest
All contributing authors declared no conflicts of interest.
Acknowledgments
The authors acknowledge the effort of the students who helped during the development of the questionnaire. Authors also declare that the research was not funded by any agency or organization.
References
- [1] American Society for Industrial Security and the Society for Human Resource Management. Development of workplace violence prevention and intervention national standard [Internet]. 2009 Mar 9 [cited 2014 Dec 28]. Available from: http://security-today.com/articles/2009/03/09/asis-workplace-violence.aspx .
- [2] U.S. Department of Labor, Bureau of Labor Statistics. Survey of workplace violence prevention [Internet]. 2006 [cited 2014 Dec 26]. Available from: http://www.bls.gov/iif/oshwc/osch0033.pdf .
- [3] American Society for Industrial Security International Healthcare Security Council. Managing disruptive behavior and workplace violence in healthcare [Internet]. 2011 [cited 2014 Dec 28]. Available from: http://www.g4s.us/∼/media/Files/USA/PDF-Articles/Hospitals%20and%20Healthcare/Council_Healthcare_WorkplaceViolence.ashx .
- [4] U.S. Department of Labor, Occupational Safety and Health Administration. Workplace violence [Internet]. 2011 [cited 2015 Nov 23]. Available from: https://www.osha.gov/SLTC/workplaceviolence/ .
- [5] U.S. Department of Justice, Bureau of Justice Statistics. Violence in the workplace, 1993–1999: special report from the National Crime Victimization Survey [Internet]. Washington DC (WA): U.S. Department of Justice, Bureau of Justice Statistics; 2001 [cited 2014 Dec 26]. Available from: http://www.bjs.gov/content/pub/pdf/vw99.pdf .
- [6] Fidelity Brokerage Investment Services LLC. Market and sectors [Internet]. 2014 [cited 2015 Oct 1]. Available from: https://eresearch.fidelity.com/eresearch/markets_sectors/sectors/sectors_in_market.jhtml?tab=learn§or=35 .
- [7] E.F. Morrison; The culture of caregiving and aggression in psychiatric settings; Arch Psychiatr Nurs, 12 (1998), pp. 21–31
- [8] K.M. McPhaul, J.A. Lipscomb; Workplace violence in health care: recognized but not regulated; Online J Issues Nurs, 9 (2004), p. 7
- [9] Liberty Mutual. Liberty mutual workplace safety index: the direct costs and leading causes of workplace injuries [Internet]. Boston (MA): Liberty Mutual; 2004 [cited 2014 Dec 30]. Available from: http://www.libertymutual.com/ .
- [10] Emergency Nurses Association. Violence in the emergency care setting [Internet]. 2010 [cited 2015 Nov 23]. Available from: www.ena.org/SiteCollectionDocuments/Position%20Statements/Violence_in_the_Emergency_Care_Setting_-_ENA_PS.pdf .
- [11] A. Kvas, J. Seljak; Unreported workplace violence in nursing; Int Nurs Rev, 61 (2014), pp. 344–351
- [12] Whitmore B. Engaged leaderships role in workplace violence prevention [Internet]. 2012 [cited 2014 Dec 28]. Available from: http://www.huffingtonpost.com/bill-whitmore/workplace-violence_b_1278476.html .
- [13] Occupational Safety and Health Administration; Guidelines for preventing workplace violence for health care and social service workers; U.S. Department of Labor, Occupational Safety and Health Administration, Washington DC (WA) (1998) 3148 p
- [14] Restrepo T, Shuford H. Violence in the workplace. National Council on Compensation Insurance [Internet]. 2012 [cited 2014 Dec 26]. Available from: https://www.ncci.com/pages/default.aspx .
- [15] J. Gacki-Smith, A. Juarez, L. Boyett, C. Homeyer, L. Robinson, S. Maclean; Violence against nurses working in US emergency departments; J Nurses Admin, 39 (2009), pp. 340–349
- [16] T. Heponiemi, A. Kouvonen, M. Virtanen, J. Vänskä, M. Elovainio; The prospective effects of workplace violence on physicians' job satisfaction and turnover intentions: the buffering effect of job control; BMC Health Serv Res, 14 (2014), p. 19
- [17] D.M. Gates, C.S. Ross, L. McQueen; Violence against emergency department workers; J Emerg Med, 31 (2006), pp. 331–337
- [18] Microsoft Excel (computer program). Version 2010. Redmond (WA): Microsoft; 2010.
- [19] G. d'Ettorre, M. Greco; Healthcare work and organizational interventions to prevent work-related stress in Brindisi, Italy; Saf Health Work, 6 (2015), pp. 35–38
- [20] C. Kamchuchat, V. Chongsuvivatwong, S. Oncheunjit, T.W. Yip, R. Sangthong; Workplace violence directed at nursing staff at a general hospital in southern Thailand; J Occup Health, 50 (2008), pp. 201–207
- [21] H. Pai, S. Lee; Risk factors for workplace violence in clinical registered nurses in Taiwan; J Clin Nurs, 20 (2011), pp. 1405–1412
- [22] L.J. Samuel, C. Tudor, M. Weinstein, H. Moss, N. Glass; Employers' perceptions of intimate partner violence among a diverse workforce; Saf Health Work, 2 (2011), pp. 250–259
- [23] P.F. Levin, J.B. Hewitt, S.T. Misner, S. Reynolds; Assault of long-term care personnel; J Gerontol Nurs, 3 (2003), pp. 28–35
- [24] R.J. Child, J.C. Mentes; Violence against women: the phenomenon of workplace violence against nurses; Issues Ment Health Nurs, 31 (2010), pp. 89–95
Document information
Published on 07/10/16
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?