Summary
Background/Objective
The Knowledge Program (TKP) allows prospective data collection during routine clinical practice. The aim of this study was to evaluate the efficacy and feasibility of TKP for capturing and monitoring health status measures in patients undergoing lateral internal sphincterotomy (LIS).
Methods
TKP data of patients undergoing LIS from December 2008 to May 2013 were retrieved. Health status measures including the Cleveland Global Quality of Life (CGQL), European Quality of Life Index (EQ-5D), Fecal Incontinence Severity Index (FISI), anorectal pain scores, and satisfaction questions were evaluated in the study.
Results
A total of 500 patients underwent LIS within the study period. Overall patient numbers responding to the health status measures in the pre- and postoperative period were as follows: CGQL: 112 preoperatively, 53 postoperatively; EQ-5D: 112 preoperatively, 55 postoperatively; FISI: 102 preoperatively, 30 postoperatively; and anorectal pain score: 107 preoperatively, 45 postoperatively. Among the responders, the number of patients who completed the health status measures both pre- and postoperatively was as follows: EQ-5D: 31, CGQL: 28, anorectal pain: 24, and FISI: 15. A total of 30 patients completed postoperative satisfaction and recommendation questions. Postoperative earliest (p = 0.02) and most recent (p = 0.01) anorectal pain visual analog scores were significantly lower than the preoperative measurements. The earliest postoperative EQ-5D scores were significantly higher than their preoperative values (p = 0.02). The majority of patients who completed the surveys said they were satisfied (70% and 67%) and would recommended (73% and 70%) LIS to others undergoing postoperative earliest and most recent follow up.
Conclusion
LIS reduces anorectal pain without worsening quality of life. TKP captures information directly from patients and records it to a database which may reduce the risk of information loss or alteration.
Keywords
chronic anal fissure;lateral internal sphincterotomy;perioperative pain;quality of life;The Knowledge Program
1. Introduction
Computer technology has been used in patient care, education, and monitoring for years.1 Information related to appointments, office visits, diagnostic tests, operations, discharge summaries, and follow up is recorded in computer-based systems. Information necessary for patient care is usually obtained by a nurse or a physician and recorded for further use. Patient data can also be used for clinical research following institutional review board (IRB) approval. Some high volume centers, including our institution, have additional IRB-approved databases that are maintained prospectively under the guidance of professional staff.2 Correct, secure, and reliable data storage is the key component of a successfully maintained database. In addition to the clinical information, health status measures including patient-reported functional outcomes and disease specific quality of life (QOL) analyses following treatment are recorded in databases. Traditionally, QOL studies have been performed through patient self-report questionnaires printed on paper forms. Recently, electronic questionnaires have been applied with the help of advanced technology.3 However; there are limited studies about the value and practicality of the electronic data collection systems for monitoring patients' perioperative health status. At our outpatient clinic, health status measures have been collected using a novel system “The Knowledge Program” (TKP), which is a type of software used for prospective data collection and monitoring during routine clinical visits.4 The system communicates wirelessly between tablet computers and the electronic TKP database. Patients use touchscreen computers to answer questions regarding their health status measures, and the electronic database keeps data secure and classifies the data to be used for patient care and research.
Lateral internal sphincterotomy (LIS) is usually performed as the definitive treatment for chronic anal fissure when medical therapy fails.5 In this study, we aimed to evaluate the efficacy and feasibility of TKP for gathering and monitoring health status measures in patients undergoing LIS for chronic anal fissure.
2. Methods
After obtaining IRB approval, data recorded in TKP database related to the patients who underwent LIS for chronic anal fissure from December 2008 to May 2013 were reviewed. Patients who underwent concurrent abdominal and/or other anorectal procedures were excluded from the study. Health status measures including validated questionnaires such as the Cleveland Global Quality of Life (CGQL), European QOL Index (EQ-5D), Fecal Incontinence Severity Index (FISI), anorectal pain scores, and satisfaction questions were used. Patients who had answered TKP questionnaires both before and after surgery were included in the analysis for evaluating perioperative monitoring of the health status measures. For continued perioperative monitoring, the preoperative values were compared to both earliest and most recent postoperative values.
