Highlights
- Artemisinin modulates △ψm and caspase 3 apoptotic pathways.
- Artemisinin induces ERK/CREB signaling pathway.
- Artemisinin protects RPE cells against H2 O2 -induced oxidative stress.
- Artemisinin suppresses H2 O2 -induced the increase of ROS in RPE cells.
Abstract
The pathological increase in the levels of reactive oxygen species (ROS) in the retinal pigment epithelium (RPE), is implicated in the development of age-related macular degeneration (AMD). The discovery of drug candidates to effectively protect RPE cells from oxidative damage is required to resolve the pathological aspects and modify the process of AMD. In this study, a FDA-approved anti-malaria drug, Artemisinin was found to suppress hydrogen peroxide (H2 O2 )-induced cell death in human RPE cell-D407 cells. Further study showed that Artemisinin significantly suppressed H2 O2− induced D407 cell death by restoring abnormal changes in nuclear morphology, intracellular ROS, mitochondrial membrane potential and apoptotic biomarkers. Western blotting analysis showed that Artemisinin was able to activate extracellular regulated ERK/CREB survival signaling. Furthermore, Artemisinin failed to suppress H2 O2 -induced cytotoxicity and the increase of caspase 3/7 activity in the presence of the ERK inhibitor PD98059. Taken together, these results suggest that Artemisinin is a potential protectant with the pro-survival effects against H2 O2 insult through activation of the ERK/CREB pathway.
Grphical abstract
Keywords
Retinal pigment epithelial cells ; Age-related macular degeneration ; Artemisinin ; ROS ; ERK
1. Introduction
Age-related macular degeneration (AMD) is a progressive degenerative eye disorder which is mainly caused by a breakdown of the macula in the retina. At early stage of AMD, it does not lead to any symptoms or vision loss. However, late AMD seriously affects vision and further influences daily activities such as driving, reading, face recognition and life quality [1] . In the developed world, AMD is the common leading cause of blindness and its incidence keeps increasing in the people with age 65 or older [2] . AMD can be divided into two types: dry AMD 85–90%) and wet AMD 10–15%). At present, the current therapies such as laser photocoagulation, photodynamic therapy and anti-VEGF therapy are limited to wet AMD, but the more prevalent dry AMD still lacks effective therapies [3] and [4] .
The clinical characteristic of dry AMD is a decrease in chorioretinal blood flow [5] . Chorioretinal atrophy results in subsequent degeneration of retinal pigment epithelium (RPE) cells. The RPE, a pigmented monolayer, plays a critical role in maintaining retinal functions such as nutrient transport, formation of the outer blood retinal barrier to block the passage of water and ions, the phagocytosis of photoreceptor outer segment tips as well as the regeneration of visual pigments etc [6] , [7] and [8] . Age-associated degeneration of RPE eventually lead to loss of photoreceptor cells and vision loss in the affected area [9] . Thus, the identification of effective drug candidates to protect RPE cells from death may be a potential strategy for reducing the process of dry AMD.
Although the etiology and pathogenesis of dry AMD are not fully elucidated, age-related alterations such as increased oxidative stress and decreased cell density in the RPE were considered as main changes in dry AMD [10] , [11] , [12] , [13] , [14] and [15] . The adequate oxygen distribution and supply are necessary for maintenance of retinal function [16] . Due to high-oxygen microenvironment in the retina, RPE cells are exposed to constant oxidative stress resulting from reactive oxygen species (ROS) caused by intense light exposure [17] . Light-induced retinal damage leads to the increase of ROS such as superoxide radical (·O2− ), hydroxyl radical (·OH) and hydrogen peroxide (H2 O2 ). High levels of ROS damage the RPE cells, which have been linked with the pathogenesis of clinical visual diseases [17] . H2 O2 is an oxidizing agent, commonly used to cause irreversible oxidative damage and activation of the apoptotic cascade in various RPE cell models [18] and [19] . Therefore, H2 O2 -induced oxidative injury in RPE cell model, is suitable for investigating the effects of drug candidates for the treatment of dry AMD.
