Summary
Background and aims
Total laparoscopic surgery is not a new concept, but it is not preferred generally for right colectomy. The aim of the study is to evaluate the outcomes, which are related with surgical technique after total laparoscopic right colectomy (TLRC) and laparoscopic-assisted right colectomy (LARC) for right colon cancer in 30 consecutive patients.
Materials and methods
Thirty patients with right colon cancer, half of which were treated with TLRC and half of which were treated with LARC, were compared with regard to patient demographics, operative and postoperative data, histopathologic findings, follow-up data, and the complications related to the surgical technique.
Results
There were 16 men and 14 women, median age was 63 years (range 41–86) with a body mass index (BMI) of 27 kg/m2 (range 20–33). There were no differences between the groups for BMI, harvested lymph node number, or distal and radial margins. The length of the incision and the length of the postoperative stay was shorter in the TLRC group (p = 0.000). Overall complications were higher in the LARC group than in the TLRC group (p = 0.014). The median follow-up was 28 months (range 5–99). In the late period, two patients in the LARC group were reoperated on. The cause of reoperation was internal herniation in one patient due to ileal twisting and incisional hernia in the other one.
Conclusion
Our preliminary data indicate that TLRC could result in better outcomes for right colon cancer patients than LARC.
Keywords
extracorporeal anastomosis;intracorporeal anastomosis;laparoscopic right colectomy;total laparoscopic colon resection
1. Introduction
Laparoscopic interventions have developed considerably in the last decade. Today, with the improvement of surgical skills and laparoscopic instruments, surgeons have begun to perform totally laparoscopic colorectal operations with the use of different techniques such as robotics or single port.1; 2 ; 3
In laparoscopic-assisted colectomy, the colon is mobilized with or without intracorporeal division of the vascular pedicle, the specimen is then extracted through a small incision and the anastomosis is performed extracorporeally.4; 5; 6; 7 ; 8 If the whole procedure, including dissection, vessel ligation, resection, and anastomosis, is performed intracorporeally, except for extracting the specimen through the incision, then it is totally laparoscopic. Total laparoscopic operations have been increasingly popular in the left colon and rectum; however, they are performed rarely in the right colon.9; 10 ; 11 Today, laparoscopic-assisted right colectomy (LARC) is still more preferred than the total laparoscopic one.4; 5; 6; 7; 8 ; 12 In the literature, there are few data comparing the outcomes of total laparoscopic right colectomy (TLRC) and LARC for colon cancer.10 ; 11 The aim of this retrospective study is to evaluate the preliminary results of the two different techniques, TLRC and LARC, for colon cancer.
2. Materials and methods
2.1. Study design
Thirty consecutive patients underwent TLRC or LARC for right colon cancer and were included to the study. Our methodology conformed to the principals outlined in the Declaration of Helsinki. The patients were fully informed about the operation and a detailed inform consent form reporting the operation details were signed by the patients. The decision for the type of anastomosis was made by the operating surgeons before laparoscopic exploration. Physical examination, blood biochemistry, colonoscopy, biopsy of the tumoral lesion, and computed tomography scan of the chest, abdomen, and pelvis were performed before surgery for each patient. The exclusion criteria for performing laparoscopic right colectomy were as follows: (a) tumor-related factors: no history of previous malignancy, tumors larger than 8 cm, tumors that were inoperable as a result of unresectable or multiple distant organ metastases, obstructing tumor and intestinal perforation, lesions of the transverse colon and lesions that require resection of the splenic flexure; or (b) patient-related factors: contraindications for laparoscopic surgery such as having a severe cardiopulmonary disease. Patients with a history of inflammatory bowel disease were excluded from the study.
Patient data were recorded and supplemented during the hospital stay and on follow-up visits after the surgery. Standard demographics, body mass index (BMI), length of the postoperative hospital stay, operative procedure, incision type and the length of incision, first defecation time after surgery, duration of surgery, blood loss during surgery, histopathologic evaluation of the resected specimens, and early (in the first 30 days after the surgery) and late (ones that occur after 30 days following the surgery) complications were evaluated retrospectively.
