Abstract
Objective
The aim of this cadaveric study was to investigate the efficacy of the modified Stoppa approach in Ganz periacetabular osteotomy (PAO).
Methods
The Ganz PAO was performed on 10 hemipelvises with normal hips, from 5 cadavers using the modified Stoppa approach through the Pfannenstiel incision. All of the osteotomies were performed under fluoroscopic control and direct visualizing the osteotomy site from the same incision. After the osteotomy, the acetabulum was medialized and redirected anterolaterally, and fixed with 2 screws. The neurovascular structures and the joints were examined by dissecting the soft tissues after fixation of the osteotomies. Outcome parameters were center-edge (CE) angle, the distances between the osteotomy and anterior superior iliac spine (ASIS), and between the osteotomy and the sciatic notch, neurovascular and joint penetrations.
Results
After the osteotomy, the mean CE angle was improved from 19.8° to 25.2°, mean distance between the osteotomy and ASIS was 3.1 cm, and the mean distance between the osteotomy and the sciatic notch was 10.2 mm. The neurovascular structures and the joints were examined by dissecting the soft tissues after fixation of the osteotomies. No damage to the joint, surrounding arteries, veins or nerves was detected in any of the cadavers.
Conclusions
Bilateral dysplastic hips can be treated with a 10 cm, cosmetically more acceptable incision in the same session using this approach. Quadrilateral surface of the acetabulum can be directly seen using this approach and the osteotomy can be safely performed.
Keywords
Hip ; Periacetabular osteotomy ; Ganz osteotomy ; Modified Stoppa approach
Introduction
Periacetabular osteotomy is a restorative surgery for patients with hip dysplasia. There is consensus in the literature that untreated hip dysplasia progressively advances to arthritis.1 ; 2 Patients with acetabular dysplasia should be treated immediately after diagnosis rather than after symptoms appear or become more severe.3 ; 4 Surgical treatment attempts to convert the pathological shear force to a normal compressive force and prevent focal damage to the cartilage. As the weight-bearing area of the acetabulum decreases and the joint surface is lateralized, joint contact pressure increases, creating a condition which causes early osteoarthritis.2 ; 5 ; 6
Several osteotomies for the treatment of dysplastic hips have been described in the literature.1 ; 3 ; 4 ; 5 ; 7 ; 8 ; 9 ; 10 ; 11 ; 12 The Ganz periacetabular osteotomy (PAO) involves extensive exposure and careful cutting of the pelvic bones, as well as offers the advantages of a single incision, making higher amounts of corrections and pelvic continuity due to intact posterior colon.12 However, during this process, major complications may develop.1 ; 5 ; 13 ; 14 The most frequently encountered complication during the surgery is penetration of the osteotome into the joint; some authors have reported a 2.7% rate for this complication, which arises as a result of the inability to visualize the quadrilateral surface.15
There are reports in the literature documenting the use of different approaches that aim to reduce complications and decrease the duration of surgery and hospitalization, comparing the results with those of the standard approach.16 ; 17 ; 18 Some authors have focused on better visualization of the osteotomy site to achieve this aim.19 Similarly, it was hypothesized in the present study that Ganz PAO with modified Stoppa incision would be easier and safer than the standard approach. The modified Stoppa surgical approach was first described in 1993 by Cole et al for the treatment of acetabular anterior colon fractures.20 With this technique, the acetabular fracture is indirectly reduced, and fixation is possible. No previous studies have attempted to perform PAO using this approach.
PAO surgery involving a more minimally invasive method has positive effects on postoperative patient satisfaction. It was hypothesized in the present study that a medial colon osteotomy could be performed more easily using the modified Stoppa approach. The aim of this cadaveric study was to investigate the applicability of Ganz PAO surgery with the modified Stoppa surgical technique, the possible complications that may affect critical neurovascular structures, and the avoidance of penetration into the joint by osteotome or screw.
Materials and methods
This study was approved by the Board for Experimental Research in Forensic Medicine. PAO with modified Stoppa approach was performed on 10 hemipelvises of 5 fresh cadavers: 3 females and 2 male, aged 25, 31, 33, 37, and 40 years. Mean height of the cadavers was 172 cm (range: 160–178 cm), and mean weight was 84 kg (range: 56–98 kg). Hips with advanced osteoarthritis were not included in the study, and because there were no cadavers with dysplastic hips, the osteotomies were performed on hips with normal acetabulums.