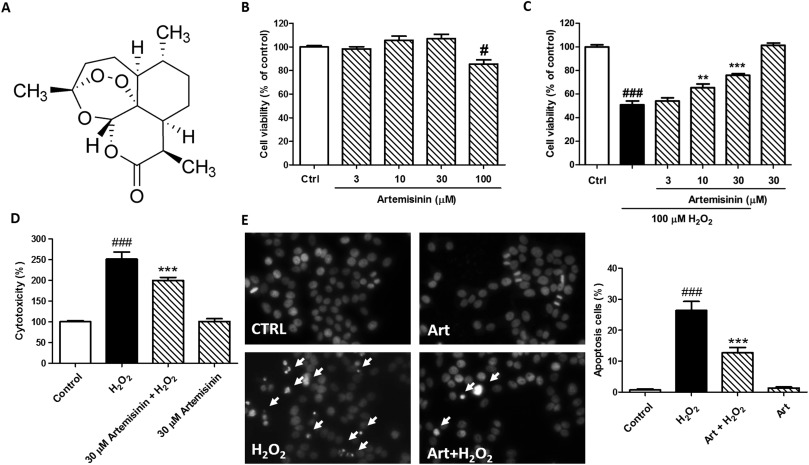
Recently, we perform H2 O2 -induced RPE cell injury model to identify potential protective candidates from various Chinese medicine. Artemisinin (the chemical structure is shown in Fig. 1 A), a FDA-approved anti-malarial medicine, was found to exhibit the protective effect against H2 O2 -induced oxidative injury in the D407 (a human RPE cell line) cells. Artemisinin, a sesquiterpene lactone, was originally isolated from the qinghao (the Chinese name of plant Artemisia annua L .) by Chinese scientists [20] . At present, Artemisinin and its derivatives have been clinically used to treat malaria in the world with great safety. Accumulated studies indicate that Artemisinin and its derivatives have additional potential in anti-Inflammation [21] , immune-regulation [22] , anti-viruses [23] and anti-cancer [24] . In the present study, we found that the protective effect of Artemisinin against H2 O2 -induced oxidative damage in RPE cells was via restoring abnormal changes in nuclear morphology, intracellular ROS, mitochondrial membrane potential and caspase activation. We also investigated the roles of the ERK1/2 survival pathway in the protective effect of Artemisinin.
|
|
|
Fig. 1. Protective effects of Artemisinin against H2 O2 -induced cytotoxicity in D407 cells. (A) The structure of Artemisinin. (B) Cells were treated with Artemisinin (3–100 µM) or 0.1% DMSO (vehicle control) for 24 h and cell viability was measured using the MTT assay. Cells were pre-treated with Artemisinin at indicated concentration or 0.1% DMSO (vehicle control) for 2 h and then incubated with or without 100 µM H2 O2 for a further 24 h. Cell viability and the release of LDH were measured by MTT assay (C) and LDH assay (D), respectively. (E) Apoptosis of D407 cells was detected by staining with Hoechst 33342 and visualized by fluorescence microscopy. The number of apoptotic nuclei with condensed chromatin was counted from the photomicrographs and presented as a percentage of the total number of nuclei. # P<0.05, ### P<0.005 versus control group;**P<0.01,***P<0.005 versus the H2 O2 -treated group were considered statistically significant differences. |
2. Materials and methods
2.1. Materials
3-(4,5-dimethylthiazol-2-yl)−2,5-diphenyl tetrazolium bromide (MTT), CellROX® Deep Red Reagent, 5,5′,6,6′-tetrachloro-1,1′,3,3′-tetraethyl-benzimidazolyl-carbocyanineiodide (JC-1), and Hoechst 33342 were purchased from Molecular Probes (Eugene, OR, USA). DMSO is from Sigma (Sigma, US). Horseradish peroxidase-conjugated anti-rabbi, anti-beta-actin, anti-phospho-CREB, anti-CREB, anti-phospho-Akt, anti-Akt, anti-phospho-ERK1/2 and anti-ERK1/2 were purchased from Cell Signaling Technology (Woburn, USA). PD98059 and LY294002 were obtained from Merck Millipore. Super Signal West Pico chemiluminescent substrate was purchased from Thermo Scientific (Rockford, IL, USA). Gibco® fetal bovine serum (FBS) and penicillin-streptomycin (PS) were purchased from Life Technologies (Grand Island, NY, USA).
2.2. Cell culture
Human retinal pigment epithelial cell line D407 was obtained from cell bank, Sun Yat-sen University (Guangzhou, China). Cell passages 5–10 were used for all experiments and cell cultures were maintained in 75-cm2 tissue culture flasks in DMEM supplemented with 10% FBS, streptomycin 100 μg/ml, penicillin 100 U/ml, and incubated at 37 °C with 5% CO2 humidified atmosphere. The medium was replaced every 2 days, and cells were sub-cultured by trypsin treatment twice a week, at a 1:5 split ratio.
2.3. MTT assay
Cell viability was determined by MTT assay with a slight modification of the protocol described by Zheng and Quirion [25] . Briefly, D407 cells were seeded in 96-well plates at a density of 2×104 cells/well. After serum starvation, the cultures were exposed to reagents for 24 h. Thereafter, the cells were incubated with MTT (0.5 mg/ml) for an additional 3 h. The medium was aspirated from each well and DMSO (100 µL) was added. Absorbance at 570 nm was measured by Infinite M200 PRO Multimode Microplate (Tecan, Switzerland). Cell viability was presented as a percentage compared with the control group.
2.4. LDH assay
Cell cytotoxicity was determined by measuring the activity of lactate dehydrogenase (LDH) released into the incubation medium when cellular membranes were damaged. D407 cells were seeded into 96-well plates (5×103 cells/well). After appropriate treatment, the activity of released LDH in the medium was determined according to the instructions of CytoTox-ONE™ Homogeneous Membrane Integrity Assay (Promega, USA). The fluorescent intensity was measured using Infinite M200 PRO Multimode Microplate at an excitation wavelength of 560 nm and emission at 590 nm. All values of % LDH released were normalized to the control group.
