Abstract
Objective: To synthesize contemporary evidence (2015–2025) comparing post-mastectomy breast reconstruction techniques—including prepectoral and subpectoral implants, as well as autologous flaps (DIEP, TRAM, latissimus dorsi)—focusing on patient-reported quality of life (QoL) and safety outcomes.
Methods: A systematic review was conducted following PRISMA 2020 guidelines. Searches were performed in PubMed/MEDLINE, Embase, CENTRAL, and Scopus for studies published between January 2015 and August 2025. Eligible designs included randomized controlled trials and comparative cohort studies. The primary outcome was QoL assessed with the BREAST-Q instrument. Secondary outcomes included complications (implant loss, capsular contracture), reoperations, and the impact of post-mastectomy radiotherapy (PMRT). Risk of bias was assessed using RoB-2 for RCTs and ROBINS-I for observational studies.
Results: Autologous reconstruction consistently achieved higher long-term BREAST-Q scores compared with implant-based techniques, despite longer recovery times. Prepectoral implant placement reduced animation deformity and capsular contracture relative to subpectoral reconstruction, with similar overall complication rates but increased rippling and seroma in selected cohorts. PMRT significantly increased the risks of implant loss and severe capsular contracture, favoring autologous approaches in patients requiring radiotherapy. BREAST-Q remains the gold standard PROM, with updated multilingual validations enhancing cross-cultural applicability.
Conclusions: Autologous flaps offer sustained QoL benefits in selected candidates. Prepectoral implant reconstruction, with or without acellular dermal matrix, is safe and effective, particularly in non-PMRT settings. Shared decision-making guided by BREAST-Q and aligned with NCCN/ESMO guidelines is essential.
Keywords (MeSH): Mastectomy; Mammaplasty; Breast Implants; Surgical Flaps (DIEP/TRAM); Quality of Life; Patient-Reported Outcome Measures; BREAST-Q; Radiotherapy; Adjuvant
Introduction
Breast reconstruction after mastectomy1 is an essential component of comprehensive breast cancer management,contributing significantly to improved body image and overall quality of life4 (QoL). Current guidelines from the National Comprehensive Cancer Network (NCCN) and the European Society for Medical Oncology (ESMO) recommend offering immediate or delayed reconstruction based on oncologic safety, patient comorbidities, planned adjuvant8 therapy, and patient preference. The BREAST-Q6 is the validated and widely used patient-reported5 outcome measure (PROM) specifically designed to assess satisfaction and QoL after breast reconstruction.
Methods
Data: this systematic review was conducted according to PRISMA 2020 guidelines and registered in PROSPERO (ID to be added).
Databases sources and search strategy: a comprehensive literature search was performed in PubMed/MEDLINE, Embase, Cochrane CENTRAL, and Scopus from January 2015 to August 2025. Gray literature was explored through Clinical Trials and relevant guideline documents from NCCN and ESMO were included. The core PubMed search strategy was as follows: (“Mastectomy”[MeSH]) AND (“Mammaplasty”[MeSH] OR “Breast Reconstruction”) AND (prepectoral OR subpectoral OR implant OR autologous OR DIEP OR TRAM OR “latissimus dorsi” OR “acellular dermal matrix” OR ADM) AND (“Quality of Life”[MeSH] OR BREAST-Q6 OR “patient-reported”) AND (2015:2025[pdat]).*
Eligibility criteria (PICOS):
- Population: Women ≥18 y after mastectomy1.
- Intervention: Prepectoral/subpectoral implants, autologous flaps.
- Comparators: Alternative reconstruction techniques, immediate versus delayed reconstruction, post-mastectomy radiotherapy7 (PMRT) versus no radiotherapy7.
- Outcomes: BREAST-Q6 domains, complications, reoperations, and healthcare costs.
- Design: Randomized controlled trials (RCTs) and comparative cohort studies.
Exclusions: Oncoplastic breast-conserving surgery, non-comparative case series.
- Design: Randomized controlled trials (RCTs) and comparative cohort studies.
Risk of bias: The ROBINS-I tool was used for observational studies, and RoB 2 for RCTs.
