Abstract
The conceptualization of the Household/Neighborhood Model for skilled nursing facilities began in 1987 at Evergreen Retirement Community in Oshkosh, WI, USA in the search for the “perfect” nursing home. Being able to see perfection required being freed from the mental constraints of regulations, reimbursement systems, and existing staff training programs so that visionary thinking was possible. Conceptualization was followed by a pilot project to test various aspects of the vision. The result was (1) a management philosophy built on Continuous Quality Improvement, (2) a team-based organization structure, (3) cross-functional staff roles, (4) social-model activity programming, and (5) a residential style physical setting that won strong support from the State of Wisconsin. With this support, we had the opportunity to open in 1997 the first full-scale model of a Household/Neighborhood in the United States based upon providing “resident and relationship centered services and care”. The model was validated through a year-long evaluative research study. In 2004 we opened a second full-scale model incorporating significant improvements identified through experience. The opportunity to further develop the model has been provided through its adoption in China by China Senior Care, which will open their first facility in 2014.
Keywords
Aging ; Environment ; Design ; Long-term ; Care
1. Introduction
The objectives of this paper are to describe the: (1) drivers behind the conceptualization of the Household/Neighborhood Model skilled nursing facility at Evergreen Retirement Community, Oshkosh, Wisconsin; (2) steps taken to develop the concept, including a pilot project; (3) planning for a full-size household/neighborhood; (4) research during the implementation of the Continuous Quality Improvement management philosophy; (5) collaboration with the State of Wisconsin to allow construction of the first full-size neighborhood; (6) transformation of the organization structure to support the model; (7) research evaluation of the first full-size neighborhood; (8) planning and construction of the second household/neighborhood; and (9) utilization and further development of the model for use in China. This paper is a critical reflective appraisal of a participatory action research project where the physical setting, organization, staffing and operations were significantly changed to create a new paradigm of long-term care.
2. Drivers behind conceptualization of Household/Neighborhood
2.1. Early history of evergreen
The idea of a continuing care retirement community in Oshkosh, Wisconsin with both independent living and nursing home accommodations came from a successful local industrialist and his wife. They were willing to expend a significant portion of their personal funds to make it a reality with the objective of becoming residents. As a sponsoring organization for this non-profit, risk-taking endeavor they recruited the Wisconsin Conference of the United Methodist Church.
Evergreen opened in 1967 with 92 apartments for independent elders and a 50 resident nursing home providing both skilled and intermediate care. The first of 18 single-family ranch-style homes and 2 duplexes were built beginning in 1970. In 1974 a 3-story addition with 56 skilled and intermediate nursing care accommodations and 20 apartments was opened. I was hired as CEO in 1976 when the first CEO retired.
2.2. Background of author
My undergraduate education resulted in two Bachelor׳s degrees, Architectural Engineering and Business through a 5-year program, plus an extra year of liberal arts studies through a scholarship to broaden the education of engineers. Upon graduation in 1962, I worked as an engineer for an industrial corporation. My employer provided me the opportunity to do some volunteer service with the building committee of a non-profit continuing care retirement community. Through this experience I recognized that a career in long-term care administration would provide the means to use the breadth of my education and my desire to serve people.
In 1966 I took the position of assistant administrator at a non-profit, long-term care facility. I quickly realized that I needed more education in order to be successful in this new field. In 1968 I began graduate school and received a Master׳s degree in Studies in Aging in 1970. During the next 6 years prior to going to Evergreen, I had varied work experience in long-term care, the last being the owner׳s representative to guide the design and construction of a new skilled nursing facility.
2.3. Evergreen culture
The above history and background are relevant to the development of the Household/Neighborhood Model since this creative endeavor was ultimately the product of the forward thinking, risk-taking perspective of the Rowland׳s and my unique education, career path and leadership philosophy. This combination eventually resulted in the development of an organization culture that thrived on innovation and cutting-edge thinking in response to external factors that evolved over time.