2.5. Hoechst 33342 staining
D407 cells were seeded into 12-well plates (8×104 cells/well). After appropriate treatment, these cells were washed with PBS, fixed with 4% formaldehyde (v/v in PBS) and then stained with 10 μg/ml Hoechst 33342 for 15 min at room temperature. After washing with PBS, the nuclei were visualized using EVOS FL Imaging System (Thermo Fisher Scientific, USA).
2.6. Measurement of intracellular ROS levels
Intracellular ROS generation was evaluated using CellROX® Deep Red Reagent (Thermo Fisher Scientific, USA). The cells were incubated with CellROX® Deep Red Reagent (5 µM) in DMEM for 1 h in the dark, rinsed twice with 1x PBS solution and the fluorescence was observed and recorded using a fluorescent microscope at an excitation wavelength of 640 nm and an emission wavelength of 665 nm. Semi-quantification of ROS level was assessed by using Image-J software. All values of % ROS level were normalized to the control group.
2.7. Measurement of mitochondrial membrane potential (△ψm)
JC-1 dye was used to monitor mitochondrial integrity. In brief, D407 cells were seeded into black 96-well plates (1×104 cells/well). After appropriate treatment, the cells were incubated with JC-1 (10 μg/ml in medium) at 37 °C for 15 min and then washed twice with PBS. For signal quantification, the intensity of red fluorescence (excitation 560 nm, emission 595 nm) and green fluorescence (excitation 485 nm, emission 535 nm) were measured using a Infinite M200 PRO Multimode Microplate. Mitochondrial membrane potential (△ψm) was calculated as the ratio of JC-1 red/green fluorescence intensity and the value was normalized to the control group. The fluorescent signal in the cells was also observed and recorded with a fluorescent microscope.
3. Caspase 3/7 activity assay
After treatment, the activity of caspase 3/7 was measured using the commercially available Caspase-Glo® 3/7 Assay (Invitrogen, USA) according to the manufacturers protocol. Briefly, D407 cells were lysed in lysis buffer and centrifuged at 12,500×g for 5 min 15 µL of cell lysate was incubated with 50 µL of 2X substrate working solution at room temperature for 30 min in 96-well plates. The fluorescence intensity was then determined by Infinite M200 PRO Multimode Microplate at an excitation wavelength of 490 nm and emission at 520 nm. The fluorescence intensity of each sample was normalized to the protein concentration of sample. All values of % caspase 3/7 activities were normalized to the control group.
3.1. Western blotting
Western blotting was performed as previously described [25] . Briefly, treated cells from different experimental conditions were rinsed once with ice-cold PBS and lysed in RIPA buffer [50 mM Tris–HCl pH 8.0, 150 mM NaCl, 1 mM EDTA, 1% Igepal CA-630, 1% sodium dodecyl sulfate (SDS), 50 mM NaF, 1 mM NaVO3, 5 mM phenylmethysulfonyl fluoride, 10 μg/ml leupeptin (Sigma), and 50 μg/ml aprotinin (Sigma) or 2× sample buffer (final concentration of 62.5 mM Tris–HCl pH 6.8, 2% (w/v) SDS, 10% glycerol, 50 mM dithiothreitol, and 0.1% (w/v) bromophenol blue)]. Samples with equal amounts of protein determined with a BCA protein assay kit according to the manufacturer’s instructions, were separated by SDS polyacrylamide gel electrophoresis (PAGE) and transferred to PVDF membranes. The phosphorylation of Akt and ERK1/2 was determined by Western blotting with their respective phospho-specific antibodies while β-actin was using as a total protein control. Blot was visualized using ECL kit according to the manufacturers instructions. The blots were stripped, and reprobed with anti-Akt or anti-ERK1/2, respectively. The intensity of the bands was quantified using ImageJ software.
3.2. Statistical analysis
Statistical analysis was performed using GraphPad Prism 5.0 statistical software (GraphPad software, Inc., San Diego, CA, USA). All experiments were performed in triplicate. Data are expressed as mean±standard deviation (SD). Statistical analysis was carried out using one-way ANOVA followed by Tukeys multiple comparison, with p<0.05 considered statistically significant.
4. Results
4.1. Artemisinin attenuated H2 O2 -induced D407 cell death
To evaluate the cytotoxicity of Artemisinin, D407 cells were incubated with various concentrations of Artemisinin for 24 h and the cytotoxicity was determined by MTT assay. As shown in Fig. 1 B, Artemisinin at between 3 and 30 μM did not cause any cytotoxicity in D407 cells compared to the control group, and was used in further experiments. To test the protective effects of Artemisinin, D407 cells were treated with Artemisinin for 2 h before being exposed to H2 O2 for 24 h. The result of MTT assay showed that the treatment of 100 μM H2 O2 resulted in dominant cell death (50%), whereas pre-treatment with 3, 10 and 30 μM of Artemisinin significantly attenuated H2 O2 -induced cell death in a concentration-dependent manner (54%, 65% and 75%, respectively) (Fig. 1 C). The protective activity of Artemisinin was also confirmed by the lactate dehydrogenase (LDH) assay. As shown in Fig. 1 D, pre-treated cells with 30 μM of Artemisinin for 2 h significantly reduced H2 O2 -induced LDH leakage (from 251% to 199%). Nuclei condensation was observed in D407 cells after exposure to 100 μM H2 O2 (26%) in Hoechst 33342 staining assay. However, a pre-treatment of 30 μM Artemisinin decreased these changes (9%) (Fig. 1 E). Artemisinin alone did not lead to nuclear morphological change of D407 cells.
