Keywords
Ventricular rupture;Ventricular septal rupture;Myocardial infarction;Mitral regurgitation
1. Introduction
Cardiac rupture (CR) is a life-threatening mechanical complication of acute myocardial infarction (MI). CR subsumes 3 pathogenetic entities in descending order of frequency including (i) free wall rupture (FWR), (ii) ventricular septal rupture (VSR) and (iii) papillary muscle rupture (PMR). The incidence of CR decreased from 6.2% to 3.2% in parallel with a progressive use of revascularization procedures and implementation of potent medication [5] ; [6]. In particular, the incidence of CR was highest in patients with a ST elevation myocardial infarction (STEMI, 0.9%) and lower in patients with non-ST elevation myocardial infarction (NSTEMI, 0.17%) or unstable angina (0.25%) [8]. Before use of reperfusion therapy, the incidence of VSR was 1–3% [1] ; [6]. Obviously, the incidence of VSR is declining (0.2–0.3%) in parallel with the decreasing incidence of CR since the inception of thrombolytic therapy [7] ; [8]. With the implementation of percutaneous coronary interventions (PCI), VSR has become an even rarer mechanical complication. Although reperfusion therapy reduces the size of the infarcted myocardium, it can also provoke hemorrhagic dissection or reperfusion injury, thus potentially accelerating the onset of VSR [3]; [9] ; [4]. Consequently, time from MI to onset of VSR may have been reduced from 5 days to 1 day in patients receiving reperfusion therapy [1]; [3]; [6] ; [9]. Notably, the intra-hospital mortality rate without surgical repair is about 74%–90%. Despite numerous improvements in surgical techniques, mortality rate remains high (20–45%) even in patients undergoing surgical repair, particularly when the RCA is the culprit lesion and cardiogenic shock is involved [3] ; [6]. We present a challenging case of a complex cardiac rupture complicating a silent subacute myocardial infarction which still should be remembered as a potential differential diagnosis though it has decreasing frequency.
2. Case report
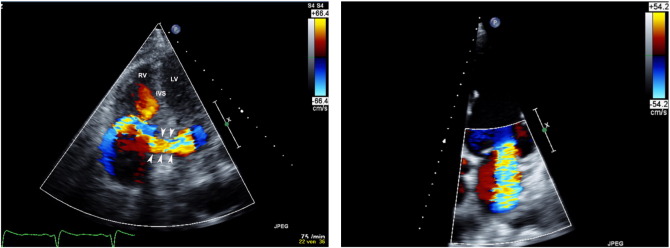
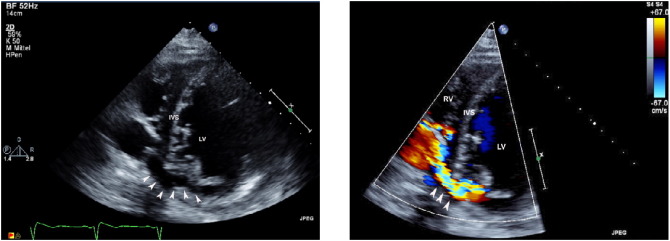
During the weekend, a 75-year old man was admitted to our department after an unclear syncope on his way to the supermarket. He was referred to cardiologic evaluation because of progressive dyspnea NYHA IIIb (New York Heart Association functional class IIIb) and deterioration of physical capacity during the weeks. Nevertheless he had not sought medical help during that interval. His medical history was completely clear, without any current medication. There was no history of previous syncopal episodes. At admission, the patient was tachycardic (100 beats/min) and his blood pressure was 140/90 mm Hg. Oxygen saturation was 93%, mild prominent jugular vein in 45° position could be