The same surgical technique was performed for each cadaver by the senior author. The technique described by Cole et al was utilized to provide effective acetabular surgery.20 Before the osteotomy procedure, anteroposterior pelvic radiographs were obtained, and center-edge (CE) angles were measured.
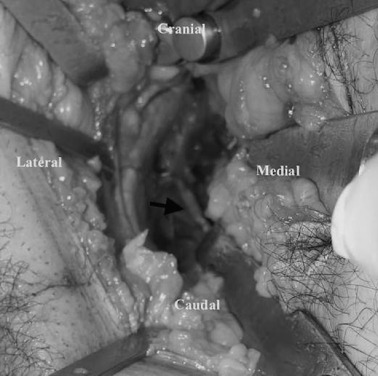
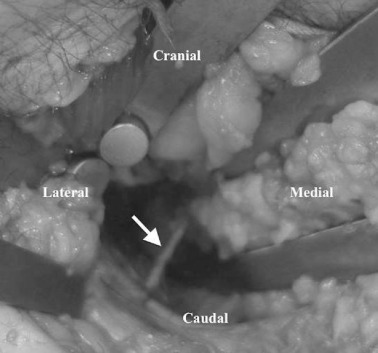
PAO was performed as originally described; however, the exposure involved a modified Stoppa incision. The cadavers were laid supine on a radiolucent operating table, and a 10-cm transverse incision was made 2 cm above the symphysis pubis (Fig. 1 ). The rectus sheath was carefully incised at the inferior border of the rectus abdominis muscle. After incision of the fascia transversalis, the abdominal muscles were bluntly dissected, and the peritoneum was retracted craniomedially with a blunt retractor. The psoas and iliac veins lying on the linea pectinealis were dissected bluntly and retracted carefully. The corona mortis was dissected carefully (Fig. 2 ). The periosteum was raised above the iliopectineal line, and a blunt retractor was inserted into the greater sciatic notch. At this stage, the obturator nerve was visualized in all cases and carefully preserved (Fig. 3 ).
|
|
|
Fig. 1. Incision. Pfannenstiel incision approximately 10 cm for modified Stoppa approach. |
|
|
|
Fig. 2. The corona mortis. Dissection and ligation of the corona mortis is important to prevent bleeding (black arrow) . It was dissected in all the cadavers to simulate real surgery. |
|
|
|
Fig. 3. The obturator nerve. The obturator nerve (white arrow) , which is prone to injury in modified Stoppa approach, was dissected and protected. |
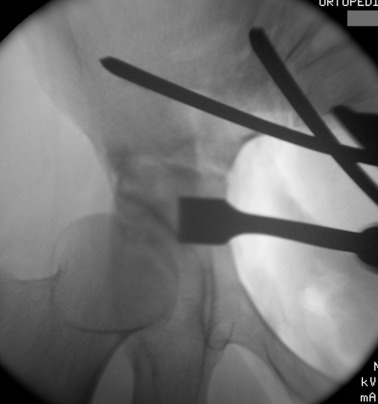
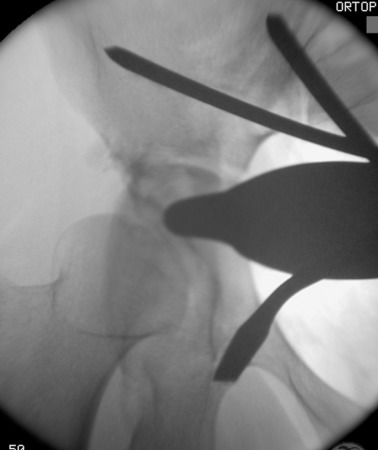
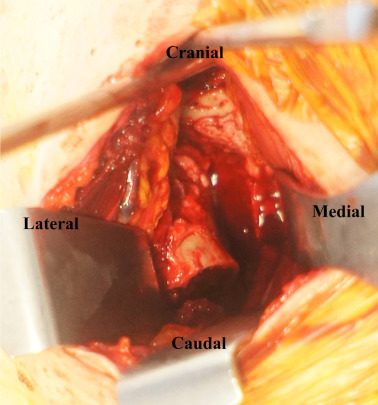
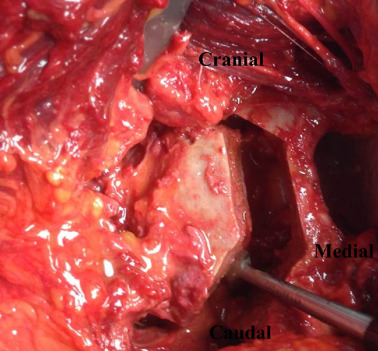
Prior to conducting the osteotomies, the greater sciatic notch, supraacetabular region, pubic rami, and quadrilateral surface were exposed, and the distances were measured as described by Shiramizu et al.15 The first osteotomy was performed on the supra-acetabular region and the iliac wing, from the pectineal line and aiming 1–2 cm distal to the medial of the anterior superior iliac spine (ASIS) (Fig. 4 ). The second osteotomy was performed on the posterior colon of the acetabulum, under fluoroscopic guidance with a 45° oblique view of the iliac. This osteotomy was from the pectineal line to the inferior ischium with an angle of 130° to the first osteotomy, leaving approximately 1 cm of bone posterior to the osteotomy line to preserve the posterior colon, as described in previously conducted anatomical studies (Fig. 5 ).15 The third osteotomy was performed on the pubic arm near to the acetabulum (Fig. 6 ; Fig. 7 ). And the last osteotomy was performed on the distal ischium, parallel to the inferior acetabular rim (Fig. 8 ). Each stage of the operation was conducted under fluoroscopic control to ensure that the osteotome did not penetrate the