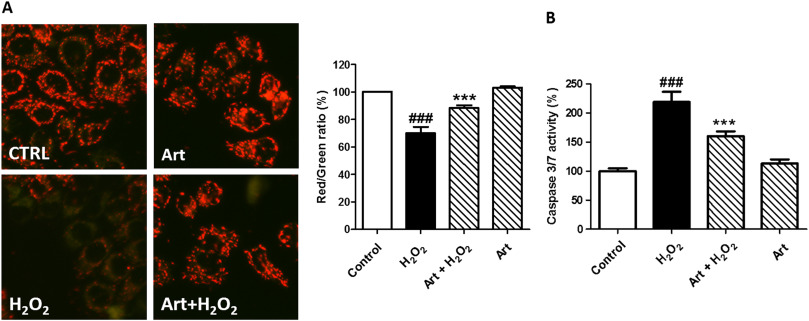
4.2. Artemisinin decreased H2 O2 -induced change of mitochondrial membrane potential and caspase 3/7 activity
Mitochondrial inhibition causes the loss of mitochondrial membrane potential (△ψm). To determine whether Artemisinin could reduce H2 O2 -induced △ψm loss, the △ψm in D407 cells was assessed by analyzing the red/green fluorescent intensity ratio of JC-1 staining. Exposure of D407 cells to 100 μM H2 O2 resulted in an increase in green fluorescence intensity indicating △ψm dissipation (69%) (Fig. 2 A). Pre-treatment with Artemisinin at 30 μM for 2 h attenuated H2 O2 -induced △ψm loss (88%).
|
|
|
Fig. 2. Artemisinin attenuated H2 O2 -induced mitochondrial membrane potential (△ψm) loss and caspase 3/7 activity increase in D407 cells. After pre-treatment with 30 μM Artemisinin or 0.1% DMSO (vehicle control) for 2 h, D407 cells were incubated with or without 100 μM H2 O2 for another 24 h. (A) △ψm was determined by the JC-1 assay. (B) Quantification of caspase 3/7 activity was determined by caspase 3/7 activity assay. ### P<0.005 versus control group;***P<0.005 versus H2 O2 -treated group was considered significantly different. |
Caspase 3/7 is a main biomarker in the apoptosis of dopaminergic neuronal cells. As shown in Fig. 2 B, treatment of cells with 100 μM H2 O2 for 24 h increased caspase 3/7 activity by more than 2-fold compared to the control group (219%). In contrast, pre-treatment with Artemisinin significantly reduced caspase 3/7 activation induced by H2 O2 (160%).
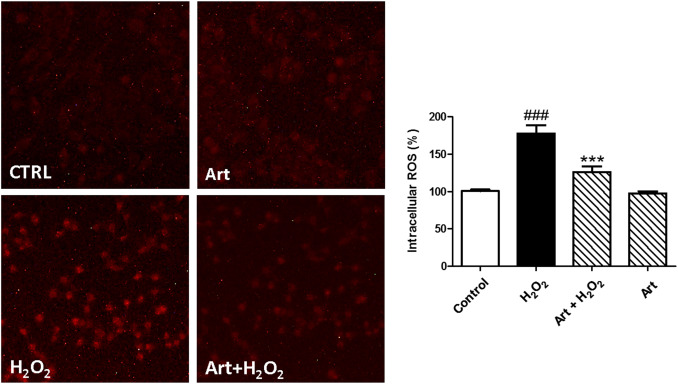
4.3. Artemisinin suppressed H2 O2 -induced increase of intracellular ROS
The accumulation of excess ROS is considered to be one of the main causes of cell damage induced by H2 O2 . Intracellular ROS were measured by staining with a fluorescent probe, CellROX® Deep Red Reagent, in D407 cells. As shown in Fig. 3 , 100 μM H2 O2 caused a significant increase in fluorescent intensity in the cells compared to the control group (177%). However, the increase in ROS was significantly suppressed by pretreatment with Artemisinin at 30 μM (126%).