Data synthesis: Findings were summarized narratively. A meta-analysis was planned if ≥3 homogeneous studies were available. (Table 1)
Results (Evidence Synthesis)
Meta-analyses indicate that autologous breast reconstruction, such as DIEP and TRAM flaps, provides higher BREAST-Q scores in breast satisfaction and overall outcome at mid- and long-term follow-up, despite a longer initial recovery period [4,6]. These findings suggest that autologous reconstruction offers superior patient-reported outcomes compared to implant-based methods [4,6].
Prepectoral breast reconstruction avoids pectoralis muscle elevation, which reduces animation deformity and capsular contracture while maintaining complication rates comparable to subpectoral placement [3,7]. Nevertheless, some studies have reported an increased incidence of rippling and seroma formation associated with prepectoral implants [3,7].
Post-mastectomy radiotherapy (PMRT) has been shown to increase the risk of implant loss (OR ≈ 1.9) and severe capsular contracture (OR ≈ 8.9), particularly in direct-to-implant prepectoral reconstructions. These observations support the preference for autologous reconstruction when PMRT is anticipated [6].
The use of acellular dermal matrix (ADM) facilitates prepectoral implant placement without a significant increase in major early complications [8]. However, the risk of seroma and rippling varies depending on the product used, and its cost-effectiveness remains a topic of ongoing discussion [8].
Patient-reported outcomes measured using BREAST-Q modules, including versions 6.0 and 2.0, have been validated in multiple languages, ensuring cross-cultural comparability [5,9]. Version 2.0 is now recommended for assessing satisfaction and quality of life in patients undergoing breast reconstruction [5,9].
Finally, current guidelines from the NCCN (2025) and ESMO (2023) emphasize offering breast reconstruction through shared decision-making, integrating oncologic safety and the anticipated need for adjuvant therapy with patient preferences [1,2].
Discussion
This review highlights that the choice of surgical technique in breast reconstruction profoundly affects patient-reported quality of life [4,6]. Autologous reconstruction techniques, such as DIEP and TRAM flaps, consistently demonstrate superior long-term satisfaction in breast appearance and overall outcomes, as measured by BREAST-Q6 scores. However, these procedures require longer operative time, advanced microsurgical expertise, and extended recovery periods, which may limit their accessibility and patient preference [4,6].
Implant-based reconstruction, particularly prepectoral placement, offers advantages in reduced surgical morbidity and faster postoperative recovery [3,7]. Prepectoral implants also minimize animation deformity and capsular contracture compared to subpectoral placement. Nonetheless, implant-based approaches remain highly sensitive to the effects of post-mastectomy radiotherapy [7], which significantly increases the risk of implant loss and severe capsular contracture, particularly in direct-to-implant prepectoral reconstructions [6].
The introduction of acellular dermal matrix (ADM) has been transformative, facilitating prepectoral reconstruction while maintaining low rates of major early complications [8]. Despite these benefits, its high cost and variability in complication profiles necessitate careful patient selection and institutional experience [8].
Shared decision-making is critical in optimizing outcomes. Integrating oncologic safety, the need for adjuvant therapy, patient comorbidities, and psychosocial priorities ensures that reconstruction aligns with individual patient goals and quality of life [1,2]. The use of validated PROMs, such as BREAST-Q v2.0, is essential to capture patient perspectives and guide clinical decision-making across diverse populations [5,9].
Future research should focus on high-quality randomized controlled trials comparing autologous and implant-based reconstructions, as well as long-term PROMs collection, cost-effectiveness analyses, and evaluation of emerging techniques. Such studies will help refine guidelines and support evidence-based, patient-centered care in breast reconstruction.
Limitations
This systematic review has some limitations. The included studies vary in design, sample size, reconstruction techniques, and follow-up duration, which may influence outcome comparisons but also reflect real-world clinical diversity. Most evidence comes from observational cohorts rather than randomized controlled trials, introducing potential selection and reporting bias. Additionally, patient-specific factors such as comorbidities, body habitus, and psychosocial variables were inconsistently reported, limiting fully individualized recommendations. Long-term outcomes beyond five years remain scarce, and variations in BREAST-Q versions across studies may affect the consistency of patient-reported measures.