joint. By twisting the osteotome under fluoroscopic guidance, it was ensured that the fragment was completely free. After completing the osteotomies, the acetabular fragment was medialized and rotated anterolaterally using a spike-tipped pusher. An anterolateral repositioning of approximately 20° was achieved under fluoroscopy. After the correction, the osteotomy was fixed with 2 or 3 3.5-mm screws (DePuy Synthes, Bettlach, Switzerland), which were inserted percutaneously from the iliac crest to the supraacetabular area, using 0.5- to 1-cm skin incisions.
|
|
|
Fig. 4. The first osteotomy on the supra-acetabular region. From medial to lateral direction. |
|
|
|
Fig. 5. Posterior colon osteotomy. |
|
|
|
Fig. 6. Pubic rami osteotomy. |
|
|
|
Fig. 7. Pubic rami osteotomy was easily performed due to its close position to the incision. |
|
|
|
Fig. 8. Ischium osteotomy. |
The operation was considered successful if direct visualization and fluoroscopic examination confirmed that the osteotome and screws had not penetrated the joint. At this stage, the applicability of an intrapelvic plate was determined; however, because previous biomechanical studies showed that 2 screws were sufficient for ideal fixation, plate fixation was not performed.21
Following the osteotomy procedure, all hips were dissected and dislocated using the direct anterior approach and evaluated to determine whether chisel or screw penetrations had occurred to the joint and surrounding neurovascular structures (Fig. 9 ). Outcome parameters were pre- and postoperative CE angle, distance between the osteotomy and ASIS, and distance between the osteotomy and sciatic notch.
|
|
|
Fig. 9. Appearance of all the osteotomies, from the interior of the pelvis. |
Results
Mean CE angle improved from 19.8° (min: 18.6°; max: 22.1°) preoperatively to 25.2° (min: 24.1°; max 28.1°) postoperatively. Mean distance between the osteotomy and ASIS was 3.1 cm (min: 2.9 cm; max: 4.6 cm), and between the osteotomy and the sciatic notch was 10.2 mm (min: 9.7 mm; max 10.8 mm). Postoperative dissection confirmed that the sciatic nerve was not damaged by the osteotomy procedure. All osteotomies were performed while the pelvis was visualized through the same incision, facilitating preservation of the surrounding neurovascular structures such as the corona mortis and the obturator nerve. The corona mortis was identified as a vein in 4 cadavers and as an artery in 1 cadaver.
After Ganz osteotomy was completed and fixed in the cadavers, the neurovascular structures were examined via soft tissue dissection. No damage to the surrounding arteries, veins, or nerves was determined in any of the cadavers. A non-displaced fracture that extended from the osteotomy site to the middle of the iliac wing was noted in 1 specimen. The hips were carefully dislocated to examine the acetabulum, and no osteotome penetration to the acetabulum or screw malposition was found in any of the cadavers. Obesity presented a challenge when performing PAO via Stoppa incision in 2 cadavers.
