Summary
Background
The reliability of X-ray radiography for diagnosing nasal bone fractures (NBFs) remains controversial. Recent studies show that, for determining the orientation and location of the displaced/depressed fracture, nasal sonography is as accurate as facial computed tomography. This retrospective study compared conductor-assisted nasal sonography (CANS) to conventional diagnostic tools and reported subjective patient satisfaction and discomfort after closed reduction combined with tube technique.
Methods
This retrospective study reports the results of 329 refinement treatments for nasal bone fracture (including 199 men and 130 women) performed from 2005 to 2011. All patients were assessed with CANS and completed a survey immediately prior to removing the packing. Questionnaires were adapted from the nasal obstruction symptom evaluation (NOSE) scale.
Results
The study found that CANS has a 97.2% rate of accuracy in diagnosing NBF. The visual analog scale scores of nasal obstruction, nasal congestion, sleep disturbance, trouble breathing, and inability to move air through the nose were analyzed. The experimental group scores were significantly different from the control group for all scores (p < 0.001).
Conclusion
Compared to conventional methods, CANS is more accurate for detecting NBF. We recommend its use as an alternative tool for diagnosing a nasal fracture. Because the tube technique balances pressure between the nasopharynx and middle ear during swallowing, patient comfort is enhanced. Application of these modifications can improve accuracy in diagnosing NBF and can improve the quality of NBF treatment.
Keywords
conductor-assisted nasal sonography;nasal bone fracture;tube technique
1. Introduction
The prominence of the nose on the human face makes it prone to injury.1 Blunt injuries sustained in traffic accidents, slip-and-fall accidents, batteries, and sports activities are the leading causes of nasal fractures. Properly treating nasal bone fracture (NBF) requires accurate diagnosis and evaluation. In addition to physical examination used to assess nasal deviation or depression, the tool most commonly used to detect NBFs is the radiograph. Although the radiograph is the initial step in assessing NBF, its reliability for diagnosing nasal fractures remains controversial.2 However, many studies have reported that X-ray examinations have poor sensitivity and specificity for diagnosing NBFs.3; 4 ; 5 Therefore, nasal sonography has garnered much interest in recent years because it provides detailed information about superficial areas in various imaging planes. Additionally, it does not require radiation exposure. Recent studies have concluded that, for delineating the orientation and location of the displaced/depressed fracture, nasal sonography is as accurate as facial computed tomography (CT).6; 7; 8; 9 ; 10 Since 2007, the authors have used conductor-assisted nasal sonography (CANS) as the primary tool for diagnosing NBF in the emergency department of a medical university hospital. By using an innovative probe conductor design and a water-filled glove, the CANS technique effectively avoids the discomfort of applying ultrasound gel on the face while providing images that are just as clear as CT images. Sonography is ideal for rapid and accurate diagnosis in preliminary assessment of a patient with suspected NBF.
Untreated NBFs can cause both cosmetic and functional complications. However, recommended management may vary from no intervention, to closed reduction, to extensive open reduction.11 Compared to open reduction, closed reduction is less invasive and procedurally simpler but achieves comparable outcomes. Thus, closed reduction of the nasal bone is the preferred treatment for most nasal trauma patients in the emergency department.
After closed reduction, the newly repositioned nasal bone and nasal septum can be fixed with intranasal packing. Various methods have been reported for packing and supporting the reduced nasal bone. A Doyle Combo Splint (DCS; Boston Medical Products Inc. Westborough, MA, USA) was commonly used in many medical facilities. It was combined with the airway tube and a Silastic sheet. Using the same concept, we inserted silicone catheters along the floor of the inferior nasal meatus prior to packing to minimize discomfort. This simple technique not only relieves nasal obstructive symptoms but also secures the position of the nasal septum, which otherwise tends to be easily displaced after reduction surgery.
This retrospective study compared CANS to conventional diagnostic tools and reported subjective patient satisfaction and discomfort after closed reduction combined with tube technique.