Conclusions
This systematic review synthesizes contemporary evidence on post-mastectomy breast reconstruction, emphasizing both clinical outcomes and patient-reported quality of life (QoL) as measured by the BREAST-Q. Autologous reconstruction, particularly DIEP and TRAM flaps, consistently provides superior long-term outcomes in breast satisfaction, psychosocial well-being, and overall QoL, despite longer operative times, the need for specialized surgical expertise, and extended recovery. These advantages are especially relevant for patients undergoing post-mastectomy radiotherapy (PMRT), where implant-based methods are more susceptible to complications such as capsular contracture and implant loss.
Prepectoral implant reconstruction, with or without acellular dermal matrix (ADM), has proven to be a safe and effective alternative for selected patients, especially those not receiving PMRT. Compared with subpectoral placement, it reduces animation deformity and capsular contracture while maintaining comparable safety profiles. Nonetheless, aesthetic concerns such as rippling and higher seroma risk, along with the high cost of ADM, remain considerations when selecting this approach.
These findings highlight the importance of individualized, patient-centered surgical planning. Decision-making should incorporate oncologic safety, anticipated adjuvant therapy, patient anatomy, and psychosocial preferences. The BREAST-Q 2.0 remains the gold-standard patient-reported outcome measure, with multilingual validation supporting its use in both clinical practice and research internationally.
Finally, clinical choices should align with established guidelines from NCCN and ESMO, emphasizing shared decision-making and the balance between reconstructive and oncologic priorities. Autologous reconstruction is preferred for patients requiring PMRT, while prepectoral implants offer a less invasive yet effective option for those without planned radiotherapy. Future research should focus on high-quality randomized trials, long-term PROMs, cost-effectiveness analyses, and emerging innovations to further personalize and optimize care for women after mastectomy.
Tables & Figures
| Domain | Eligibility Criteria |
| Population (P) | Women ≥18 years old who underwent mastectomy (any indication: oncologic or prophylactic). |
| Intervention (I) | Post-mastectomy breast reconstruction techniques: prepectoral implants, subpectoral implants, autologous flaps (DIEP, TRAM, latissimus dorsi), with or without acellular dermal matrix (ADM). |
| Comparator (C) | Alternative reconstruction techniques, immediate vs. delayed reconstruction, post-mastectomy radiotherapy (PMRT) vs. no PMRT. |
| Outcomes (O) | Primary: Quality of Life (QoL) assessed with BREAST-Q modules (satisfaction with breasts, psychosocial, sexual, and physical well-being). Secondary: complications (implant loss, capsular contracture, seroma, rippling), reoperations, healthcare costs. |
| Study design (S) | Randomized controlled trials (RCTs) and comparative cohort studies (prospective or retrospective). Excluded: oncoplastic breast-conserving surgery, non-comparative case series, case reports. |
Table 1. PICOS eligibility criteria
(Population, Intervention, Comparator, Outcomes, Study design).
| Author / Source | Year | Design | Key Findings |
| NCCN Guidelines for Patients: Invasive Breast Cancer | 2025 | Clinical guideline | Recommends immediate or delayed reconstruction based on oncologic safety, comorbidities, and patient preference. BREAST-Q suggested as the standard PROM. |
| Cardoso F, et al. (ESMO Guidelines) | 2023 | Clinical guideline | Emphasizes shared decision-making. Highlights the impact of adjuvant radiotherapy on reconstructive technique selection. |
| Fracon S, et al. | 2022 | Systematic review | Prepectoral vs. subpectoral: prepectoral reduces animation deformity and capsular contracture but may increase risk of rippling/seroma in some cases. |
| Potter S, et al. | 2019 | Systematic review | Autologous reconstructions show higher BREAST-Q scores at mid- and long-term follow-up compared with implants. Higher overall satisfaction despite longer recovery. |
| Zinzindohoue C, et al. | 2024 | Validation study | BREAST-Q validated in multiple languages, including version 2.0. Improves cross-cultural comparability of PROMs. |
| Navid M, Mads G, et al. | 2019 | Meta-analysis | Confirms superiority of autologous techniques over implants in patient-reported quality of life. |
| Yongxiao Wu, et al. | 2024 | Systematic review | Prepectoral vs. subpectoral: similar safety, lower capsular contracture with prepectoral, but higher risk of aesthetic complications. |
| Sevasti P, et al. | 2024 | Cohort study | ADM facilitates prepectoral reconstruction without increasing major complications. Cost-effectiveness remains debated. |
| Rita M, Goncalo T, et al. | 2022 | Validation study | BREAST-Q v2.0 validated. Established as the gold standard PROM in breast reconstruction. |
Table 2. Data extraction template. Author, year, design and key findings.