A clear fluid diet and oral 90 mL of oral sodium phosphate solution (Fleet soda, Kozmed Farmassotik Urunler Ltd. Sti, Ankara, Turkey) was given to the patients for mechanical bowel preparation the day before surgery. Intravenous antibiotic prophylaxis was performed with metronidazole at the time of anaesthesia induction. All patients went through one of these laparoscopic procedures: Group I, TLRC; Group II, LARC. All operations were performed by two surgeons (T.K. and I.H.) under general anesthesia.
2.2. Surgical procedure
After the induction of general anesthesia, the patient was positioned in the modified lithotomy with legs slightly separated from each other with the help of stirrups.
The surgeon and the camera assistant stood at the left side of the patient, whereas the second assistant stood between the legs of the patient. After preparation of the skin with povidone iodine, the insufflation of the abdomen with CO2 using a Veress needle (Veress Needle, Gyrus Acmi, inc., Stamford, CT, USA) through a left upper quadrant incision was established. The insufflator was set to a pressure of 12 mmHg.
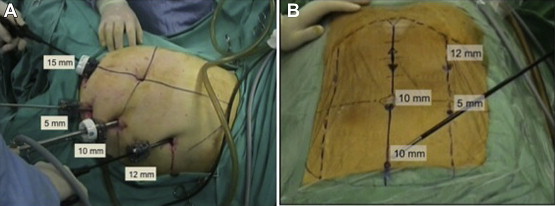
There were four trocars (one 5-mm, one 10-mm, one 12-mm, and one 15-mm) used for the TLRC (Fig. 1A). Among these, one of them was used for the camera, two of them were used for working, and the other one was used for retraction. All trocars were inserted under laparoscopic guidance, except for the first one. In LARC, the trocar sites were different from the total laparoscopic approach. Four trocars (one 5-mm, two 10-mm, and one 12-mm trocar) were used (Fig. 1B).
|
|
|
Figure 1. (A) The trocar sites of the total laparoscopic right colectomy procedure; (B) the trocar sites of the laparoscopic-assisted right colectomy procedure. |
After laparoscopic exploration, the patient was positioned to a 30-degree reverse Trendelenburg and 15-degree left lateral tilt position. Medial to lateral (vascular approach) technique was used in all operations. After the transverse colon was hung upward using an atravmatic grasper, the dissection was begun by using ultracision harmonic scalpel (Harmonic Scalpel Ace, Ethicon Endo-Surgery, Cincinnati, OH, USA) with the help of gentle traction of the right colon mesentery to lateral. Peritoneal incision was made below the ileocolic pedicle and close to the right border of the superior mesenteric vein. After the retroperitoneum was entered, the dissection was continued over Toldt fascia. The posterior sheath of the right mesocolon was dissected sharply through the anatomic avascular lines. The second part of the duodenum was exposed and sharply dissected from the mesocolon to ligate ileocolic vessels safely. The ileocolic vessels were clipped closely to the superior mesenteric vein with the help of endo clips (Hem-O-Lok, Weck Closure Systems, NC, USA). In our technique, we use endo clips instead of vascular cartridge. The reasons for this are: (1) they help perform a better high ligation and adequate regional lymph node dissection without leaving any remnant lymph node particle, and (2) help perform a safe ligation of the ileocolic pedicle by clipping the vessels alone without any other tissue entrapment. The next step was dissection of the head of the pancreas from the right mesocolon. Right colic vessels were clipped and divided by using endo clips and endo shears, respectively. The dissection of the right colon mesentery was carried out in a cephalad direction to find the middle colic vessels. When they were identified, the right branches of the middle colic vessels were dissected and clipped in cases of cecal and ascending colon tumors. Middle colic vessels were clipped and divided before they give out branches in cases of right flexure tumors. In those patients requiring ligation of the middle colic vessels, the left splenic flexure was mobilized for tension-free ileocolic anastomosis. The terminal ileum was also mobilized in all patients from the lateral and caudal peritoneal attachments for the same purpose.