2. Materials and methods
This study enrolled 329 consecutive patients (199 male, 130 female) who were treated for NBFs at our plastic surgery department by two surgeons between January 1, 2005 and September 1, 2011. Fifty-five patients randomly selected as the control group who had nasal packing using Gelfoam® (Pfizer, NY, USA) and polyvinyl alcohol (PVA) sponge packing Invotec® (Invotec Inc, FL,USA) only. The remaining 274 patients (experimental group) had nasal packing with Gelfoam and PVA sponge packing with the tube technique. Age, sex, injury etiology, concurrent injuries, surgical time, and treatment technique were retrospectively identified and analyzed.
2.1. Diagnostic methods and application of CT and radiographs
Conventionally, diagnoses of nasal fractures require a detailed patient history and physical examination. Plain X-ray images were obtained first. However, CT examinations were performed when more severe facial bone injuries or intracranial lesions were suspected. In our hospital, facial CT scans are performed using 16-channel multidetector-row CT (Light-speed, General Electric Medical Systems, Milwaukee, WI, USA) at a slice thickness of 1–3 mm. Images are then viewed with a picture archiving and communications system. We classified all patients based on the nasal trauma classification proposed by Rohrich and Adams.12 Type I is simple and unilateral, Type II is simple and bilateral, Type III is comminuted, Type IV is complex (nasal and septal disruption), and Type V is associated with nasoorbitoethmoid fracture and midface fracture.
2.2. Conductor-assisted nasal sonography
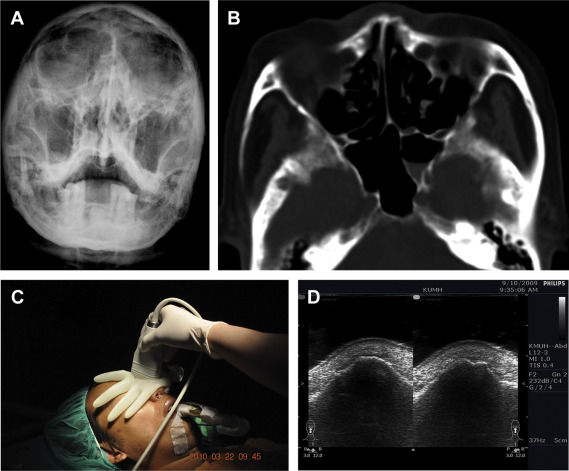
CANS was introduced in our emergency department in 2007. Since then, physicians have routinely used sonography to evaluate patients with acute nasal trauma except in cases of open wounds to the nose. During the study period, all CANS surveys were performed with a Philips Envisor HD ultrasound machine (Philips Medical Systems, Bothell, WA, USA) with a linear transducer (12 to 3 MHz; Fig. 1A–D). Transverse and longitudinal scans are both executed for the examiners panoramic evaluation. A water-filled surgical glove was used as a probe conductor to ensure full contact with the surface of the nose13 (Fig. 1C). In the study, any disruption, deviation, discontinuation of nasal cortical bone, or subcutaneous ectopic air noted over the scan site would be defined as nasal fractures. The examiner usually dichotomizes the survey result (fractured or nonfractured nose) with additional description of the injury site.
|
|
|
Figure 1. (A) Conventional Waters view showing negative findings and poor imaging quality for nasal bone. (B) Axial CT showing a depressed fracture in the left lateral aspect of the nose without dorsum fracture. However, the right lateral aspect of the nose fracture is not visible. (C) The results of conductor-assisted nasal sonography performed after closed reduction can be immediately assessed in the operating room. (D) Axial sonography showing depressed fracture indicated by identical discontinuity over both the left and right lateral aspects of the nose. The right side fracture (arrow) was unrecognized by CT scan. CT = computed tomography. |
2.3. Closed reduction and tube technique
In the emergency room, the risks, benefits, and nonsurgical alternatives were carefully explained to the patient. Additionally, the nose was reexamined to confirm the fracture diagnosis.
Generally, nasal pyramid fractures were reduced firstly. The Asch forceps was used to raise the nasal pyramid and to correct the malpositioned part of the septum. Insertion of Gelfoam below the nasal pyramid may provide extra support of these bone fragments. However, the repositioned septum is not completely stable and is easily displaced by nasal swelling, hematoma formation, or another accidental external force. The septum should be inspected and carefully rechecked for septal hematoma. Any septal hematoma should be drained directly.