|
|
|
Fig. 3. Artemisinin reduced the increase of H2 O2 -induced oxidative stress in D407 cells. After pre-treatment with 30 μM Artemisinin or 0.1% DMSO (vehicle control) for 2 h, D407 cells were incubated with or without 100 μM H2 O2 for another 24 h. Intracellular ROS level was determined by the CellROX® Deep Red Reagent. ### P<0.005 versus control group;***P<0.005 versus H2 O2 -treated group was considered significantly different. |
4.4. Artemisinin up-regulated ERK/CREB signaling
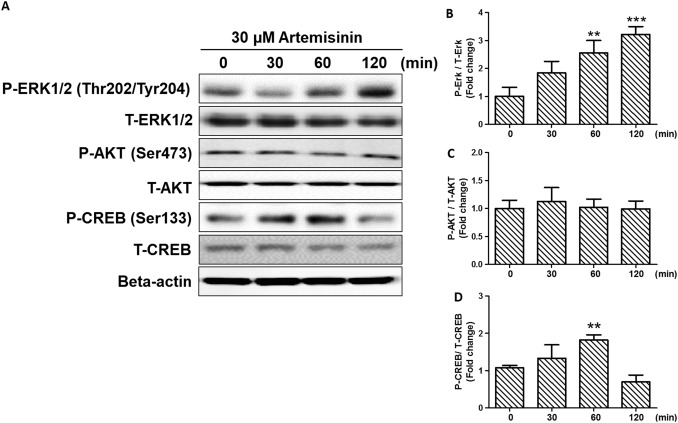
Previous studies indicated that Artemisinin was able to activate ERK signaling in various cell models [26] , [27] and [28] . ERK was found to be involved in the inhibition of apoptosis. To determine whether the ERK signaling pathway is regulated by Artemisinin in D407 cells, D407 cells were treated with 30 μM Artemisinin for 0, 0.5, 1, and 2 h and then the phosphorylation of ERK1/2 (Thr202/Tyr204) was examined by Western blot analysis. As shown in Fig. 4 A and B, Artemisinin gradually increased the phosphorylation intensity of ERK1/2 in D407 cells within 2 h. These results suggested that ERK survival signaling could be activated by Artemisinin. In contrast, Artemisinin had no effect on the phosphorylation of AKT, a serine/threonine kinase implicated in cell survival (Fig. 4 A and C). CREB is an ERK-mediated nuclear transcription factor involved in many biological functions including neuronal survival. The results of Western blotting showed that the phosphorylation of CREB (Ser133) was increased significantly by Artemisinin (Fig. 4 D).
|
|
|
Fig. 4. Involvement of ERK/CREB signaling in the cytoprotective effect of Artemisinin. (A) D407 cells were pre-treated with 30 µM Artemisinin. The cells were collected at 0, 30, 60, and 120 min. The expression of phosphorylated ERK1/2, total ERK1/2, phosphorylated Akt, total Akt and phosphorylated CREB, total CREB and beta-actin were detected by Western blotting with specific antibodies (A). (B)(C)(D) Quantification of representative protein band from Western blotting. **P<0.01,***P <0.005 versus the 0 min group was considered significantly different. |
4.5. ERK signaling was involved in the protective effect of Artemisinin
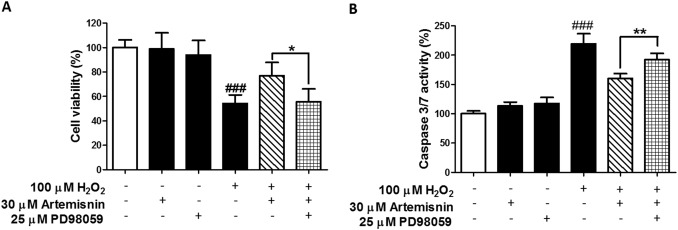
To further confirm the involvement of ERK signaling in the protective effects of Artemisinin, the ERK pathway inhibitor PD98059 was used in cell survival assay with H2 O2 cytotoxicity. As shown in Fig. 5 A, the protective effect of Artemisinin was abolished by the application of PD98059 in MTT assay. Similar results were obtained from caspase 3/7 assay which showed that Artemisinin failed to suppress the increase of caspase 3/7 activity in the presence of the ERK pathway inhibitor (Fig. 5 B), suggesting that ERK signaling is involved in the protective effects of Artemisinin.
|
|
|
Fig. 5. The ERK pathway inhibitor PD98059 attenuated the protective effects of Artemisinin. D407 cells were pre-treated with 30 µM Artemisinin and 25 µM PD98059 for 2 h and then incubated with or without H2 O2 for a further 24 h. Cell viability and caspase 3/7 activity were measured by MTT assay (A) and caspase 3/7 activity assay (B). ### P<0.005 versus control group;*P<0.05,**P<0.01 versus the Artemisinin+H2 O2 -treated group was considered significantly different. |
5. Discussion
Oxidative stress in the retina plays a critical role in the pathogenesis of dry AMD. Although antioxidant defense mechanisms in retinal cells are sufficient to counteract weak oxidative stress, strong oxidative stress disrupt normal antioxidant mechanisms and result in irreversible damage to the retina. Using additional antioxidant to suppress oxidative stress is reported to avoid oxidative damage and maintain the function of retina. Yttrium oxide nanoparticles are excellent free radical scavengers prevent photoreceptor death in a light-damage model of retinal degeneration [29] . In addition, experimental and clinical studies suggest that taking high dose of antioxidant vitamins and zinc supplements are potential strategies for delaying the progression of AMD and vision loss [30] . In this study, we found that 100 µM H2 O2 resulted in the collapse of the △ψm and increase of ROS in RPE cells while pre-treatment of Artemisinin was able to significantly suppress these abnormal changes in D407 RPE cells. Apoptosis is a frequent type of cell death observed in RPE cells [31] . The decrease of cell viability, the increase of LDH release and nuclear morphological changes induced by H2 O2 were significantly suppressed by Artemisinin (Fig. 1 ), suggesting that anti-oxidant activity of Artemisinin contributes to its protective effects. The concentration range of artemisinin (10–30 µM) used in our experiments has no toxicity in D407 cells and is therapeutically relevant based on the in vitro quantitation with malaria plasmodion indicate that Atemisinin is a safe protectant [43] .