inspected. On physical examination, there were signs of congestive heart failure, including lower leg edema on both sides. Moreover, bilateral basal crackles were evident without clinical signs of pleural effusion. During auscultation, a 3/6 holosystolic–diastolic murmur was apparent at the left sternal border. The 12-lead electrocardiogram showed a new onset of paroxysmal atrial fibrillation with 115 beats/min, insinuated Pardée Q waves in the lateral leads (I, aVL) and a left anterior hemibloc. The Troponin T level was 460 ng/ml, CK 192 U/L, CK-MB 20 U/L and the BNP level 12,815 pg/ml. Chest X-ray imaging showed signs of pulmonary congestion. We started a therapy with Furosemid i.v. and Xipamid p.o. for sequential nephron blockade. After recompensation by decreasing weight as well as pulmonary congestion and an improving clinical status, echocardiography was performed detecting a reduced left ventricular function (LVEF 24%). There was suspicion of a complex cardiac rupture with circumscribed pericardial effusion (end-diastolic 5 mm). Echocardiographic examination revealed a significant left-to-right shunt with a pulmonary-to-systemic flow ratio (Qp:Qs) of 3.4 and a velocity jet of 200 cm/s. In order to obtain information on the localization of the myocardial rupture and its anatomy, a transesophageal echocardiogram was performed. The CR was located at the posterobasal left ventricular free wall (LVFW) and seemed to have connected to the right ventricle through an intramyocardial tunnel via two formed intramyocardial cavities (LV 15 × 20 mm/RV 50 × 38 mm) (Figs. 1A, 2). Moreover, there was a severe mitral regurgitation due to papillary muscle dysfunction (Fig. 1B), resulting in a post-capillary pulmonary hypertension (Pasys70 mm Hg).
|
|
|
Fig. 1. Transthoracic two-dimensional apical four chamber views with color Doppler technique. (A) The image shows a significant left-to-right shunt (white arrowheads) at the junction between the basal inferior interventricular septum (IVS) and the inferoposterior wall. RV denotes right ventricle and LV left ventricle. (B) The image shows the severe mitral regurgitation. |
|
|
|
Fig. 2. Transthoracic short-axis views without (A) and with color Doppler technique (B). (A) The image shows trajectory (white arrowheads) from the left ventricle (LV) to the right ventricle. (B) The image shows a turbulent flow from the left ventricle (LV) to the right ventricle (RV) at the junction between the basal inferior interventricular septum (IVS) and the inferoposterior wall (white arrowheads). |
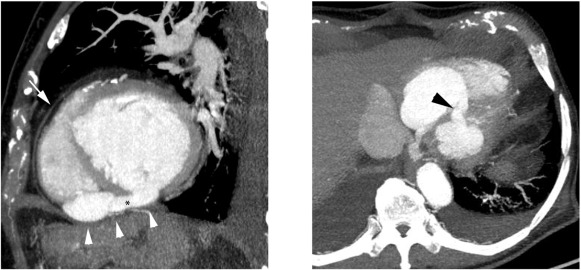
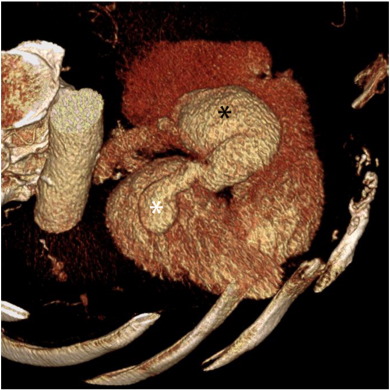
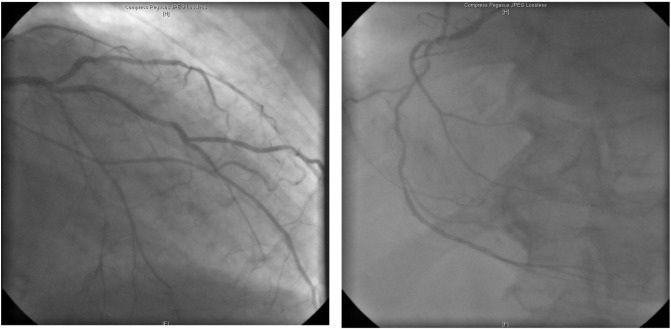