Two segments of silicone tube with multiple side holes were inserted bilaterally into the inferior nasal meatus. The silicone tubes secured the septum along the inferior nasal meatus to avoid further septal distortion. Then, two PVA sponges were inserted medially and upward the nasal root to pack the common nasal meatus. The PVA sponges provided support to the nasal septum and nasal pyramid walls. This method not only stabilized the septum, but also minimized patient discomfort. It could balance the pressure between the nasopharynx and middle ear during swallowing. An external thermoplastic splint was used to maintain the reduced position for the 7 days (Fig. 2). Nasal packing was removed 3 days later. The patient underwent a 0–100 scale visual analog scale (VAS) questionnaire before removal of the nasal packing. All other procedures performed for the nose after the initial surgery was considered revision procedures.
|
|
|
Figure 2. (A, B) After closed reduction, a silicone catheter with multiple side holes was inserted into the inferior nasal meatus and the nasal septum was fixed by placing a polyvinyl alcohol sponge packing (INVOTEC) along the common nasal meatus. (C) Immediately after surgery, the septum was supported by suturing the catheter with the INVOTEC. An external splint was also applied. |
2.4. Discomfort caused by nasal obstruction
All patients completed a survey of nasal obstruction, nasal congestion, sleep disturbance, trouble breathing, and inability to move air through the nose immediately prior to removal of the packing. A questionnaire was adapted from the Nasal Obstruction Symptom Evaluation (NOSE)14 ; 15 scale, which is a disease-specific questionnaire for assessing the outcome of an intervention in nasal obstruction. A 0–4 scale is defined as 0 = not a problem, 1 = very mild problem, 2 = moderate problem, 3 = fairly bad problem, and 4 = severe problem. Each score is multiplied by 5 then added together. Total scores of 0 and 100 represent the results were assessed with VAS scores.
2.5. Statistical analysis
For statistical analysis, measured values are expressed as averages and standard deviations, SPSS, version 14.0 (SPSS Inc., Chicago, IL, USA) was used. Agreement between the experimental and control groups were measured with Fishers exact test and statistical significance threshold was set at 0.05. The descriptive statistical analysis includes accuracy, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) compared the clinical and intraoperative diagnosis and radiography findings with sonographic findings.
3. Results
3.1. Demographic data
The 329 patients enrolled in this retrospective study included 199 males and 130 females (age range, 7–80 years; mean age, 32.14 years). The highest incidence occurred in the group aged 20–29 years followed by the groups aged 30–39 years. The most common causes of injury were traffic accident (49.5%), battery (22.5%), sports injury (20%), and slip and fall (8%). The most frequent physical examination findings in the emergency department were tenderness (98%), nasal bleeding (69%), nasal deviation (63%), depression (58%), swelling (31%), and facial abrasion/laceration (18%).
Among these patients, 73% had NBFs only, 22% had concurrent nasal septal fractures, 18% had concurrent facial laceration, and 17% had concurrent facial bone fractures. In patients with concurrent facial bone fractures, the involved structures were the zygomaticomaxillary complex in 9.1%, the orbital floor in 5.7%, the mandible in 1.6%, the skull in 1.1%, and the frontal bone in 0.9%. Table 1 shows the demographic data for the 329 patients with NBF in this study. Furthermore, the most common type of nasal fracture was Type II, followed by Type III and Type I (Table 2).
| Mean (SD)/n (%) | |
|---|---|
| Age (y) | 32.14 |
| Male | 99 (66.5) |
| Female | 100 (33.5) |
| Trauma mechanism | |
| Traffic accident | 148 (49.5) |
| Battery | 67 (22.5) |
| Sports injury | 60 (20) |
| Slip and fall | 24 (8) |
| Clinical findings | |
| Tenderness | 293 (98) |
| Nasal bleeding | 206 (69) |
| Nasal deviation | 188 (63) |
| Depression | 173 (58) |
| Swelling | 93 (31) |
| Facial abrasion/laceration | 54 (18) |
| Associated fractures | |
| Nasal bone fracture alone | 248 (83) |
| Concurrent nasal septal fracture | 66 (22) |
| Concurrent facial fracture | 50 (17) |
SD = standard deviation.