The stomach was hung with an atraumatic grasper. The gastrocolic ligament was dissected with the omentum majus preserving gastroepiploic vessels along the greater curvature. With the guidance of Bursa omental anatomic space, the right flexure was freed downwards. Because the medial dissection was completed, the right colon was fully mobilized after separating lateral peritoneal attachments.
2.3. Total laparoscopic resection and intracorporeal anastomosis
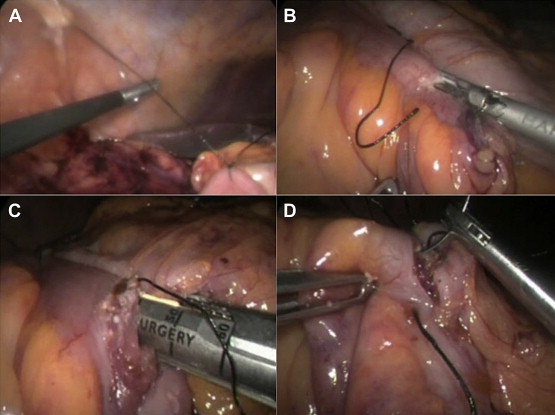
After vascular ligation, the transverse colon and the ileum (7 cm proximal to the ileocecal valve) were prepared for division. The terminal parts of the colon and the ileum were checked for viability. An endoscopic linear stapler (Echelon 60 ENDOPATH Ethicon Endo-Surgery, Cincinnati, OH, USA) inserted from the 12-mm left upper quadrant port was used for the division of the colon and the ileum. We use two or three cartridges for colon resection according to the diameter of the colon. The specimen was put into an Endobag (Endocatch II ENDO CATCH II 15 mm, Covidien, Dublin, Ireland) that was inserted through the 15-mm suprapubic port. The Endobag remained within the abdomen until the intracorporeal anastomosis was finished. The ileocolic anastomosis was performed in an isoperistaltic fashion. First, the ileum and the colon were sutured together with 2/0 silk stitches by using a needle-holder inserted via a 12-mm port. This stitch was used for the traction of the bowel segments laterally to do a safe anastomosis (Fig. 2A). The stitch was tied and cut in a distance of 5 cm. The traction was performed with the help of a suture-passer device that was inserted to grab the silk stitch from the right upper quadrant, percutaneously. Small full thickness incision was created with using Ultracision on both the colon and ileum for the insertion of endoscopic linear stapler jaws (Fig. 2B). The endoscopic linear stapler was inserted through the 12-mm left upper quadrant port to perform a side-to-side ileocolic anastomosis (Fig. 2C). The stapler was fired. The opening was closed by using continuous 2/0 polipropylene sutures with the help of the needle holder intracorporeally (Fig. 2D). The isoperistaltic anastomosis was finished with overlapping the ileum mesentery over the transverse mesocolon without closing the mesenteric defects. The suprapubic 15-mm port incision was widened to a 4–6-cm length to retrieve the resected specimen.
|
|
|
Figure 2. The steps of creating intracorporeal ileocolic anastomosis. (A) Suspension of the ileum and the transverse colon to the abdominal wall before side-to-side anastomosis; (B) creation of the holes on the intestinal walls for insertion of the linear stapler jaws; (C) creation of the side-to-side ileocolic anastomosis; (D) closure of the holes with separate sutures. |
2.4. Laparoscopic-assisted resection and extracorporeal anastomosis
The vascular dissection and the ligation steps were the same as the ones performed in the total laparoscopic resection approach. After vascular division, the supraumbilical incision was vertically widened. The wound protector (Alexis, Applied Medical, Rancho Santa Margarita, CA, USA) was inserted. The transverse colon and the ileum were retrieved. Functional end-to-end anastomosis was performed by using two linear staplers (75 mm Proximate, Ethicon Endo-Surgery, Cincinnati, OH, USA) with blue cartridge. After the anastomosis was placed into the abdomen, the supraumbilical incision was closed. All trocars were removed after desufflation. Trocar sites larger than 5 mm were closed with fascia sutures. No drain was inserted. In LARC, the pneumoperitoneum was recreated. The opening between the ileum and the colon mesentery was closed by using continuous 2/0 silk sutures.