The first opportunity to utilize the combination of my knowledge of both building design and studies in aging occurred in the early 1980s. During that time Evergreen identified the need for accommodations specifically for independent elders who wanted a living environment that would maximize their independence, foster relationships with neighbors, and offer equity ownership. I provided the leadership to develop the design for groupings of eight attached homes that accomplished the above objectives. The philanthropist supported what was clearly a risk-taking endeavor due to the uniqueness of both the building design and the financing mechanism. Because of his encouragement, in 1984 the first building was opened and filled quickly. As a result, over the next few years, 4 and 1/2 more of these buildings were built.
While this project was not for residents requiring skilled nursing, who are the focus of this paper, the objective was to provide a living environment offering “resident and relationship centered” services to independent residents. The success of this endeavor encouraged the Evergreen governing board to support, over many years, the risk-taking innovation required to provide high quality life experiences for residents needing “resident and relationship centered” skilled nursing care and services.
2.4. Impetus for new nursing home
An external driver for the development of the Household/Neighborhood Model was the opening in the early 1980s of a large addition, with all private rooms, to a nearby nursing home. This put Evergreen at a significant disadvantage in attracting admissions to vacant accommodations in our nursing home since most were semi-private rooms with side-by-side beds. In 1983 the decision was made to create more private rooms with either an addition to our traditional nursing home or a new physical setting. The governing board decided to begin planning a replacement nursing home since the site plan made expanding the current building difficult and many resident toilet rooms could not be remodeled to make them handicapped accessible in accord with federal government regulations.
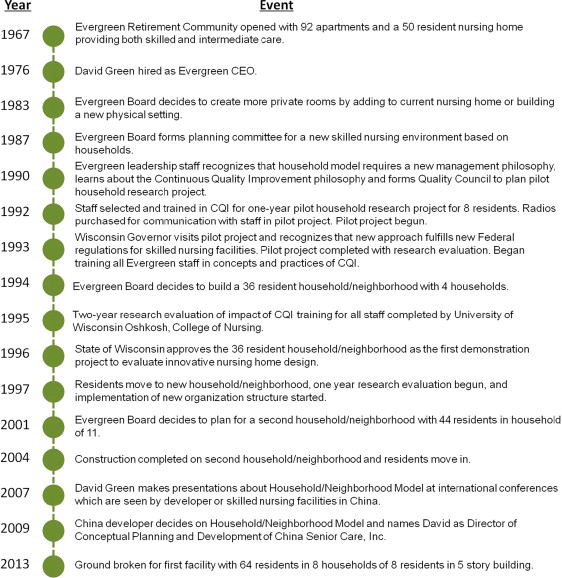
Figure 1 shows a timeline of Evergreen Household/Neighborhood Model development.
|
|
|
Figure 1. Evergreen Household/Neighborhood Model development timeline. |
3. Conceptualizing the household
3.1. Planning process for a new skilled nursing environment
Early in 1987, the governing board formed a planning committee for a new skilled nursing environment; the committee included representatives of all key stakeholder groups – residents, direct-care and support staff, management staff and board members. A nationally recognized consultant with significant experience in nursing home design was retained to facilitate the 9-month planning process which included monthly day-long meetings of the committee.
The first step in planning was to define a vision of how we wanted life to be for the residents in the “perfect” nursing home. Thus we began by defining the desired “end” to be achieved, a positive subject, rather than focusing on the problems we needed to overcome, including regulations and finances, which are inherently negative in the field of long-term care. By beginning with the vision, all participants in the planning process were able to contribute to the creative dialog since they could identify the life experiences desired in a skilled nursing environment.
3.2. Rationale for household
A key aspect of the vision defined by the planning committee was that the setting should look and feel like “home”, which would be very different from the hospital-like nursing home designs used at that time. During my graduate school studies, I learned of research done in the 1960s at the Philadelphia Geriatric Center which supported the creation of small households. The researcher3 found that when each resident had a clearly defined private space adjoining a shared space where they could associate with a small group of residents, and adjacent public space for interacting with the larger community, the residents were much more likely to exhibit normal social and exploratory behaviors. The small groupings of residents, each with designated private space, provided the conceptual foundation of the “household” for our new building design.