| Classification of injury | Number of patients | Total, n (%) | |
|---|---|---|---|
| Without nasal septal injury | With nasal septal injury | ||
| Type I | 67 | 0 | 67 (20.4) |
| Type II | 110 | 8 | 118 (35.9) |
| Type III | 71 | 14 | 85 (25.8) |
| Types IV and V | 9 | 50 | 59 (17.9) |
3.2. Conductor-assisted nasal sonography
The facial bone CT scans can provide the most accurate information for detecting NBF. For those patients who had received both CANS examination and facial CT scans, the agreement between CANS and CT was 0.926. CANS was more reliable than X-ray films in detecting nasal bone fracture. Compared with the CT scan, sonography showed 100% sensitivity and 90% specificity, 97% PPV, and 100% NPV. Compared with conventional radiographs, Lou et al13 reported that CANS was more accurate in detecting NBF (0.978). The diagnostic performance (sensitivity, specificity, PPV, NPV, and accuracy) of the comparison between CANS and CT scan is shown in Table 3.
| Sensitivity | Specificity | PPV | NPV | Accuracy | |
|---|---|---|---|---|---|
| Nasal sonography | 1 | 0.90 | 0.97 | 1 | 0.978 |
NPV = negative predictive value; PPV = positive predictive value.
3.3. VAS scores
The VAS scores of nasal obstruction, nasal congestion, sleep disturbance, trouble breathing, and inability to move air through the nose were 38.5 ± 12.7, 44.3 ± 13.2, 33.8 ± 13.7, 42.1 ± 13.2, and 35.9 ± 12.6, respectively, in the experimental group; the VAS scores were 73.6 ± 14.6, 63.8 ± 14.5, 63.9 ± 15.4, 68.6 ± 16.2, and 61.6 ± 12.5, respectively, in the control group. Neither the patients in the experimental group nor the control group had accidental packing removal. The experimental group had significantly different scores than the control group for all scores (p < 0.001). All patients underwent closed reduction of the nasal bone immediately followed by packing with/without tube technique. The details of the results are summarized in Table 4.
| Control group | Experimental group | p | |
|---|---|---|---|
| Case numbers | 55 | 274 | |
| VAS scores due to nasal packing | |||
| Nasal obstruction | 73.6 ± 14.6 | 38.5 ± 12.7 | <0.001 |
| Nasal congestion | 63.8 ± 14.5 | 44.3 ± 13.2 | <0.001 |
| Sleep disturbance | 63.9 ± 15.4 | 33.8 ± 13.7 | <0.001 |
| Trouble breathing | 68.6 ± 16.2 | 42.1 ± 13.2 | <0.001 |
| Inability to move air through nose | 61.6 ± 12.5 | 35.9 ± 12.6 | <0.001 |
| Dissatisfaction (%) | 9.1 | 5.8 | 0.367 |
| Revision rate (%) | 3.6 | 1.8 | 0.332 |
VAS = visual analog scale (0–100 scale in this study).
4. Discussion
The motorcycle is one of the most common forms of private transportation in Taiwan. The major causes of NBFs include not only battery and sports accidents, but also motorcycle accidents. In addition, the incidence of motorcycle-related traumatic injuries (69.6%) is higher than that of all other traffic injuries.16 Most patients were in the 20–29-year age group (36.7%) followed by the 30–39-year age group (21%). The number of male patients was almost double that of female patients. Finally, 49.5% of the NBFs injuries in this series were traffic accident-related.
Generally, diagnosis of NBF requires a detailed patient history and a thorough physical examination. A radiologic examination is often performed to check for bone fractures. For many years, X-rays were the most commonly used images for diagnosing NBF.17 However, studies in this field do not support the routine use of radiography to assist in diagnosing NBF. The effectiveness of routine radiography for surveying NBF has been questioned repeatedly in the literature. For example, Clayton and Lesser2 concluded that radiographs were useless for routinely assessing NBFs and for optimizing NBF treatment. Nigam et al18 reported that nasal radiographs are not routinely required for treating nasal trauma. Hong et al8 also reported that, because X-rays have limited accuracy for diagnosing NBF (82%), facial CT is preferable. In summary, because of the questionable effectiveness of plain X-ray images for diagnosing NBF, they should not be the sole basis of subsequent evaluation and management.