Histopathologic data including the number of lymph nodes harvested, longitudinal and radial margins of the specimen were recorded. The seventh edition of the American Joint Committee on Cancer (AJCC) cancer staging manual was used for staging of the tumors.
2.5. Statistical analyses
All data were expressed as median (range). Mann-Whitney U test and Chi-squared test (Fishers exact test) were used for the continuous and the categorical variables respectively. SPSS 12.0 (SPSS Inc., Chicago, IL, USA) was used for assessing the significance of the differences between groups. A p < 0.05 was considered as significant.
3. Results
Thirty patients were included in the study: of 15 in the LARC group and 15 in the TLRC group. There were 16 men and 14 women whose median age was 63 (range 41–86) years with a BMI of 27 kg/m2 (range 20–33).
There were no differences between the groups regarding the BMI, the first defecation time after surgery, operation time, or blood loss during surgery (Tables 1 and 2). The mean incision length and postoperative hospital stay of the patients in the TLRC group was significantly shorter than those in the LARC group (p < 0.001).
| LARC (n = 15) | TLRC (n = 15) | p value | |
|---|---|---|---|
| Sex (F/M) | 8/7 | 7/8 | 1.000 |
| Age (yr) | 63 (41–86) | 67.5 (47–80) | 0.383 |
| Body mass index (kg/m2) | 26 (20–31) | 27 (21–33) | 0.447 |
F = female; LARC = laparoscopic-assisted right colectomy; M = male; TLRC = total laparoscopic right colectomy.
| LARC (n = 15) | TLRC (n = 15) | p value | |
|---|---|---|---|
| Length of incision | 7 (6–8) | 5 (4–6) | <0.001 |
| Operation time (min) | 90 (70–150) | 100 (80–165) | 0.925 |
| Blood loss during surgery (ml) | 60 (50–100) | 60 (40–90) | 0.645 |
| First defecation time after surgery (d) | 4 (2–4) | 3 (2–4) | 0.108 |
| Postoperative hospital stay (d) | 8 (5–13) | 5 (4–7) | 0.000 |
LARC = laparoscopic-assisted right colectomy; TLRC = total laparoscopic right colectomy.
Histopathologic results, including harvested lymph nodes, surgical margins, and tumor stages, did not show any significant differences between two groups (Tables 3 and 4). The median follow-up time was 28 months (range 5–99).
| LARC (n = 15) | TLRC (n = 15) | p value | |
|---|---|---|---|
| Harvested lymph nodes | 23 (14–40) | 22 (16–48) | 0.581 |
| Proximal margin (cm) | 14 (7–30) | 14 (10–35) | 0.625 |
| Distal margin (cm) | 12 (10–30) | 16 (7–35) | 0.057 |
| Radial margin (mm) | 4 (1–12) | 4 (2–10) | 0.447 |
LARC = laparoscopic-assisted right colectomy; TLRC = total laparoscopic right colectomy.
| Stage | LARC (n = 15) | TLRC (n = 15) | p value |
|---|---|---|---|
| I | 5 | 4 | 1.000 |
| IIA | 4 | 5 | 1.000 |
| IIIB | 4 | 3 | 1.000 |
| IIIC | 2 | 3 | 1.000 |
LARC = laparoscopic-assisted right colectomy; TLRC = total laparoscopic right colectomy.