3.3. Size of household
The next aspect of the vision to be determined was the size of each household, which could be based on a variety of factors including staffing patterns, size of the building, or the dynamics of the social grouping. Evergreen chose staffing patterns with the objective of having one primary care giver in each household during waking hours. This staff member, designated Resident Assistant (RA) rather than nursing assistant, would have the primary responsibility for the household during one shift, but would be assisted as necessary by a “buddy” RA from the adjoining nursing unit and by the unit nurse.
To determine the number of residents one staff member could reasonably serve, all of the tasks to be managed by a household Resident Assistant were identified and the time required for each task was estimated. By adding up the projected task times, the initial conclusion was that one RA would be needed for 6 residents.
We decided that the only way to verify this conclusion was to create a pilot household to test our assumptions. We were fortunate to have a small separated area of the existing nursing home where we could create a household with accommodations for 8 residents. While 8 is more residents than the initial calculations indicated, the space provided the opportunity to operationally determine the accuracy of the estimate.
3.4. Elements of the pilot household
In the pilot project area, the resident rooms surrounded an open space that was remodeled to provide a living and dining area for the 8 residents, a staff work area for documentation and medications, a kitchenette for final meal preparation and snacks, a laundry room with a washer and dryer for personal clothes, a staff toilet, a storage closet for activity supplies, and a storage area for each resident with supplies needed for personal care.
A key objective in designing the household was to have all the resources required by the Resident Assistants close to the point-of-use to minimize the RA travel time. This was a significant departure from the design of the traditional nursing home where were all of the resources are grouped around the nurse׳s station for the convenience of the nurses.
3.5. Staffing the pilot household
An important decision in the success of the pilot project was the process for selecting the staff members. The number of staff on the team included all who would have contact with the household residents during the project. All 27 persons involved were invited to volunteer because of their work attitudes and history. Therefore, everyone was enthusiastic about the challenges and opportunities the project offered. All but one fulfilled their commitment for the one-year duration of the project (planning and training time preceded this).
Another important decision was not to include a manager on the team. This was done so that the team would be guided by the diverse and collective perspectives of all the members rather than having the possibility that one member could have inordinate influence. Therefore, the team was “self-directed” with trained co-facilitators selected from the team members. The facilitators kept management informed about project progress and obtained answers to questions from the project team by communicating through a member of senior management that served as a liaison to the team.
3.6. Preparation of the pilot household project team
In 1990 prior to selecting the household team, Evergreen leadership learned about the management philosophy of Continuous Quality Improvement (CQI) which was beginning to be adopted by USA industry as a replacement for the traditional philosophy of “direct and inspect”. The CQI philosophy is expressed through a team-based organization structure where: (1) the unique knowledge and experience of each team member is identified and developed, (2) the collective knowledge and commitment of all the team members determines the capability of the team, and (3) operational decisions are made by the team guided by the organization values. The CQI philosophy was recognized as the necessary foundation for training the household team.
To guide us though the formation and implementation of this new management philosophy we retained as a consultant a nurse with experience assisting hospitals begin the adoption of CQI. Since Evergreen was the first long-term care organization in the USA to both develop the household model and incorporate the CQI philosophy we had to look outside our field for assistance. The consultant guided us to create a leadership planning group we called a Quality Council which included 5 leadership staff (including the CEO) and 5 front-line staff, all from different disciplines, plus a resident. To have the CEO as a Council member with a vote equal to the vote of any other member was essential in order to show strong support for what would eventually be a radical transformation of the entire organization.
The Quality Council developed a 30 h CQI training program for the household project team that included the following content: (1) Evergreen׳s values, vision and mission statements; (2) core concepts of CQI; (3) interpersonal skills; (4) decision-making skills; (5) communication skills; (6) defining the customer; (7) role of project team; (8) empowering staff and residents; (9) effective team process; (10) problem identification; (11) problem solving; (12) CQI tools; (13) costs of quality; and (14) requirements for team excellence.