Additionally, a cardiac computer tomography (CT) was performed (Fig. 3, A and B). Through this, a rupture of the LVFW inferior at the basis of the heart could be assumed (diameter 2.3 mm). Adjacent to this, a radiocontrast agent filled cavity (6 × 4.3 mm) could be observed, which seemed to have connected to a defect at the inferior wall of the right ventricle (diameter 0.5 cm), corresponding to the echocardiographic suspicion of an entry point in the LVFW and an exit point in the right ventricle, causing an extracardiac left-to-right shunt via a pseudoaneurysm (Fig. 4). Urgent preoperative cardiac catheterization revealed a three-vessel coronary artery disease (Fig. 5). The patient was transferred to the department of cardiovascular surgery for urgent closure of CR with concomitant bypass graft surgery and mitral valve replacement. Intraoperative exploration by median sternotomy with subsequent longitudinal pericardiotomy revealed a dilated heart, several pericardial adhesions, but no suspected wall rupture. Thereafter, a cardiopulmonary bypass was established, the aorta cross-clamped, and the heart was arrested with a cardioplegic solution. Preparation of the sulcus interatrialis and a left atriotomy with exposure of the mitral valve was accomplished. After resection of the anterior leaflet of the mitral valve, a ventricular septal rupture within the posterior septum was clearly disclosed. Repair of the VSR was performed transvalvular through the resected mitral valve by means of an autologous pericardial patch (ca. 2 cm diameter) with running sutures. Afterwards, valve replacement was performed by using a mechanical valve (St. Jude Medical Masters expanded cuff-prosthesis, 29 mm) according to papillary dysfunction and severe mitral regurgitation. Concomitant coronary artery bypass grafting was performed using the saphenous vein graft to the left anterior descending (LAD). After a surgery time of approximately 4 h, the chest was closed, and the patient was taken to the intensive care unit. The postoperative period was uncomplicated. On the first postoperative day the patient was weaned to extubation and on the second day inotropes and vasopressors were tapered out. Echocardiographic examination before discharge disclosed a residual shunt (Qp:Qs 2.6), a recovered right ventricular function, and a persistent reduced left ventricular function (LVEF 28%) without signs of mitral valve dysfunction. Despite a residual shunt, the patient made a steady cardiovascular recovery and was transferred to a rehabilitation facility approximately 3 weeks after surgery. At the three-month follow-up, the patient was well with NYHA II. Transthoracic echocardiography showed no changes in residual shunt and left ventricular function. At the six-month follow-up, the patient is almost asymptomatic with a good exercise tolerance. The ejection fraction by the echocardiogram is 35%. He has recovered and continues to do well 6 months after the procedure (NYHA II).