2.1. Data capture process within TKP
TKP software is designed for data monitoring in routine clinical practice. Heath status measures are gathered using TKP in accordance with an IRB-approved protocol. When patients check-in at the outpatient clinic, they complete the electronic questionnaires on touch-screen tablet computers that are connected wirelessly to the electronic TKP database. The software is structured to calculate questionnaire scores automatically and directly upload the electronic database. The database is password-protected and IRB approval is necessary for every specific project that requires retrieval of the patient information from TKP database. Detailed information about TKP set-up was documented previously.4
2.2. QOL and pain measures
The CGQL score includes three items: current QOL, current health, and current level of energy, each self-reported on a scale of 0 to 10 (0 = worst, 10 = best). The CGQL utility score is calculated by dividing the total of the aforementioned parameters by 30 (0 = worst, 1 = best).6 The European QOL Index (EQ-5D) is a generic instrument for describing and evaluating health and is based on a descriptive system that defines health in terms of five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. This validated questionnaire has its own visual analog score questioning the respondents self-rated health. The range of the EQ-5D score is between 0.1 = worst and 1 = best.7 Anorectal functions were assessed using the FISI. The FISI score ranges from 0 to 61, where 0 = best and 61 = worst.8 Anorectal pain was evaluated with a visual analog scale scored from 0 to 10 (0 = best and 10 = worst). Anorectal pain was scored from 1 (no pain) to 10 (worst pain). Patient satisfaction was assessed by asking patients two questions: (1). Are you satisfied with your surgery? and (2). Would you recommend your surgery to others? Responses were reported on a scale from 1 to 5 (1 = not at all, 5 = extremely).
2.3. Statistics
Comparisons of the groups were performed using the Wilcoxon rank-sum test. Parametric data were reported as median and interquartile range (IQR) and nonparametric data as numbers except where otherwise noted. A p value <0.05 was considered to be significant.
3. Results
A total of 500 (272 male) patients underwent LIS within the study period. Overall patient response numbers to the health status measures in the pre- and postoperative period were as follows: CGQL: 112 preoperatively, 53 postoperatively; EQ-5D: 112 preoperatively, 55 postoperatively; FISI: 102 preoperatively, 30 postoperatively; and anorectal pain score: 107 preoperatively, 45 postoperatively. Among the responders, the number of patients who completed the health status measures both pre- and postoperatively was as follows: EQ-5D: 31, CGQL: 28, anorectal pain: 24, and FISI: 15. Thirty patients completed postoperative satisfaction and recommendation questions.
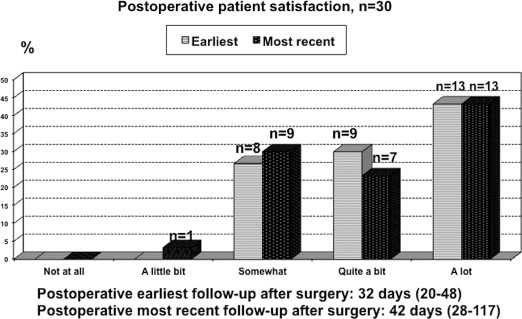
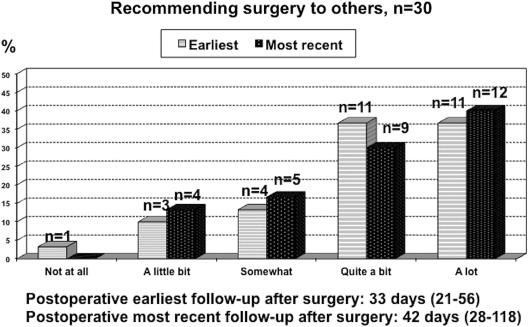
Postoperative earliest (p = 0.16) and most recent (p = 0.2) CGQL scores did not differ significantly from their preoperative values. However, the earliest postoperative EQ-5D quality of life scores were significantly higher than their preoperative values (0.83 vs. 0.80, p = 0.02). Although they were not significant, postoperative FISI scores improved gradually and this change became more obvious at the most recent follow up (p = 0.054). Postoperative earliest (p = 0.02) and most recent (p = 0.01) anorectal pain visual analog scores were significantly lower than their preoperative measurements ( Table 1). The exact days of preoperative, postoperative earliest, and most recent follow up are presented for every value individually in Table 1. The majority of patients who completed the surveys said they were satisfied (n = 21, 70% vs. n = 20, 67%) and would recommended (n = 22, 73% vs. n = 21, 70%) LIS to others in postoperative earliest and most recent follow up, respectively ( Figure 1 ; Figure 2). Among the patients who responded to the health status measures pre-and postoperatively, 18 patients had multiple postoperative office visits due to persistent complaints including anal/perianal pain (n = 6), bleeding (n = 6), itching (n = 2), or other general medical problems (n = 4).