3.7. Impact of household design on operations
During the year-long household pilot project (1992–93), the decentralization to the household of the supplies and equipment used by the Resident Assistants proved to be a powerful means for improving the productivity of the RAs. The resulting reduction in walking: (1) provided time to develop relationships with the residents, which are critical to resident and relationship centered services and care; (2) enhanced the quality of the work life for the RA by demonstrating the support of management for this position; and (3) gave them time for additional “home-making” tasks. These tasks included washing residents personal clothes to avoid lost or misplaced items, assisting with resident interest activities, doing some housekeeping (i.e., keeping resident rooms neat, and maintaining order and cleanliness of shared spaces), setting the table before meals, serving the meals (food was delivered in bulk to maximize the opportunity for resident choice), and washing dishes in the household dishwasher (some residents need special eating utensils because of disabilities so keeping the utensils in the household assured they were always available).
3.8. Relationship development
The importance of staff developing personal relationships with residents cannot be overstated since the relationship between residents and staff may be the greatest determinate of the resident׳s quality of life. For the household to reflect the best of what “home” means to each resident, every task done by a staff member that involves interaction with a resident must be viewed by the staff member as an opportunity to further the development of a positive, meaningful relationship with the resident. Relationship development needs to be regarded by all staff as equally important with properly completing the tasks.
Another important finding of the pilot project was that one Resident Assistant could normally meet the needs of 8 residents since most tasks took less time than projected based upon the estimates from a traditional nursing unit (6 residents). The exceptions were during emergencies such as falls, when specialized care by a nurse was required, or when transfers from one location to another (sometimes using portable lift devices) required an additional staff member (a nurse or Resident Assistant) to assist. Since these persons come from outside the household, the need for an efficient way for the household RA to communicate with them was required.
3.9. Need for communication devices
During the planning of the household pilot project, the need for the household Resident Assistant to have a means for easily and quickly communicating with the “buddy” RA and the unit nurse became evident. With this clear understanding of our need, we were able to find a manufacturer that was developing personal radios for use in hospitals. Evergreen became their first long-term care customer and three radios were purchased for the household project.
After the staff in these three positions experienced the benefits of the radios, all the direct care staff at Evergreen wanted them. Since we were the manufacturer׳s “beta-site” for developing this product for long-term care settings, such an arrangement became financially feasible. As the first long-term care facility in the USA using personal communication devices, we continued to work with the manufacturer for 4 years to improve the reliability, size and performance of the product. When the desired product performance could not be achieved, we searched for other types of communication devices and found what was needed in an in-house cellular phone system which had been recently developed.
Our experience with personal communication devices demonstrated that providing the “high-touch” living environment of “home” for residents in an efficient manner requires “high-tech” solutions. Staff quickly recognized that personal wireless communication devices are absolutely essential for resident and relationship centered services and care.
3.10. Household pilot project evaluation
To systematically determine how the 8 residents, their families and the 27 staff involved felt about the pilot household, a researcher4 was retained to evaluate their responses to this new living environment. Because the resident sample of 8 was very small, quantitative research was not appropriate. Through periodic interviews during the year of operation, the research determined that all three groups had very positive responses to this radically different approach to skilled nursing facility design and operations. The overall evaluation was that every nursing home resident should have the opportunity to live in this kind of setting.
3.11. Examples of household impact on residents
The household experience positively impacted all of the residents to some degree, but the experience of one stands out. Prior to moving to the household, the resident had been unsociable, uncooperative, uninvolved, and nonverbal. Initially she would not venture beyond the entry to her room. Before long she moved further into the shared area until her favorite spot was at the dining table. Her regular involvements included setting the table for meals and making sure the needs of other residents were met. She even began to talk.
She died near the end of the project and a memorial service was held for her in the household. Everyone attending the service expressed gratitude for how this loner had become a friend of all during the relatively brief time she lived in this new setting. Obviously, the new environment was transformative for her.
We also learned that dining in small “family” groups had a positive impact on behavior during meals and on food consumption. Socialization around the table increased as did resident assertiveness with each other regarding what the group considered inappropriate conversation during meals; the amount of food eaten increased, and the quantity of food dropped on the floor greatly decreased, perhaps because the residents regarded the household as their home.