| Theme | Summary of Findings |
| Autologous vs. implants | Autologous reconstruction shows superior outcomes in BREAST-Q scores compared with implants, especially in long-term satisfaction and well-being. |
| Prepectoral vs. subpectoral | Prepectoral reconstruction reduces the risk of capsular contracture compared with subpectoral placement. |
| Impact of PMRT | Post-mastectomy radiotherapy (PMRT) is associated with higher rates of implant failure and complications. |
| Acellular dermal matrix (ADM) | ADM use enables safe prepectoral reconstruction but increases the risk of rippling. |
| Patient-reported outcomes (PROMs) | BREAST-Q remains the gold standard for assessing quality of life in breast reconstruction, validated in multiple languages and versions. |
Table 3. Narrative synthesis. Summary of findings.
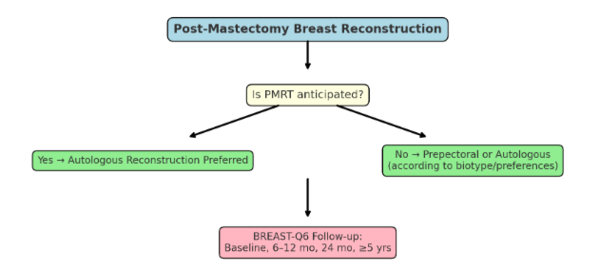
Figure 1. Clinical decision tree
- PMRT anticipated → autologous preferred.
- No PMRT → prepectoral or autologous depending on biotype/preferences.
- BREAST-Q6 at baseline, 6–12, 24 months, ≥5 years.
References
- 1. NCCN Guidelines for Patients: Invasive Breast Cancer. Version 3.2025. link
- 2. Cardoso F, et al. ESMO Clinical Practice Guidelines for Early Breast Cancer. Ann Oncol. 2023. doi:10.1016/j.annonc.2023.01.001
- 3. Fracon S, et al. Prepectoral vs subpectoral breast reconstruction: a systematic review. Aesthetic Plast Surg. 2022. doi:10.1007/s00266-022-02605-5
- 4. Potter S, et al. BREAST-Q patient-reported outcomes after autologous vs implant-based reconstruction: systematic review. J Plast Reconstr Aesthet Surg. 2019. doi:10.1016/j.bjps.2019.01.003
- 5. Zinzindohoue C, et al. BREAST-Q validation in multiple languages. Plast Reconstr Surg. 2024;153(4):987–998. doi:10.1097/PRS.0000000000001035
- 6. PubMed. Recent meta-analysis comparing autologous vs implant reconstruction outcomes. Available from: https://pubmed.ncbi.nlm.nih.gov/31711862/
- 7. PMC. Systematic review on prepectoral vs subpectoral implants. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC11385603/
- 8. BMC Cancer. Study on ADM outcomes. Available from: https://bmccancer.biomedcentral.com/articles/10.1186/s12885-024-13359-3
- 9. PubMed. BREAST-Q v2.0 validation and PROMs. Available from: https://pubmed.ncbi.nlm.nih.gov/35791701/
Document information
Published on 31/08/25
Submitted on 23/08/25
Licence: CC BY-NC-SA license
Share this document
Keywords
claim authorship
Are you one of the authors of this document?