|
|
|
Fig. 3. Maximum intensity (MIP) CT image of the heart in sagittal (A) and axial oblique projection (B). (A) The images show the presumed biventricular free wall rupture with the intrapericardial left-to-right shunt formation (*). The pericardium of the anterior wall (white arrow) is clearly defined, whereas the pericardium of the inferior wall (arrowheads) adjacent to the diaphragm is vague. (B) The image demonstrates the presumed LVFWR (black arrow) with connection to the volume overloaded RV. |
|
|
|
Fig. 4. Volume rendered CT image (VRT) of the heart in right oblique projection with a view of the inferior heart border. The image shows the presumed biventricular rupture communicating with separate orifices in the LV (black *) and RV (white *) through the pseudoaneurysm. |
|
|
|
Fig. 5. Coronary angiogram shows a three-vessel coronary artery disease. (A) Left coronary angiogram shows critical stenosis of LAD in the middle segment and ostial occlusion of the LCA with collateral perfusion through the LAD. (B) Right coronary angiogram shows proximal and distal critical stenosis of the right coronary artery, RD1 and RIM. |
3. Discussion
This report presents a rare clinical case of a posterior ventricular septal rupture (VSR) after subacute myocardial infarction (MI) mimicking a biventricular free wall rupture with formation of an extracardiac left-to-right shunt via pseudoaneurysm. However, in contrast to initial echocardiographic and computer tomographic suspicion, only intraoperative exploration established the challenging diagnosis of a complex postinfarction VSR, mimicking this rare mechanical defect because of its strict posterior localization within the dilated heart. In general, mechanical complications after MI include ventricular septal rupture (VSR), free wall rupture (FWR) and papillary muscle rupture (PMR). Though estimating the frequency of a cardiac rupture (CR) is difficult, it is assumed to be between 3 and 5% [1] ; [3]. In particular, the incidence of FWR occurs up to 10% of MI, as VSR and PMR have a lower incidence of < 1% and 0.5–5% [7] ; [8]. As a result, a VSR generally occurs in an early phase after MI at the sides of the softened necrotic area, as the necrotic myocardium becomes fibrotic in the long term [1]. Generally, VSR can be categorized due to their localization within the interventricular septum in anterior (66%) or posterior (34%) and morphologically as simple or complex in geometry. Corresponding to our patient, complex VSR (often basal inferoposterior) are hallmarked by irregular, serpiginous connection through the interventricular septum with intramural hematoma [1]; [3]; [13] ; [14]. In contrast, an anterior MI leads more frequently to anteroapical and simple VSR [3]. Simple VSR are characterized by a discrete defect and a direct connection across the interventricular septum at the same level on both sides [1]; [3]; [13] ; [14]. Although reperfusion therapy reduces the size of infarcted myocardium, in this context it can also promote hemorrhagic dissection or reperfusion injury, thus accelerating the onset of VSR [3] ; [9]. Consequently, the interval between MI and new onset of VSR may have been reduced from five days to one day, since the inception of revascularization procedures. Delayed postinfarction VSR, emerging after more than two weeks, is a rare event [2]; [6] ; [14]. Female sex, hypertension, first MI and advanced age (> 60 y) are considered common risk factors associated with postinfarction VSR [8]; [9] ; [14]. Notably, in 20% of patients with VSR, concomitant severe mitral regurgitation is evident [12]. Hence, the challenging task might be to distinguish these two mechanical complications. In contrast, the murmur associated with severe mitral regurgitation is loudest at the apex, often has a diastolic component, and rarely has a palpable thrill [1]. Nevertheless, auscultation of new heart sounds in the context of acute myocardial infarction should lead to further diagnostic examination. In this regard, it has been shown previously that echocardiography with the Doppler technique is recommended to assess the site and size of VSR, left and right ventricular functions, right ventricular pressure and shunt size. Two-dimensional echocardiography alone directly visualized a VSR in only 40% [12]. Although VSR with complex geometry can be visualized with additional Doppler color flow mapping, it has been described previously that particular cases are underrated, and appropriate information on the precise VSR morphology can only be derived at the time of surgical repair [13]. In this instance, a transesophageal echocardiogram (TEE) adjunct to transthoracic (TTE) imaging was performed in order to obtain more detailed information on the localization of the rupture site in order to overcome diagnostic gaps [10]. However, in our case, even echocardiography (TTE, TEE), as well as subsequent