No operation was converted to open or no additional port was inserted to achieve better laparoscopic exploration in both groups. The complication rate for the LARC group (54%) was significantly higher than the TLRC group (7%; p = 0.014). This is shown in Table 5. In a patient with a BMI of 31 in the LARC group, twisting of the ileal mesentery was noticed after the anastomosis had been completed. The anastomosis was revised. There were three patients reoperated on for anastomotic leakage during the early postoperative period (7% in TLRC group vs. %13 in LARC group). All these patients were treated with terminal ileostomy and distal mucous fistula. In the late period two patients in the LARC group were operated on. One of these patients was operated on for acute abdomen. Operative findings revealed necrosis of an ileum segment due to an internal herniation through the mesentery. Resection of the necrotic bowel and ileo-ileal anastomosis were performed. The other patient was operated on for incisional hernia 3 months after initial surgery.
| LARC (n = 15) | TLRC (n = 15) | p value | |
|---|---|---|---|
| Intraoperative complications | |||
| Twisting of the mesentery | 1 (7%) | 0 (0%) | 1.000 |
| Postoperative complications | |||
| Early | |||
| Anastomotic leakage | 2 (13%) | 1 (7%) | 1.000 |
| Wound infection | 3 (20%) | 0 (0%) | 0.224 |
| Late | |||
| Incisional hernia | 1 (7%) | 0 (0%) | 1.000 |
| Internal herniation | 1 (7%) | 0 (0%) | 1.000 |
| Total complications | 8 (54%) | 1 (7%) | 0.014 |
LARC = laparoscopic-assisted right colectomy; TLRC = total laparoscopic right colectomy.
4. Discussion
After the first description of a laparoscopic colectomy for colon cancer by Jacobs in 1991,13 laparoscopic colorectal surgery has developed considerably. Laparoscopy offers less pain, rapid recovery, lower morbidity, shorter hospital stay, and better cosmesis with acceptable oncological results.8; 12; 14; 15; 16; 17; 18; 19; 20; 21 ; 22 Totally laparoscopic operations have gained wide popularity for left colon and rectal cancer operations. However, they have been rarely preferred by laparoscopic surgeons for patients with right colon cancer. Technical difficulty, equipment cost, and longer operation time could be limitations of TLRC.9; 10 ; 11 TLRC has been performed to overcome the detrimental effects of laparoscopic assisted technique such as unnoticed mesenteric rotation and increased tension of the mesentery while extracting the colon and ileum to perform anastomosis. Creating the anastomosis intracorporeally and retrieving the specimen through the suprapubic incision are the differences of TLRC than LARC.9; 10 ; 11
The main advantage of the laparoscopy is shortened skin incision. Reduced size of the surgical wound causes less pain, faster recovery period, less intraabdominal adhesion, and less incisional hernia occurrence. The technique and the experience of the surgeon could change the length of the incision in laparoscopic right colectomy. The skin incision of the TLRC patients is shorter than the LARC. The surgeons are eager to make middle abdominal incisions for specimen retrieval and perform extracorporeal anastomosis in LARC. However, the rate of incisional hernia can rise up to 24.3% after the midline incisions in laparoscopic-assisted colectomy.23; 24 ; 25 Transverse incisions in abdominal surgery are based on better anatomical and physiological principles.26 ; 27 Totally laparoscopic interventions provide a free specimen extraction site such as suprapubic incision or natural orifices. In TLRC, we perform Pfannensteil incision (suprapubic horizontal incision) for taking the resected specimen out of the abdominal cavity. We observed no incisional hernia in the TLRC group, but there was one patient operated on for incisional hernia in the LARC group. Pfannensteil incision offers less adhesions, less incisional hernia, and better cosmesis.28
The main goal of laparoscopic surgery in comparison with open surgery is to reduce tissue trauma. Laparoscopic surgery prevents excessive traction and manipulation of abdominal tissue. However, extracorporeal anastomosis may cause ischemia–reperfusion of the colon and ileum while evisceration through minilaparotomy incision for minimum 5–10 minutes.5 ; 6 During the entrapment in a very tight incision, inadvertent tearing of the mesentery of the bowel due to traction or torsion can occur.10 One of the patients in the LARC group was operated on with the diagnosis of internal herniation through the mesenteric defect. Ileal rotation could be related to inadequate exposition during the completion of extracorporeal anastomosis in the LARC group.