| Preoperative | Postoperative | ||
|---|---|---|---|
| Earliest | Most recent | ||
| GGQL (n = 28)a | 0.6 (0.42–0.73) | 0.68 (0.56–0.73) | 0.68 (0.52–0.74) |
| Time to/after surgery (d) | 20 (12–44) | 37 (22–61) | 82 (29–209) |
| Overall responders, nb | 112 | 53 | |
| p | 0.16c | 0.20d | |
| EQ-5D (n = 31)a | 0.80 (0.46–0.83) | 0.83 (0.77–0.86) | 0.83 (0.77–0.84) |
| Time to/after surgery (d) | 15 (9–29) | 33 (20–52) | 90 (34–188) |
| Overall responders, nb | 112 | 55 | |
| p | 0.02c | 0.17d | |
| FISI (n = 15)a | 12 (7–30.5) | 8 (0–16) | 0 (0–12) |
| Time to/after surgery (d) | 15 (9–29) | 34 (24–91) | 92 (27–560) |
| Overall responders, nb | 102 | 30 | |
| p | 0.10c | 0.054d | |
| Anorectal pain (n = 24)a | 5 (3.75–7.25) | 3 (1–5.25) | 3 (1–5.25) |
| Time to/after surgery (d) | 15 (7–26) | 34 (24–51) | 70 (29–300) |
| Overall responders, nb | 107 | 45 | |
| p | 0.02c | 0.013d | |
CGQL = Cleveland Global Quality of Life; EQ-5D = European Quality of Life Index; FISI = Fecal Incontinence Severity Index.
a. Number of patients who completed The Knowledge Program questionnaires, both pre- and postoperatively, during office visits.
b. Overall number of patients answering the questionnaires within the described time period.
c. Preoperative versus postoperative earliest.
d. Preoperative versus postoperative most recent.
|
|
|
Figure 1. Patient satisfaction after lateral internal sphincterotomy. |
|
|
|
Figure 2. Patient recommendation after lateral internal sphincterotomy. |
4. Discussion
The cohort of patients involved in this study was undergoing LIS for chronic anal fissure at a tertiary colorectal unit. Our results shows that LIS relieves anorectal pain and provides high patient satisfaction without worsening QOL during the perioperative period. Although there are various treatment alternatives including Botox injection, chemical sphincterotomy and fissurectomy, LIS is still the gold standard intervention for chronic anal fissure.9 The beneficial effects of LIS on QOL have been documented in prospective studies,5 ; 10 and Ortiz et al5 reported that improvements in QOL can be observed 6 months after LIS. The EQ-5D index showed a significant QOL improvement in short-term postoperative period in our patients. LIS can improve QOL by reducing anorectal pain. However, QOL can also be affected by other patient related and environmental factors.8 Postoperative complications may worsen QOL after LIS. Patients with anal continence issues tend to have a poorer QOL than those with normal continence after LIS.5 Long-term outcomes of patients undergoing LIS at our institution were presented in greater detail in a previous retrospective study which reports good postoperative functional scores and high patient satisfaction.11 Although chronic anal fissure is a “prolonged” disease requiring surgical treatment after failed medical therapy, pathophysiology and treatment alternatives are less complex than those used for other benign chronic colorectal diseases such as Crohns disease or ulcerative colitis. LIS is a simple and definitive treatment option that is associated with low operative complications.12 Therefore; this study was designed for patients who underwent LIS for chronic anal fissure to evaluate the inherent value of TKP as means of gathering and monitoring health status measures during the perioperative period.
Utilization of TKP for data collection is the novel component of the current study. Difficulties associated with outcome research such as cost, the necessity of educated research professionals, and overwhelming workloads have forced researchers to create new methods of facilitating clinical studies. TKP, which was initially developed in the Cleveland Clinic Neurological Institute, was adapted for use in our outpatient colorectal surgery clinic 5 years ago.4 ; 13 The tablets , wireless technology, and structured software programs, tremendously simplify the use of electronic questionnaires during routine clinical practice.4 TKP may facilitate clinical outcome research in many ways. Firstly; the tablet technology offers an opportunity to utilize the time patients spend in the waiting area for the purpose of data collection. TKP also actively includes patients in the scientific assessment of their care. This involvement may motivate patients to be more compliant throughout the treatment process. Real-time scoring of health status measures enables practitioners to use these scales in routine clinical practice. We believe the integration of health status measures into clinical practice will improve the quality of patient care and increase the response rates of questionnaires.4 Secondly; TKP may reduce the requirement of manpower for data collection and storage for research. Additionally, patient confidentiality is better protected, since questionnaires are answered and transferred directly to the database without the need for human interaction. This also reduces the risk of recall bias when compared to paper based questionnaires evaluating postoperative health status and outcomes retrospectively. Reduced human involvement and paperwork may also reduce unintentional mistakes that occur during the data gathering processes. Thirdly; data collection with a touch screen tablet may take less time than completing paper-based questionnaires.4 In addition to the perioperative benefits of TKP usage, current internet technology and advanced software programs can be used to monitor homecare and the long-term follow-up outcomes of therapies.1 We believe this would be highly beneficial to academic institutions.