cardiac computer tomography were misleading by suspecting a biventricular free wall rupture with extracardiac left-to-right shunt in the dilated heart. Regardless of the imaging technique used, there remains a gray zone in which it is challenging to detect the appropriate site, size, and direction of mechanical defects following myocardial infarction (especially after inferior MI). In this instance, a Swan Ganz catheter might be helpful in revealing a step-up in oxygen saturation between the right atrium and pulmonary artery caused by a left–right shunt through the VSR [1]. The size of VSR can be estimated by a pulmonary-to-systemic flow ratio (Qp:Qs). We dispensed with having a left ventriculogram or a Swan Ganz catheter with respect to the risk of volume overload and two corresponding results in different non-invasive imaging techniques. Coronary angiography is often performed in order to assess coronary anatomy for concomitant revascularization. Remarkably, coronary angiographic studies highlighted the frequency and contribution of a VSR according to its culprit lesion. LAD stenosis was evident in 66% of patients with VSR, 6% had LCX stenosis, and 28% had RCA stenosis [1] ; [3]. VSR was associated with a higher incidence of single vessel disease and lacking collateral circulation [1] ; [2]. When multi-vessel disease in coronary angiography occurred, it was more frequently associated with a posterior and complex VSR leading to worse prognosis [2]; [3] ; [14]. As mortality remains high in all patients without surgical repair (78%–90%) [1]; [2]; [3] ; [6], being highest in patients with posterior VSR [13], cardiac repair is urgently required. In current European or American guidelines there is no agreement with regard to the exact timing for surgery [11] ; [13]. Indeed, early surgery might be associated with high mortality rates and high risk of residual shunts due to the complex geometry of the VSR in the weakened infarct area. Moreover, delayed surgery might allow easier septal repair after the infarct area had remodeled to a scarred tissue [13]. However, easier septal repair must be weighed against the risk of an abruptly expanding rupture site, which may result in sudden hemodynamic deterioration [11]. Despite progress in surgical techniques, mortality rate after surgical repair remains high (20–45%) [1]; [5] ; [6]. Probably, an increase in proportion of ruptures with complex geometry (especially in posterior VSR) and reduced onset might have posed a new challenge to surgeons with the still high mortality rates [2]. Therefore, challenging procedures had been developed, like percutaneous closure of the VSR with occluder devices. Recently performed trials and case reports investigated the implementation in acute or subacute setting, as a bridge to surgery approach and for closure of residual shunts after initial surgical repair [5]; [7] ; [11]. The percutaneous approach in acute postinfarction VSR, being a less invasive procedure, was associated with an overall 30-day survival rate of 35%. Higher mortality rates occurred in patients with cardiogenic shock (up to 93%) [3] ; [9]. As described above, postinfarction VSR are large in size and morphologically complex in geometry. Thus, a further increase in VSR size might occur after the initial procedure, increasing the likelihood of device dislocation [7]. Consequently, the depicted patient was transferred to the department of cardiovascular surgery for urgent closure of ventricular septal rupture, mitral valve replacement and concomitant bypass graft surgery after this case had been presented to an interdisciplinary heart team. Despite successful initial repair, residual shunts occur in 10% to 20% due to the technical difficulty of complete repair within the odd-shaped surface of the trabecular and their complex geometry with further increase in VSR size after the initial surgical repair [5]. Perioperative alteration of the mitral valve function and residual shunts are all associated with a poor postoperative outcome [3]. However, reoperation of residual shunts is associated with mortality rates of 29% [5]. Therefore, we dispensed with having a reoperation, as clinical course initially was encouraging, and left as well as right ventricular function recovered.
4. Conclusion
Although the combination of precise physical examination, echocardiography, and cardiac computer tomography is regarded as the diagnostic evaluation of choice, in particular cases these diagnostic tools are insufficient to localize the correct rupture site, size, and direction of a complex cardiac rupture (especially after inferior MI) — a distinction with implications for prognosis and surgical treatment. Solely in-situ surgical exploration, based on the interpretation of different noninvasive imaging procedures by an interdisciplinary heart team, might permit the differentiation among complex cardiac ruptures.