A literature review by Arden et al concluded that radiographs not only have low sensitivity and specificity in diagnosing nasal fractures, they also have limited predictive value when used for managing such injuries because of their high incidence of false-positive and -negative interpretations.19 Since 2007, our emergency department began to use CANS for diagnosing NBF. Although facial CT can provide structures details for diagnosing the nasal bone fracture, the high radiation exposure associated with CT remains a major concern. Also, axial CT images alone are not always sufficient for a definitive diagnosis. For example, CT may not clearly reveal a fine line indicating an NBF,20 ; 21 and a minor depression caused by an NBF is more easily diagnosed with the nasal lateral view obtained by X-ray than by CT scan.8 However, Hong et al8 reported achieving 100% accuracy in diagnosing NBF and recommended the use of sonography as the primary method of diagnosing nasal fracture in children. Mohammadi et al22 ; 23 reported that, for diagnosing NBF, sonography is superior to both X-ray and CT. Lee et al9 reported that sonography is superior to CT in terms of accuracy and reliability in evaluating nasal fractures. The clinical experience of the authors also indicates that sonography is more accurate than X-ray for detecting NBF.13
However, application of ultrasonic gel on the nose may irritate the patients. Therefore, a water-filled glove is used to conduct ultrasound waves and obtains comprehensive images with comparable resolution. The CANS provides a full view of the bilateral nasal wall and enables identification of fine fracture lines (Fig. 1D). The definition for an accurate diagnosis is that sonographic survey allows the examiner to illustrate every detail of the fracture, such as disclosure of all the existing fracture lines, precise estimation of the extent of fracture (its severity, displacement amount, orientation, etc).
The CT images can provide three-dimensional details and septum information. However, the cost and associated radiation exposure are the drawbacks. Under cost-effective consideration, we strongly recommend sonography as an alternative tool for diagnosing nasal fracture. The efficacy of CANS for detecting NBFs was confirmed by its high sensitivity and specificity. Table 59; 13; 21; 22 ; 23 compares sonography with other imaging methods for detecting NBF.
| Study | Study design | Examination tool | Sample size | Results |
|---|---|---|---|---|
| Thiede et al26 (2005) | Prospective | Conventional X-ray | 63 | Lateral nasal (US > XR) Nasal dorsum (XR > US) Nasal pyramid (US = XR) |
| Gurkov et al21 (2008) | Prospective | Conventional X-ray | 80 | Nasal dorsum, Se: 98%, Sp: 95% Lateral wall Se: 98%, Sp: 75% |
| Mohammadi et al22 (2009) | Cross-sectional double blind | Conventional X-ray | 171 | Se: 90%, Sp: 98%, PPV: 98%, NPV: 87% |
| Lee et al9 (2009) | Cross-sectional | Conventional X-ray, CT | 138 | Se: 100% Sp: 100% Ac: 100% |
| Lou et al13 (2012) | Retrospective | CT | 71 | Se: 100%, Sp: 89% PPV: 96%, NPV: 100% |
| Mohammadi et al23 (2011) | Retrospective | CT | 87 | Se: 97%, Sp: 91% Positive Likelihood Ratio: 11 Negative Likelihood Ratio: 0.0 |
Ac = accuracy; NPV = negative predictive value; PPV = positive predictive value; Se = sensitivity; Sp = specificity; US = ultrasonography; XR = X-ray.
To avoid interfering with the diagnosis and treatment process in acute settings, we performed an observational study during the study period. The nasal sonographic approach was termed as a supplemental examination in addition to conventional protocol. We did not intentionally execute nasal sonography in those who were apparently free of nasal injury, because the blinding for the examiner might be difficult to implement. Instead, the sonographic survey was routinely executed prior to facial CT scan.
We dichotomized the survey result into fractured or nonfractured nose with additional description of injury site (e.g., left lateral wall or nasal dorsum, etc.) We prefer to define CANS as a screening tool instead of a comprehensive examination because the nasal septal injury cannot be well visualized via this approach. According to our experience, if the CANS result is negative, even if soft-tissue swelling is still prominent, no further CT scan is needed.
