Walled-off necrosis of the pancreas is defined as a mature, encapsulated collection of pancreatic and/or peripancreatic necrosis that has developed a well-defined inflammatory wall. It usually occurs > 4 weeks after onset of necrotizing pancreatitis [1] . Minimally invasive techniques are thought to induce less physiological stress as compared with open surgical necrosectomy [2] .
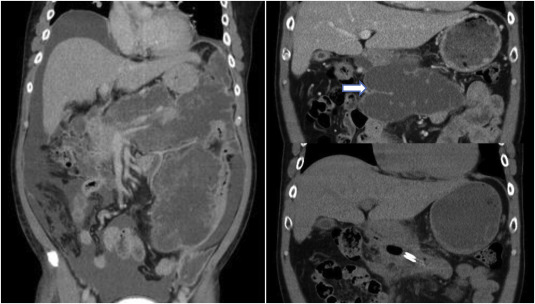
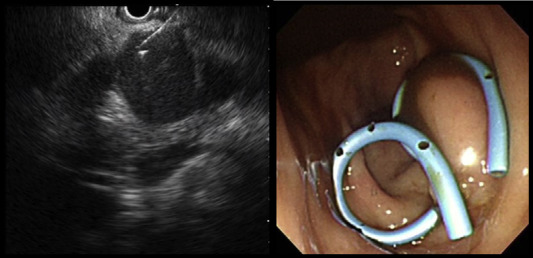
We report one case of successful drainage of walled-off necrosis of the pancreas by endoscopic transluminal drainage. This was a 52-year-old man who had just been admitted for acute necrotizing pancreatitis. Abdominal computed tomography (CT) showed extensive abscess formation in the retroperitoneum complicated with ascites (Figure 1 , left). He received CT-guided percutaneous drainage and the drainage catheter was removed because of poor function. Endoscopic retrograde pancreatography revealed a tortuous pancreatic duct, which communicated with the peripancreatic abscess cavity. Thus, a pancreatic duct stent was inserted. However, the following abdominal CT 3 months later still showed a large walled-off pancreatic necrosis (Figure 1 , right upper). We performed endoscopic ultrasound (EUS) puncture from the stomach to the walled-off necrosis and then inserted two double-pigtail stents (Figure 2 ).
|
|
|
Figure 1. This patient had pancreatitis and extensive lobulated abscess formation in retroperitoneum and left pararenal space complicated with dirty ascites ( Left). Three months later, abdominal CT still demonstrated a large walled-off necrosis with liquefaction in the peripancreatic space (Arrow), up to 17.3 cm in length (Right upper). Subsequent abdominal CT showed shrinkage of the necrosis after endoscopic-ultrasound-guided transluminal drainage (Right lower). CT = computed tomography. |
|
|
|
Figure 2. Endoscopic-ultrasound-guided puncture with 19G fine-needle aspiration biopsy needle was performed in the peripancreatic necrosis (Left), then two double-pigtail stents were inserted for drainage (Right). |
Immediately after EUS-guided cystogastrostomy, a large volume of brown fluid was drained into the stomach. Nine days after the procedure, abdominal CT demonstrated that the lesion size was decreasing (Figure 1 , right lower). The clinical symptoms also improved.
In patients with walled-off pancreatic necrosis with minimal symptoms, medical management without a drainage procedure is suggested. For patients who have large, symptomatic lesions, a drainage procedure should be considered. There are several options including surgical, transluminal, and percutaneous drainage.
EUS-guided cystogastrostomy is a less invasive intervention, with >90% being technically successful, with a 10–15% morbidity rate [3] ; [4] . Complications include secondary infection, bleeding, perforation, and stent migration. The most serious cause of bleeding is endoscopic puncturing of unrecognized pseudoaneurysms. Thus, preprocedural imaging studies such as CT scan are important to observe the lesion in detail and to avoid these complications.
Conflicts of interest
The authors declare no conflicts of interest.
References
- [1] P.A. Banks, T.L. Bollen, C. Dervenis, H.G. Gooszen, C.D. Johnson, M.G. Sarr, et al.; Classification of acute pancreatitis — 2012: revision of the Atlanta classification and definitions by international consensus; Gut, 62 (2013), pp. 102–111
- [2] S. van Brunschot, O.J. Bakker, M.G. Besselink, T.L. Bollen, P. Fockens, H.G. Gooszen, et al.; Treatment of necrotizing pancreatitis; Clin Gastroenterol Hepatol, 10 (2012), pp. 1190–1201
- [3] M.R. Antillon, R.J. Shah, G. Stiegmann, Y.K. Chen; Single-step EUS-guided transmural drainage of simple and complicated pancreatic pseudocysts; Gastrointest Endosc, 63 (2006), pp. 797–803
- [4] L.C. Hookey, S. Debroux, M. Delhaye, M. Arvanitakis, O. Le Moine, J. Devière; Endoscopic drainage of pancreatic-fluid collections in 116 patients: a comparison of etiologies, drainage techniques, and outcomes; Gastrointest Endosc, 63 (2006), pp. 635–643
Document information
Published on 15/05/17
Submitted on 15/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?