In our series, total complication rate of the TLRC group is significantly lower than the LARC group. Recent studies also suggest that creation of intracorporeal anastomosis in laparoscopic right colectomy could be performed safely with improved postoperative patient comfort keeping radical oncological standards.29 ; 30 In various studies, the rate of complications rise to 18% with a wound infection rate of 7%, an anastomotic leakage rate of 3.5% and a surgical reintervention rate of 4.2% in LARC.8; 10 ; 15 Somehow, our overall complication rate and anastomotic leakage rate is slightly higher than the laparoscopic right colectomy series.5 ; 6 But, the results are not similar and varying among the laparoscopic colon surgery series. Park et al31 had reported that anastomotic leakage rate could range between 6–9% for the first 200 cases of laparoscopic colon surgery. High postoperative morbidity could be the factor causing prolonged postoperative hospital stay in patients underwent LARC. Histopathologic results after TLRC and LARC were similar in the study.
This study is a small case series comparing TLRC and LARC; we can only recommend our preliminary experience regarding two different techniques. TLRC is a technically superior intervention to LARC. Our preliminary data indicate that performing TLRC could improve postoperative outcomes. New prospective randomized studies including sufficient patient numbers will be able to prove the advantages and disadvantages of these two techniques clearly.
Acknowledgments
The authors have no conflicts of interest to declare. No funding source was used for the study. The authors thank Arif Sami Kahya, MD, for the figures and Sibel Akbay for the editing of the article.
References
- 1 R.A. Cahill, I. Lindsey, O. Jones, et al.; Single-port laparoscopic total colectomy for medically uncontrolled colitis; Dis Colon Rectum, 53 (2010), pp. 1143–1147
- 2 A. Zimmern, L. Prasad, A. Desouza, et al.; Robotic colon and rectal surgery: a series of 131 cases; World J Surg, 34 (2010), pp. 1954–1958
- 3 J.H. Lefevre, F. Bretagnol, M. Ouaïssi, et al.; Total laparoscopic ileal pouch-anal anastomosis: prospective series of 82 patients; Surg Endosc, 23 (2009), pp. 166–173
- 4 I. Baca, Z. Perko, I. Bokan, et al.; Technique and survival after laparoscopic assisted right hemicolectomy; Surg Endosc, 19 (2005), pp. 650–655
- 5 A.J. Senagore, C.P. Delaney, K.M. Brady, et al.; Standardized approach to laparoscopic right colectomy outcomes in 70 consecutive cases; J Am Coll Surg, 199 (2004), pp. 675–679
- 6 W.S. Tan, M.H. Chew, B.S. Ooi, et al.; Laparoscopic versus open right hemicolectomy: a comparison of short-term outcomes; Int J Colorectal Dis, 24 (2009), pp. 1333–1339
- 7 M.H. Zheng, B. Feng, A.G. Lu, et al.; Laparoscopic versus open right hemicolectomy with curative intent for colon carcinoma; World J Gastroenterol, 11 (2005), pp. 323–326
- 8 C.P. Delaney, R.P. Kiran, A.J. Senagore, et al.; Case-matched comparison of clinical and financial outcome after laparoscopic or open colorectal surgery; Ann Surg, 238 (2003), pp. 67–72
- 9 I. Raftopoulos, A.P. Courcoulas, D. Blumberg; Should completely intracorporeal anastomosis be considered in obese patients who undergo laparoscopic colectomy for benign or malignant disease of the colon; Surgery, 140 (2006), pp. 675–683
- 10 M. Hellan, A. Casandra, A. Pigazzi; Extracorporeal versus intracorporeal anastomosis for laparoscopic right colectomy; JSLS, 13 (2009), pp. 312–317
- 11 R. Bergamaschi, E. Schochet, C. Haughn, et al.; Standardized laparoscopic intracorporeal right colectomy for cancer: short-term outcome in 111 unselected patients; Dis Colon Rectum, 51 (2008), pp. 1350–1355