Discussion
The purpose of this study was to evaluate the applicability of a safe and easy posterior colon osteotomy using a modified approach. Ganz PAO with a modified Stoppa incision was performed on 10 hemipelvises of 5 cadavers. Our experience with this approach suggests that location of the incision may be more cosmetically acceptable than with other approaches; furthermore, the modified Stoppa incision allows the application of bilateral PAOs in the same session in cases of bilateral dysplasia. The quadrilateral surface of the acetabulum can be better visualized with this approach, allowing the osteotomy to be safely performed. Our results demonstrate that this procedure provides good exposure with minimal dissection of the soft tissues and can be performed with decreased amount of X-ray exposure because of the direct visualization of the quadrilateral surface through the exposure. To the best of our knowledge, this is the first study of Ganz PAO procedure using modified Stoppa approach.
Ganz PAO is a widely accepted procedure for treating acetabular dysplasia.6 ; 12 ; 22 ; 23 ; 24 Several surgical approaches for Ganz PAO have been described; the most frequently used are the ilioinguinal and Smith-Petersen techniques.12 However, these approaches damage soft tissue, increase the complication rate, extend the patients hospital stay, and leave a significant and visible incision scar. Therefore, less-invasive approaches for PAOs are being investigated. The modified Stoppa incision, which provides more comfortable access to the pelvic brim and quadrilateral surface, has been previously introduced for acetabular fracture treatment.20 ; 25 ; 26 The area entered with the modified Stoppa approach is the anterior extraperitoneal-prevesical true intrapelvic space. When required, this incision can be extended toward the desired side, and the exposure can be increased.
There is a potential risk of intrapelvic vascular injury during Ganz PAO.27 A previous study reported excessive arterial bleeding requiring embolization in a patient with a prior acetabuloplasty.28 In a study by Kambe et al discussing the increased potential for vascular injury, the distance between the ramus pubis superior and the obturator artery was found to be 27.2–33.4 mm.29 With a modified Stoppa incision, the obturator artery, which is at high risk of injury during the classic Smith-Petersen procedure, can be protected by direct visualization.12 In the same study, the mean anterior inferior iliac spine-external iliac artery distance was found to be 31.7 mm in females and 38.2 mm in males. Despite its advantage of visualizing the obturator artery, the modified Stoppa incision does not allow for visualization of the external iliac artery.
Wall et al reported that during superior pubic ramus osteotomy, the obturator nerve and artery passes between 4 and 8 mm posteriorly.30 In exposures made with a Smith-Peterson incision, the obturator nerve is at risk along the course of the obturator foramen because the nerve passing immediately inferior cannot be relocated and may thus be damaged during pubic ramus osteotomy.12 With the technique applied in the present study, the full length of the obturator nerve could be visualized and protected.
Femoral nerve palsy may develop in some patients when dissection performed by Smith-Petersen incision enters between the rectus and the tensor fascia lata.12 ; 16 ; 26 Permanent dysesthesia associated with lateral femoral cutaneous nerve dysfunction severely reduces postoperative satisfaction of Ganz osteotomy patients.31 With a modified Stoppa incision, the femoral nerve and cutaneous branch are moved, resulting in less likelihood of this complication occurring postoperatively. In our study, the incision and exposure did not approach the femoral nerve trace.
Ganz et al described chisel penetration as the most severe complication of the procedure, occurring at a rate of 2.7%.12 The accepted reason for this complication is that the quadrilateral surface cannot be directly visualized, resulting in osteotomies in this region being performed blindly.15 In a study by Shiramizu et al that aimed to minimize complications, they attempted to prevent osteotome penetration by creating landmarks in the quadrilateral area.15 With the modified Stoppa technique, the acetabulum is approached from the medial aspect, and the quadrilateral surface can be completely visualized. During postoperative dissections, no chisel and wire penetration was detected in any cadavers in the present study.
Patients with symptomatic hip dysplasia are generally young adult females, a patient group in which cosmetic concerns are a priority.27 ; 32 Inan et al discussed this concern in a study of the application of endoscopy-assisted mini-incision PAO.27 In clinical studies, patients who have undergone Ganz PAO have been generally satisfied with the operations. From short- and mid-term results onward, most patients describe a reduction in pain and improved joint function.11 However, cosmetic changes and the short- and long-term effects on the patients psychology have not been discussed in these studies. PAO performed with modified Stoppa incision may be more acceptable postoperatively because a bikini can cover the incision scar, leading us to believe that cosmetic satisfaction of patients will be greater. The length of the modified Stoppa incision is similar to that of a Smith-Petersen incision, but the Stoppa incision is parallel to the skin creases; furthermore, healing is more physiologic, so the procedure may result in less scarring than a classic incision would.