The discomfort associated with nasal obstruction can cause multiple physiologic and psychological changes. Goode and Spooner24 first demonstrated the concept of silicone tubing in 1972. They found that children who generally could not tolerate the packing experience improved comfort when silicone rubber tubes were added below the packing.24 In our clinical practice, we noticed that deviated septum and mucosa swelling may compromise the intranasal airflow. After nasal fracture reduction and proper hemostasis, we tried to minimize the packing discomfort by inserting two segments of catheters into both inferior nasal meatuses. The catheters redirect the airstream communications via the common meatus. The swallowing-induced negative pressure was then decreased after smooth ventilating between the nasopharynx and the external world. The tube method enables early nasal respiration and reduces patients' discomforts.
In the survey of patient discomfort and subsequent physiologic and psychological changes, the NOSE scale was used and is a promising and reliable method to evaluate subjective discomfort such as nasal obstruction, nasal congestion, sleep disturbance, trouble breathing, and inability to move air through nose.14 ; 15 The experimental group had significantly lower VAS scores than the control group (p ≤0.001) Therefore, the tube technique is appropriate to reduce patient discomfort.
The commercially available Doyle Combo Splint (DCS) containing silicone nasal airway and Rhinocell (expandable sponge, Boston Medical Products Inc., MA, USA) can serve the same purpose compared with our tube technique. Kim et al25 reported that DCS was useful in maintaining nasal respiration and reducing the inconvenience to patients. However, the DCS is a nasal airway coating with an expandable sponge, and this device must go posteriorly to reach the nasopharynx. The DCS cannot be inserted superiorly to support the depressed bony pyramid. They still need a Vaseline gauze to packing the superior part of nasal cavity.
The advantages of the tube technique are as follows. (1) We can choose the proper diameter and length of tube according to each patients unique anatomy and different injury mechanism. (2) These catheters can also serve as septum support. (3) Gelfoam is accurately inserted into the superior meatus for hemostasis and also stabilized the fractured bony pyramid. A Gelfoam sterile compressed sponge has hemostatic properties and is usually liquefied within 2–5 days. (4) Invotec PVA sponges provide an effective tamponade effect to the nasal mucosa. It prevents further mucosa damage and adhesions in the nasal cavity. All of these factors promote quick healing by preventing additional mucosal damage and irritation. (5) In addition, the expanded Invotec sponges can fully fill the nasal cavity; they deliver pressure to the septum in coordination with silicone tubes. Nursing staff checked patients' respiration function frequently and cleaned the silicone tube by suction when needed. Removal of blood clotting or secretion will enhance patient comfort and maintain ventilation.
The main limitations of this study are its retrospective nature and its population of patients treated at only one hospital. Patient satisfaction is extremely subjective, and even objective evaluation relies on the individual patients opinions.
5. Conclusion
Compared to conventional methods, CANS is more accurate for detecting NBF. We recommend its use as an alternative tool for diagnosing nasal fracture. Because the tube technique balances pressure between the nasopharynx and middle ear during swallowing, patient comfort is enhanced. Application of these modifications can improve accuracy in diagnosing NBF and can improve the quality of NBF treatment.