- 12 E. Lezoche, F. Feliciotti, A.M. Paganini, et al.; Laparoscopic vs open hemicolectomy for colon cancer; Surg Endosc, 16 (2002), pp. 596–602
- 13 M. Jacobs, J.C. Verdeja, H.D. Goldstein; Minimally invasive colon resection; Surg Laparosc Endosc, 1 (1991), pp. 144–150
- 14 H.J. Bonjer, W.C. Hop, H. Nelson, et al.; Transatlantic laparoscopic assisted vs. open colectomy trials study group. Laparoscopic assisted vs open colectomy for colon cancer: a meta analysis; Arch Surg, 142 (2007), pp. 298–303
- 15 A.M. Lacy, J.C. Garcia-Valdecasas, S. Delgado, et al.; Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomized trial; Lancet, 359 (2002), pp. 2224–2229
- 16 A.J. Senagore, C.P. Delaney; A critical analysis of laparoscopic colectomy at a single institution: lessons learned after 1000 cases; Am J Surg, 191 (2006), pp. 377–380
- 17 M.M. Reza, J.A. Blasco, E. Andradas, et al.; Systematic review of laparoscopic versus open surgery for colorectal cancer; Br J Surg, 93 (2006), pp. 921–928
- 18 Clinical Outcomes of Surgical Therapy Study Group; A comparison of laparoscopically assisted and open colectomy for colon cancer; N Engl J Med, 13 (2004), pp. 2050–2059
- 19 R. Veldkamp, E. Kuhry, W.C. Hop, The colon cancer laparoscopic or open resection study group (COLOR), et al.; Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomized trial; Lancet Oncol, 6 (2005), pp. 477–484
- 20 J. Fleshman, D.J. Sargent, E. Green, et al.; Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST study group trial; Ann Surg, 246 (2007), pp. 655–662
- 21 D.G. Jayne, P.J. Guillou, H. Thorpe, et al.; Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASSICC Trial Group; J Clin Oncol, 20 (2007), pp. 3061–3068
- 22 T.M. Khalili, P.R. Fleshner, J.R. Hiatt, et al.; Colorectal cancer, comparison of laparoscopic with open approach; Dis Colon Rectum, 41 (2008), pp. 832–838
- 23 E. Kuhry, W. Schwenk, R. Gaupset, et al.; Long-term outcome of laparoscopic surgery for colorectal cancer: a cochrane systematic review of randomized controlled trials; Cancer Treat Rev., 34 (2008), pp. 498–504
- 24 U. Ihedioha, G. Mackay, E. Leung, et al.; Laparoscopic colorectal resection does not reduce incisional hernia rates when compared with open colorectal resection; Surg Endosc, 22 (2008), pp. 689–692
- 25 E.R. Winslow, J.W. Fleshman, E.H. Birnbaum, et al.; Wound complications of laparoscopic vs open colectomy; Surg Endosc, 16 (2002), pp. 1420–1425
- 26 T.P. Grantcharov, J. Rosenberg; Vertical compared with transverse incisions in abdominal surgery; Eur J Surg, 167 (2001), pp. 260–267
- 27 J.A. Halm, H. Lip, P.I. Schmitz, et al.; Incisional hernia after upper abdominal surgery: a randomized controlled trial of midline versus transverse incision; Hernia, 13 (2009), pp. 275–280
- 28 K. Kisielinski, J. Conze, A.H. Murken, et al.; The Phannenstiel as so called ‘bikini cut’: still effective more than 100 years after the first description; Hernia, 8 (2004), pp. 177–181
- 29 M. Fabozzi, R. Allieta, R.B. Contul, et al.; Comparison of short- and medium-term results between laparoscopically assisted and totally laparoscopic right hemicolectomy: a case-control study; Surg Endosc, 24 (2010), pp. 2085–2091
- 30 M. Scatizzi, K.C. Kröning, A. Borrelli, et al.; Extracorporeal versus intracorporeal anastomosis after laparoscopic right colectomy for cancer: a case-control study; World J Surg, 34 (2010), pp. 2902–2908
- 31 I.J. Park, G.S. Choi, K.H. Lim, et al.; Multidimensional analysis of the learning curve for laparoscopic colorectal surgery: lessons from 1,000 cases of laparoscopic colorectal surgery; Surg Endosc, 23 (2009), pp. 839–846
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?