Increased mitochondrial DNA damage and protein loss of election transport chain in RPE cells have been found in AMD patients, suggesting that mitochondrial dysfunction plays a key role in the process of AMD [32] , [33] , [34] and [35] . Mitochondrial apoptotic pathway due to mitochondria deficiency plays a critical role in the pathogenesis of retinal diseases. It has been reported that strategies to block mitochondrial apoptotic pathway are potential therapeutics to prevent retinal pigment epithelial cells death. In this study, our results showed that H2 O2 -induced △ψm loss could be suppressed by pre-treatment with Artemisinin. The increase of intracellular ROS induced by H2 O2 , leads to damage to the mitochondrial membrane and results in the collapse of the △ψm and activation of the apoptotic cascade [36] , [37] , [38] and [39] . Pre-treatment with Artemisinin was able to suppress the activation of caspase 3/7 (Fig. 3 ).
ERK/CREB pathway is a central signaling component that plays a role in the initiation and regulation of most of the stimulated cellular processes such as proliferation, survival and differentiation [40] . Both AKT and ERK survival pathways are reported as a key signaling to induce CREB phosphorylation and cellular anti-oxidant mechanism [41] and [42] . In our study, the increase in CREB phosphorylation, following treatment with Artemisinin, was observed. However, it was noted that ERK, no AKT, could be activated by Artemisinin. Furthermore, our results showed that Artemisinin failed to suppress H2 O2 -induced cytotoxicity and the increase of caspase 3/7 activity in the presence of the ERK inhibitor PD98059 (Fig. 5 ). Therefore, these results provide mechanistic evidence to support the notion that Artemisinin-regulated protective effects against H2 O2 -induced oxidative stress occur via ERK dependent CREB activation.
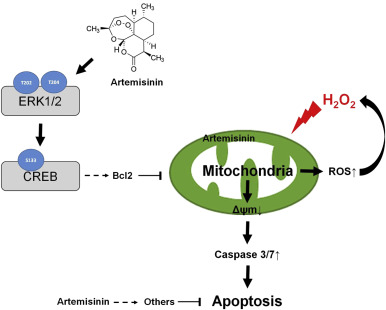
In summary, our findings demonstrate that Artemisinin is able to reduce H2 O2 -induced oxidative stress in D407 retinal pigment epithelial cells through the regulation of multiple mechanisms including (1) inhibiting the generation of intracellular ROS; (2) modulating △ψm and caspase 3/7 dependent pathway; (3) activating ERK1/2 signaling (Fig. 6 ). The protective effects of Artemisinin to attenuate H2 O2 -mediated intrinsic mitochondrial apoptotic pathway are, at least in part, mediated via the activation of ERK1/2 signaling. Our results offer support for the potential development of Artemisinin to prevent retinal pigment epithelial cells death in the process of AMD.
|
|
|
Fig. 6. The possible mechanism of Artemisinin. |
Acknowledgements
This research was financially supported by the Guangdong Provincial Project of Science and Technology (2011B050200005 ), the National Natural Science Foundation of China (31371088 ), SRG2015-00004-FHS and MYRG2016–00052-FHS from University of Macau , and the Science and Technology Development Fund (FDCT) of Macao (FDCT 021/2015/A1 ).