References
- 1 Y.T. de Villers, R.C. Schultz; Nasal fractures; J Trauma, 15 (1975), pp. 319–327
- 2 M. Clayton, T. Lesser; The role of radiography in the management of nasal fractures; J Laryngol Otol, 100 (1986), pp. 797–801
- 3 G.J. de Lacey, B.K. Wignall, S. Hussain, J.R. Reidy; The radiology of nasal injuries: problems of interpretation and clinical relevance; Br J Radiol, 50 (1977), pp. 412–414
- 4 B.D. Daly, J.L. Russel, M.J. Davidson, J.T. Lamb; Thin section computed tomography in the evaluation of nasoethmoidal trauma; Clin Radiol, 41 (1990), pp. 272–275
- 5 V. Mondin, A. Rinaldo, A. Ferlito; Management of nasal bone fractures; Am J Otolaryngol, 26 (2005), pp. 181–185
- 6 K. Kishibe, S. Saitou, Y. Harabuchi; Significance of ultrasonography for nasal fracture; Nippon Jibiinkoka Gakkai Kaiho, 108 (2005), pp. 8–14
- 7 J. Danter, M. Klinger, R. Siegert, et al.; Ultrasound imaging of nasal bone fractures with a 20-MHz ultrasound scanner; HNO, 44 (1996), pp. 324–328
- 8 H.S. Hong, J.G. Cha, S.H. Paik, et al.; High-resolution sonography for nasal fracture in children; AJR Am J Roentgenol, 188 (2007), pp. W86–92
- 9 M.H. Lee, J.G. Cha, H.S. Hong, et al.; Comparison of high-resolution ultrasonography and computed tomography in the diagnosis of nasal fractures; J Ultrasound Med, 28 (2009), pp. 717–723
- 10 C.H. Park, H.H. Joung, J.H. Lee, et al.; Usefulness of ultrasonography in the treatment of nasal bone fractures; J Trauma, 67 (2009), pp. 1323–1326
- 11 B.J. Bailey; Nasal fractures; B.J. Bailey (Ed.), Head and Neck Surgery – Otolaryngology, vol. 1, JB Lippincott Company, Philadelphia, PA (1993)
- 12 R.J. Rohrich, W.P. Adams Jr.; Nasal fracture management: minimizing secondary nasal deformities; Plast Reconstr Surg, 106 (2000), pp. 266–273
- 13 Y.T. Lou, H.L. Lin, S.S. Lee, et al.; Conductor-assisted nasal sonography: an innovative technique for rapid and accurate detection of nasal bone fracture; J Trauma, 72 (2012), pp. 306–311
- 14 M.G. Stewart, D.L. Witsell, T.L. Smith, et al.; Development and validation of the Nasal Obstruction Symptom Evaluation (NOSE) scale; Otolaryngol Head Neck Surg, 130 (2004), pp. 157–163
- 15 M.G. Stewart, T.L. Smith, E.M. Weaver, et al.; Outcomes after nasal septoplasty: results from the Nasal Obstruction Septoplasty Effectiveness (NOSE) study; Otolaryngol Head Neck Surg, 130 (2004), pp. 283–290
- 16 S.H. Keng; Helmet use and motorcycle fatalities in Taiwan; Accid Anal Prev, 37 (2005), pp. 349–355
- 17 O.J. Becker; Nasal fractures; Arch Otolaryngol, 48 (1948), pp. 344–361
- 18 A. Nigam, A. Goni, A. Benjamin, A.R. Dasgupta; The value of radiographs in the management of the fractured nose; Arch Emerg Med, 10 (1993), pp. 293–297
- 19 R.L. Arden, R.H. Mathog; Nasal fractures; C.W. Cummings, J.M. Fredrickson, L.A. Harker (Eds.), et al., Otolaryngology – Head and Neck Surgery (2nd ed.), Mosby Year Book, St Louis (1993), pp. 737–753
- 20 O. Zagolski, P. Strek; Ultrasonography of the nose and paranasal sinuses; Pol Merkur Lekarski, 22 (2007), pp. 32–35
- 21 R. Gurkov, D. Clevert, E. Krause; Sonography versus plain X-rays in diagnosis of nasal fracture; Am J Rhinol, 22 (2008), pp. 613–616
- 22 A. Mohammadi, R. Javadrashid, A. Pedram, et al.; Comparison of ultrasonography and conventional radiography in the diagnosis of nasal bone fractures; Iran J Radiol, 6 (2009), pp. 7–11
- 23 A. Mohammadi, M. Ghasemi-Rad; Nasal Bone Fracture – Ultrasonography or computed tomography?; Med Ultrason, 13 (2011), pp. 292–295
- 24 R.L. Goode, T.R. Spooner; Management of nasal fractures in children. A review of current practices; Clin Pediatr (Phila), 11 (1972), pp. 526–529
- 25 H.Y. Kim, S.R. Kim, J.H. Park, et al.; The usefulness of nasal packing with Vaseline gauze and airway silicone splint after closed reduction of nasal bone fracture; Arch Plast Surg, 39 (2012), pp. 612–617
- 26 O. Thiede, J.H. Krömer, C.C. Rudack, et al.; Comparison of ultrasonography and conventional radiography in the diagnosis of nasal fractures; Arch Otolaryngol Head Neck Surg, 131 (2005), pp. 434–439
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?