A limitation of this study is biased due to patients self-selection to complete TKP. Considering the overall number of patients undergoing LIS, the number of responders was relatively low. It is possible that healthier individuals might have more often responded to health status measures and completed TKP. Nevertheless, we believe that the design of the perioperative monitoring minimizes selection bias in this study. In general, patients undergoing LIS have none or only one postoperative office visit unless there is a complication. However, the majority of patients who were included in the perioperative monitoring analysis had multiple postoperative office visits which were related to their postoperative complaints or extra medical problems. These patients were likely not to be the patients who had the best outcomes after surgery. Moreover, the data of the current study were captured during ordinary outpatient visits with no additional explanation for any proposed study. The low response rate was another limitation of the study. TKP has been incorporated into the clinical visits slowly and tablet computers could not have been delivered to all patients initially. Among patients who received a tablet computer, some might have been uncomfortable using and completing TKP. Providing short and precise instructions for completing TKP at check-in followed by nursing staff inquiry could increase the compliance rate. During the study period, newer and more user-friendly tablets have been added to TKP system. Our outpatient nursing staff has been trained to be more proactive in checking on patients to make sure TKP questionnaires are completed before office visits.
In conclusion, LIS for chronic anal fissure reduces anorectal pain without worsening QOL. TKP captures information directly from patients and may reduce the risk of information loss or alteration in survey studies.
Acknowledgments
This study was supported by the Ed and Joey Story Endowed Chair in Colorectal Surgery.
References
- 1 T.E. Belda; Computers in patient education and monitoring; Respir Care, 49 (2004), pp. 480–488
- 2 E. Manilich, J.D. Vogel, R.P. Kiran, J.M. Church, D. Seyidova-Khoshknabi, F.H. Remzi; Key factors associated with postoperative complications in patients undergoing colorectal surgery; Dis Colon Rectum, 56 (2013), pp. 64–71
- 3 G. Velikova, E.P. Wright, A.B. Smith, et al.; Automated collection of quality-of-life data: a comparison of paper and computer touch-screen questionnaires; J Clin Oncol, 17 (1999), pp. 998–1007
- 4 B. Gurland, P.C. Alves-Ferreira, T. Sobol, R.P. Kiran; Using technology to improve data capture and integration of patient-reported outcomes into clinical care: pilot results in a busy colorectal unit; Dis Colon Rectum, 53 (2010), pp. 1168–1175
- 5 H. Ortiz, J. Marzo, P. Armendariz, M. De Miguel; Quality of life assessment in patients with chronic anal fissure after lateral internal sphincterotomy; Br J Surg, 92 (2005), pp. 881–885
- 6 V.W. Fazio, M.G. O'Riordain, I.C. Lavery, et al.; Long-term functional outcome and quality of life after stapled restorative proctocolectomy; Ann Surg, 230 (1999), pp. 575–586
- 7 The EuroQol group; EuroQol: a new facility for the measurement of health-related quality of life; Health Policy, 16 (1990), pp. 199–208
- 8 T.H. Rockwood, J.M. Church, J.W. Fleshman, et al.; Patient and surgeon ranking of the severity of symptoms associated with fecal incontinence: the fecal incontinence severity index; Dis Colon Rectum, 42 (1999), pp. 1525–1532
- 9 G. Kiyak, B. Korukluoğlu, A. Kuşdemir, I.C. Sişman, E. Ergül; Results of lateral internal sphincterotomy with open technique for chronic anal fissure: evaluation of complications, symptom relief, and incontinence with long-term follow-up; Dig Dis Sci, 54 (2009), pp. 2220–2224
- 10 N. Griffin, A.G. Acheson, P. Tung, C. Sheard, C. Glazebrook, J.H. Scholefield; Quality of life in patients with chronic anal fissure; Colorectal Dis, 6 (2004), pp. 39–44
- 11 S. Casillas, T.L. Hull, M. Zutshi, R. Trzcinski, J.F. Bast, M. Xu; Incontinence after a lateral internal sphincterotomy: are we underestimating it?; Dis Colon Rectum, 48 (2005), pp. 1193–1199
- 12 S.R. Mousavi, M. Sharifi, Z. Mehdikhah; A comparison between the results of fissurectomy and lateral internal sphincterotomy in the surgical management of chronic anal fissure; J Gastrointest Surg, 13 (2009), pp. 1279–1282
- 13 I. Katzan, M. Speck, C. Dopler, et al.; The Knowledge Program: an innovative, comprehensive electronic data capture system and warehouse; AMIA Annu Symp Proc, 2011 (2011), pp. 683–692
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?