References
- [1] A.L. Coleman, F. Yu, K.E. Ensrud, K.L. Stone, J.A. Cauley, K.L. Pedula, M.C. Hochberg, C.M. Mangione; Impact of age-related macular degeneration on vision-specific quality of life: follow-up from the 10-year and 15-year visits of the study of osteoporotic fractures; Am. J. Ophthalmol., 150 (2010), pp. 683–691
- [2] S. Resnikoff, I. Kocur, D.E. Etya’ale, T.O. Ukety; Vision 2020 – the right to sight; Ann. Trop. Med. Parasitol., 102 (Suppl 1) (2008), pp. S3–S5
- [3] A. Lux, H. Llacer, F.M. Heussen, A.M. Joussen; Non-responders to bevacizumab (Avastin) therapy of choroidal neovascular lesions; Br. J. Ophthalmol., 91 (2007), pp. 1318–1322
- [4] J. Ambati, B.K. Ambati, S.H. Yoo, S. Ianchulev, A.P. Adamis; Age-related macular degeneration: etiology, pathogenesis, and therapeutic strategies; Surv. Ophthalmol., 48 (2003), pp. 257–293
- [5] J.E. Grunwald, S.M. Hariprasad, J. DuPont, M.G. Maguire, S.L. Fine, A.J. Brucker, A.M. Maguire, A.C. Ho; Foveolar choroidal blood flow in age-related macular degeneration; Invest. Ophthalmol. Vis. Sci., 39 (1998), pp. 385–390
- [6] O. Strauss; The retinal pigment epithelium in visual function; Physiol. Rev., 85 (2005), pp. 845–881
- [7] D. Bok; The retinal pigment epithelium: a versatile partner in vision; J. Cell Sci. Suppl., 17 (1993), pp. 189–195
- [8] D. Bok; Processing and transport of retinoids by the retinal pigment epithelium; Eye, 4 (Pt 2) (1990), pp. 326–332
- [9] C.A. Curcio, P.L. Saunders, P.W. Younger, G. Malek; Peripapillary chorioretinal atrophy: Bruch’s membrane changes and photoreceptor loss; Ophthalmology, 107 (2000), pp. 334–343
- [10] R. Klein; Overview of progress in the epidemiology of age-related macular degeneration; Ophthalmic Epidemiol., 14 (2007), pp. 184–187
- [11] S.J. McGimpsey, U. Chakravarthy; VEGF-targeted therapy and beyond: pharmacotherapy and emerging Treatments in agerelated macular degeneration; Expert Rev. Clin. Pharmacol., 3 (2010), pp. 243–252
- [12] X. Ding, M. Patel, C.C. Chan; Molecular pathology of age-related macular degeneration; Progress. Retin. Eye Res., 28 (2009), pp. 1–18
- [13] P. Tokarz, K. Kaarniranta, J. Blasiak; Role of antioxidant enzymes and small molecular weight antioxidants in the pathogenesis of age-related macular degeneration (AMD); Biogerontology, 14 (2013), pp. 461–482
- [14] R.N. Mitra, S.M. Conley, M.I. Naash; Therapeutic approach of nanotechnology for oxidative stress induced ocular neurodegenerative diseases; Adv. Exp. Med. Biol., 854 (2016), pp. 463–469
- [15] Y.Z. Fang, S. Yang, G. Wu; Free radicals, antioxidants, and nutrition; Nutrition, 18 (2002), pp. 872–879
- [16] D.Y. Yu, S.J. Cringle; Oxygen distribution and consumption within the retina in vascularised and avascular retinas and in animal models of retinal disease; Progress Retin. Eye Res., 20 (2001), pp. 175–208
- [17] D.T. Organisciak, D.K. Vaughan; Retinal light damage: mechanisms and protection; Progress Retin. Eye Res., 29 (2010), pp. 113–134
- [18] M.H. Kim, J. Chung, J.W. Yang, S.M. Chung, N.H. Kwag, J.S. Yoo; Hydrogen peroxide-induced cell death in a human retinal pigment epithelial cell line, ARPE-19; Korean J. Ophthalmol., 17 (2003), pp. 19–28
- [19] L. Lu, S.F. Hackett, A. Mincey, H. Lai, P.A. Campochiaro; Effects of different types of oxidative stress in RPE cells; J. Cell. Physiol., 206 (2006), pp. 119–125
- [20] Y. Tu; The discovery of artemisinin (qinghaosu) and gifts from Chinese medicine; Nat. Med., 17 (2011), pp. 1217–1220
- [21] C. Shi, H. Li, Y. Yang, L. Hou; Anti-inflammatory and immunoregulatory functions of artemisinin and its derivatives; Mediat. Inflamm., 2015 (2015), p. 435713
- [22] C. Cheng, W.E. Ho, F.Y. Goh, S.P. Guan, L.R. Kong, W.Q. Lai, B.P. Leung, W.S. Wong; Anti-malarial drug artesunate attenuates experimental allergic asthma via inhibition of the phosphoinositide 3-kinase/Akt pathway; PLoS One, 6 (2011), p. e20932
- [23] T. Efferth, M.R. Romero, D.G. Wolf, T. Stamminger, J.J. Marin, M. Marschall; The antiviral activities of artemisinin and artesunate; Clin. Infect. Dis., 47 (2008), pp. 804–811
- [24] A.K. Das; Anticancer effect of antimalarial artemisinin compounds; Ann. Med. Health Sci. Res., 5 (2015), pp. 93–102
- [25] W.H. Zheng, R. Quirion; Glutamate acting on N-methyl-D-aspartate receptors attenuates insulin-like growth factor-1 receptor tyrosine phosphorylation and its survival signaling properties in rat hippocampal neurons; J. Biol. Chem., 284 (2009), pp. 855–861
- [26] W. Zheng, C.M. Chong, H. Wang, X. Zhou, L. Zhang, R. Wang, Q. Meng, P. Lazarovici, J. Fang, Artemisinin conferred ERK mediated neuroprotection to PC12 cells and cortical neurons exposed to sodium nitroprusside-induced oxidative insult. Free Radic. Biol. Med., 2016.