The obturator vessels and nerve are the most important structures to attend to because of their direct contact with the quadrilateral surface. There was communication (corona mortis) between the obturator and the inferior epigastric veins in 40% of the 10 hemipelvises. With the modified Stoppa approach, the structure that requires the most care is a vascular structure, the corona mortis. In a cadaveric study by Kacira et al, the distances between the modified Stoppa approach and the vascular structures were described.33 This approach was recommended in appropriate cases to increase visibility of the quadrilateral surface and the posterior colon. The corona mortis is easily protected by this approach.
There were certain limitations to this study. Because a small number of cadavers were included in the study and the acetabular morphologies of the cadavers were normal, certain anatomic variations that may be observed in dysplastic hips that require live surgery could not be anticipated. Furthermore, objective outcome measures were limited, and the procedures were performed on a single ethnic group. As a result of the small number of the available cadavers, cadavers of various ages and both genders were used. The technique described in this report may be difficult to apply in obese patients and is more applicable for non-obese patients. A percutaneous Steinmann pin, similar to the anterior application of an external fixator, may be helpful for correction. In patients with acetabular dysplasia, treatment should involve radiological and clinical examinations of the intra-articular pathologies, preoperatively and using arthrotomy or arthroscopy intraoperatively. Another important limitation of the modified Stoppa approach for Ganz PAO is that an alternative approach is usually required for the treatment of intra-articular pathologies.
Conclusion
In light of the results of this cadaveric study, Ganz osteotomy using modified Stoppa technique for bilateral dysplastic hips without advanced deformities is an appropriate surgical approach that can be performed in a single session with a single incision. To confirm the smaller incision scar and the reduced heterotopic ossification resulting from the use of this technique, further clinical studies are needed to demonstrate the efficacy of the approach and the outcomes after surgery.
Conflict of interest
None declared.
References
- 1 D.R. Wenger, J.D. Bomar; Human hip dysplasia: evolution of current treatment concepts; J Orthop Sci, 8 (2003), pp. 264–271
- 2 S.B. Murphy, R. Ganz, M.E. Muller; The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome; J Bone Jt Surg Am, 77 (1995), pp. 985–989
- 3 S.L. Frick, S.S. Kim, D.R. Wenger; Pre- and postoperative three-dimensional computed tomography analysis of triple innominate osteotomy for hip dysplasia; J Pediatr Orthop, 20 (2000), pp. 116–123
- 4 F.D. Lalonde, S.L. Frick, D.R. Wenger; Surgical correction of residual hip dysplasia in two pediatric age-groups; J Bone Jt Surg Am, 84-A (2002), pp. 1148–1156
- 5 R. Ganz, M. Leunig; Osteotomy and the dysplastic hip: the Bernese experience; Orthopedics, 25 (2002), pp. 945–946
- 6 S.B. Murphy, M.B. Millis, J.E. Hall; Surgical correction of acetabular dysplasia in the adult. A Boston experience; Clin Orthop Relat Res (1999), pp. 38–44
- 7 Y. Hasegawa, T. Iwase, S. Kitamura, K. Yamauchi Ki, S. Sakano, H. Iwata; Eccentric rotational acetabular osteotomy for acetabular dysplasia: follow-up of one hundred and thirty-two hips for five to ten years; J Bone Jt Surg Am, 84-A (2002), pp. 404–410
- 8 T. Nakamura, M. Yamaura, S. Nakamitu, K. Suzuki; The displacement of the femoral head by rotational acetabular osteotomy. A radiographic study of 97 subluxated hips; Acta Orthop Scand, 63 (1992), pp. 33–36
- 9 R.B. Salter; Role of innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip in the older child; J Bone Jt Surg Am, 48 (1966), pp. 1413–1439
- 10 D.H. Sutherland, R. Greenfield; Double innominate osteotomy; J Bone Jt Surg Am, 59 (1977), pp. 1082–1091