References
- [1] Y. Birnbaum, M.C. Fishbein, C. Blanche, R.J. Siegel; Ventricular septal rupture after acute myocardial infarction; N. Engl. J. Med., 347 (18) (Oct 31 2002), pp. 1426–1432
- [2] F.F. Cox, W.J. Morshuis, H.W. Plokker, J.C. Kelder, H.A. van Swieten, et al.; Early mortality after surgical repair of postinfarction ventricular septal rupture: importance of rupture location; Ann. Thorac. Surg., 61 (6) (Jun 1996), p. 1752,7 (discussion 1757-8)
- [3] B.S. Crenshaw, C.B. Granger, Y. Birnbaum, K.S. Pieper, D.C. Morris, et al.; Risk factors, angiographic patterns, and outcomes in patients with ventricular septal defect complicating acute myocardial infarction. GUSTO-I (global utilization of streptokinase and TPA for occluded coronary arteries) trial investigators; Circulation, 101 (1) (Jan 4-11 2000), pp. 27–32
- [4] R.G. Cummings, K.A. Reimer, R. Califf, D. Hackel, J. Boswick, et al.; Quantitative analysis of right and left ventricular infarction in the presence of postinfarction ventricular septal defect; Circulation, 77 (1) (Jan 1988), pp. 33–42
- [5] M.A. Deja, J. Szostek, K. Widenka, B. Szafron, T.J. Spyt, et al.; Post infarction ventricular septal defect — can we do better?; Eur. J. Cardiothorac. Surg., 18 (2) (Aug 2000), pp. 194–201
- [6] M. Di Summa, G.M. Actis Dato, P. Centofanti, G. Fortunato, F. Patane, et al.; Ventricular septal rupture after a myocardial infarction: clinical features and long term survival; J. Cardiovasc. Surg., 38 (6) (Dec 1997), pp. 589–593
- [7] C. Kaulfersch, I. Daehnert, G. Schuler, H. Thiele; Transcatheter closure of postinfarction ventricular septal defects; Minerva Cardioangiol., 55 (5) (Oct 2007), pp. 693–701
- [8] J. Lopez-Sendon, E.P. Gurfinkel, E. Lopez de Sa, G. Agnelli, J.M. Gore, et al.; Factors related to heart rupture in acute coronary syndromes in the global registry of acute coronary events; Eur. Heart J., 31 (12) (Jun 2010), pp. 1449–1456
- [9] V. Menon, J.G. Webb, L.D. Hillis, L.A. Sleeper, R. Abboud, et al.; Outcome and profile of ventricular septal rupture with cardiogenic shock after myocardial infarction: a report from the SHOCK trial registry. SHould we emergently revascularize occluded coronaries in cardiogenic shock?; J. Am. Coll. Cardiol., 36 (3 Suppl. A) (Sep 2000), pp. 1110–1116
- [10] T.P. Obarski, P.J. Rogers, D.L. Debaets, L.G. Murcko, M.R. Jennings; Assessment of postinfarction ventricular septal ruptures by transesophageal Doppler echocardiography; J. Am. Soc. Echocardiogr., 8 (5 Pt 1) (Sep-Oct 1995), pp. 728–734
- [11] P.T. O'Gara, F.G. Kushner, D.D. Ascheim, D.E. Casey Jr., M.K. Chung, et al.; 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines; Circulation, 127 (4) (Jan 29 2013), pp. 529–555
- [12] J.H. Smyllie, G.R. Sutherland, R. Geuskens, K. Dawkins, N. Conway, et al.; Doppler color flow mapping in the diagnosis of ventricular septal rupture and acute mitral regurgitation after myocardial infarction; J. Am. Coll. Cardiol., 15 (6) (May 1990), pp. 1449–1455
- [13] Task Force on the Management of ST-segment Elevation Acute Myocardial Infarction of the European Society of Cardiology (ESC), P.G. Steg, S.K. James, D. Atar, L.P. Badano, C. Blomstrom-Lundqvist, et al.; ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation; Eur. Heart J., 33 (20) (Oct 2012), pp. 2569–2619
- [14] O. Topaz, A.L. Taylor; Interventricular septal rupture complicating acute myocardial infarction: from pathophysiologic features to the role of invasive and noninvasive diagnostic modalities in current management; Am. J. Med., 93 (6) (Dec 1992), pp. 683–688
Document information
Published on 19/05/17
Submitted on 19/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?