- [27] Sarina, Y. Yagi, O. Nakano, T. Hashimoto, K. Kimura, Y. Asakawa, M. Zhong, S. Narimatsu, E. Gohda; Induction of neurite outgrowth in PC12 cells by artemisinin through activation of ERK and p38 MAPK signaling pathways; Brain Res., 1490 (2013), pp. 61–71
- [28] S.H. Kim, S.Y. Chun, T.S. Kim; Interferon-alpha enhances artemisinin-induced differentiation of HL-60 leukemia cells via a PKC alpha/ERK pathway; Eur. J. Pharmacol., 587 (2008), pp. 65–72
- [29] R.N. Mitra, M.J. Merwin, Z. Han, S.M. Conley, M.R. Al-Ubaidi, M.I. Naash; Yttrium oxide nanoparticles prevent photoreceptor death in a light-damage model of retinal degeneration; Free Radic. Biol. Med., 75 (2014), pp. 140–148
- [30] Age-Related Eye Disease Study Research, G. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch. Ophthalmol., vol. 119, 2001, pp. 1417–1436.
- [31] E. Kucuksayan, E.K. Konuk, N. Demir, B. Mutus, M. Aslan; Neutral sphingomyelinase inhibition decreases ER stress-mediated apoptosis and inducible nitric oxide synthase in retinal pigment epithelial cells; Free Radic. Biol. Med., 72 (2014), pp. 113–123
- [32] H. Lin, H. Xu, F.Q. Liang, H. Liang, P. Gupta, A.N. Havey, M.E. Boulton, B.F. Godley, D.N.A. Mitochondrial; damage and repair in RPE associated with aging and age-related macular degeneration; Invest. Ophthalmol. Vis. Sci., 52 (2011), pp. 3521–3529
- [33] P.P. Karunadharma, C.L. Nordgaard, T.W. Olsen, D.A. Ferrington, D.N.A. Mitochondrial; damage as a potential mechanism for age-related macular degeneration; Invest. Ophthalmol. Vis. Sci., 51 (2010), pp. 5470–5479
- [34] M.R. Terluk, R.J. Kapphahn, L.M. Soukup, H. Gong, C. Gallardo, S.R. Montezuma, D.A. Ferrington; Investigating mitochondria as a target for treating age-related macular degeneration; J. Neurosci., 35 (2015), pp. 7304–7311
- [35] C.L. Nordgaard, P.P. Karunadharma, X. Feng, T.W. Olsen, D.A. Ferrington; Mitochondrial proteomics of the retinal pigment epithelium at progressive stages of age-related macular degeneration; Invest. Ophthalmol. Vis. Sci., 49 (2008), pp. 2848–2855
- [36] P. Nicotera; Caspase requirement for neuronal apoptosis and neurodegeneration; IUBMB Life, 49 (2000), pp. 421–425
- [37] M.T. Lin, M.F. Beal; Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases; Nature, 443 (2006), pp. 787–795
- [38] G.S. Salvesen; Caspases: opening the boxes and interpreting the arrows; Cell Death Differ., 9 (2002), pp. 3–5
- [39] F.W. Sunderman; The Chloride and Nitrogen Balances and Weight Changes in Pneumonia; 1, University Of Pennsylvania, Philadelphia (1929), pp. 313–332
- [40] M. Hytti, N. Piippo, A. Salminen, P. Honkakoski, K. Kaarniranta, A. Kauppinen; Quercetin alleviates 4-hydroxynonenal-induced cytotoxicity and inflammation in ARPE-19 cells; Exp. Eye Res., 132 (2015), pp. 208–215
- [41] C.M. Chong, Z.Y. Zhou, V. Razmovski-Naumovski, G.Z. Cui, L.Q. Zhang, F. Sa, P.M. Hoi, K. Chan, S.M. Lee; Danshensu protects against 6-hydroxydopamine-induced damage of PC12 cells in vitro and dopaminergic neurons in zebrafish; Neurosci. Lett., 543 (2013), pp. 121–125
- [42] B. Vurusaner, P. Gamba, G. Testa, S. Gargiulo, F. Biasi, C. Zerbinati, L. Iuliano, G. Leonarduzzi, H. Basaga, G. Poli; Survival signaling elicited by 27-hydroxycholesterol through the combined modulation of cellular redox state and ERK/Akt phosphorylation; Free Radic. Biol. Med., 77 (2014), pp. 376–385
- [43] N. Klonis, S.C. Xie, J.M. McCaw, M.P. Crespo-Ortiz, S.G. Zaloumis, J.A. Simpson, L. Tilley; Altered temporal response of malaria parasites determines differential sensitivity to artemisinin; Proc. Natl. Acad. Sci. USA, 110 (13) (2013), pp. 5157–5162
Document information
Published on 20/10/16
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?