- 11 J.C. Clohisy, A.L. Schutz, L. St John, P.L. Schoenecker, R.W. Wright; Periacetabular osteotomy: a systematic literature review; Clin Orthop Relat Res, 467 (2009), pp. 2041–2052
- 12 R. Ganz, K. Klaue, T.S. Vinh, J.W. Mast; A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results; Clin Orthop Relat Res (1988), pp. 26–36
- 13 J.G. Hussell, J.A. Rodriguez, R. Ganz; Technical complications of the Bernese periacetabular osteotomy; Clin Orthop Relat Res (1999), pp. 81–92
- 14 C.L. Peters, J.A. Erickson, J.L. Hines; Early results of the Bernese periacetabular osteotomy: the learning curve at an academic medical center; J Bone Jt Surg Am, 88 (2006), pp. 1920–1926
- 15 K. Shiramizu, M. Naito, I. Asayama, M. Yatsunami; A quantitative anatomic characterization of the quadrilateral surface for periacetabular osteotomy; Clin Orthop Relat Res (2004), pp. 157–161
- 16 J.G. Hussell, J.W. Mast, K.A. Mayo, D.W. Howie, R. Ganz; A comparison of different surgical approaches for the periacetabular osteotomy; Clin Orthop Relat Res (1999), pp. 64–72
- 17 A. Troelsen, B. Elmengaard, K. Soballe; A new minimally invasive transsartorial approach for periacetabular osteotomy; J Bone Jt Surg Am, 90 (2008), pp. 493–498
- 18 P. Bernstein, F. Thielemann, K.P. Gunther; A modification of periacetabular osteotomy using a two-incision approach; Open Orthop J, 1 (2007), pp. 13–18
- 19 J.Y. Ko, C.J. Wang, C.F. Lin, C.H. Shih; Periacetabular osteotomy through a modified ollier transtrochanteric approach for treatment of painful dysplastic hips; J Bone Jt Surg Am, 84-A (2002), pp. 1594–1604
- 20 J.D. Cole, B.R. Bolhofner; Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results; Clin Orthop Relat Res (1994), pp. 112–123
- 21 I. Mechlenburg, S. Kold, L. Rømer, K. Søballe; Safe fixation with two acetabular screws after Ganz periacetabular osteotomy; Acta Orthop, 78 (2007 Jun), pp. 344–349
- 22 J.C. Clohisy, S.E. Barrett, J.E. Gordon, E.D. Delgado, P.L. Schoenecker; Periacetabular osteotomy in the treatment of severe acetabular dysplasia; Surg Tech J Bone Jt Surg Am, 88 (suppl 1 Pt 1) (2006), pp. 65–83
- 23 C.A. Gillett; Bernese periacetabular osteotomy for hip dysplasia in young adults; AORN J, 75 (2002) 737–742, 744-737, 749-751; quiz 752, 754, 756-738
- 24 D.A. Katz, Y.J. Kim, M.B. Millis; Periacetabular osteotomy in patients with Downs syndrome; J Bone Jt Surg Br, 87 (2005), pp. 544–547
- 25 D.M. Jeffcoat, E.A. Carroll, F.G. Huber, et al.; Operative treatment of acetabular fractures in an older population through a limited ilioinguinal approach; J Orthop Trauma, 26 (2012), pp. 284–289
- 26 E. Hirvensalo, J. Lindahl, O. Bostman; A new approach to the internal fixation of unstable pelvic fractures; Clin Orthop Relat Res (1993), pp. 28–32
- 27 M. Inan, A. Gokce, F. Ustunkan; Endoscopy-assisted periacetabular osteotomy: a preliminary cadaveric study; Clin Orthop Relat Res, 466 (2008), pp. 862–870
- 28 D. Thawrani, D.J. Sucato, D.A. Podeszwa, A. DeLaRocha; Complications associated with the Bernese periacetabular osteotomy for hip dysplasia in adolescents; J Bone Jt Surg Am, 92 (2010), pp. 1707–1714
- 29 T. Kambe, M. Naito, I. Asayama, et al.; Vascular anatomy for rotational acetabular osteotomy: cadaveric study; J Orthop Sci, 8 (2003), pp. 323–328
- 30 E.J. Wall, R. Kolata, D.R. Roy, C.T. Mehlman, A.H. Crawford; Endoscopic pelvic osteotomy for the treatment of hip dysplasia; J Am Acad Orthop Surg, 9 (2001), pp. 150–156
- 31 R. Biedermann, L. Donnan, A. Gabriel, R. Wachter, M. Krismer, H. Behensky; Complications and patient satisfaction after periacetabular pelvic osteotomy; Int Orthop, 32 (2008), pp. 611–617
- 32 J. Parvizi, O. Bican, B. Bender, et al.; Arthroscopy for labral tears in patients with developmental dysplasia of the hip: a cautionary note; J Arthroplasty, 24 (2009), pp. 110–113
- 33 B.K. Kacra, M. Arazi, A.E. Cicekcibasi, M. Buyukmumcu, S. Demirci; Modified medial Stoppa approach for acetabular fractures: an anatomic study; J Trauma, 71 (2011), pp. 1340–1344
Document information
Published on 31/03/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?