4. Planning full-size household/neighborhood
4.1. Utilizing the knowledge from household pilot
The success of the household pilot project made clear the need: (1) to replace the current skilled nursing facility with one based on the household concept, and (2) for the entire organization to adopt the CQI team-based management philosophy.
4.2. Characteristics of first household/neighborhood
The governing board decided in 1994 to build the first phase of a replacement skilled nursing environment, a 36 resident neighborhood with four households of 9 residents (1/3rd the total 108 residents). The number of residents per household was increased from the 8 in the pilot household because each neighborhood would have a “float” Resident Assistant (RA) on each shift that would assist the household RAs like the “buddy” RA in the pilot project. The significant improvement in the efficiency of the household RA through the placement of household resources near the point-of-use was also a factor in deciding to have 9 residents in each household.
4.3. Training all Evergreen staff for CQI
While the household project team was trained for CQI by the consultant, following the completion of the household research project, a staff member who recently received a Master׳s degree in Nursing Administration with an emphasis on quality was prepared by the consultant to provide this training for the 250 other staff members, which took 2 years. The staff was trained in groups of about 30 that were intentionally multi-disciplinary and multi-level, including the CEO and all other management staff. Having an on-staff trainer was essential in order for the 30 h of training of all staff to be financially feasible. After the initial training, only one annual group was necessary to train all new staff.
At the same time all the staff was being trained for teams, team facilitators from all areas of the organization were being trained by the staff trainer. Having a qualified facilitator is critical to the successful functioning of each team. In order that the facilitator focuses on guiding the team process and not on the issues being addressed by the team, having a facilitator without a vested interest in the issues being addressed is important.
4.4. Effective teams and their use
In addition to a qualified facilitator, each team needs to have: (1) a defined goal; (2) the time available to complete the assigned responsibility; (3) clarity about the resources available to complete their work; and (4) shared ground rules developed by the members to guide the team process including decision-making and member involvement on the team. The membership on the team, goal, time frame, resources, and the facilitator are all defined by senior management which considers the needs of the organization from a broad perspective. The ground rules must be developed by the team so they are unanimously supported by the members.
On an effective team, each member has a clearly defined role that makes their presence on the team essential for the team to make decisions based on the consideration of all options and the implications (pros and cons) of each option. Each team member understands the need to respect the input provided by the other members since they have learned that the best decisions are made when all perspectives are adequately considered. Another characteristic of effective teams is the mutual trust that all the members of the team will follow through on the commitments they have made.
As all the Evergreen staff was progressively trained for participation on teams, the use of teams throughout the organization was feasible and increased over time. The focus of the teams varied. Some teams were on-going, dealing with subjects such as infection control that require continual monitoring and improvements. The membership of on-going teams systematically rotates on and off over time. Other teams addressed a single project so had a limited life. If the project was improving an operational process, the members were selected as representatives from all the stakeholder groups impacted by the process.
5. Research during implementation of CQI
5.1. Determining impact of implementing CQI
Since the implementation of CQI would change the philosophy, structure and culture of Evergreen, this provided an opportunity to evaluate the impact of radical organization transformation on (1) the quality of care and services provided, and (2) the resident׳s quality of life. Because Evergreen was a pioneer in long-term care in the adoption of CQI as a management philosophy, between June 1993 and June 1995 (following completion of the household research project) representatives of the College of Nursing at the University of Wisconsin Oshkosh (UWO)5 undertook the first systematic research of the results. During the two-years of research, all the staff was receiving the CQI training described above and project teams were being formed to address improvement opportunities identified by staff as part of the training.
The objectives of the College of Nursing research were to identify the changes in the: (1) organization culture, policies and services; (2) social climate, including resident and staff cohesion, and resident conflict, influence, order and physical comfort; and (3) the resident׳s quality of life as measured by resident satisfaction, health, and functional status.
Based on the work of a primary developer of the Continuous Quality Improvement philosophy and methods,6 implementing CQI will, over time: (1) increase the value that staff place on quality, (2) help them to see other staff members as well as the residents and their families as customers, (3) empower residents and staff to actively participate in decisions that impact them, (4) provide operational processes that make staff more productive, and (5) encourage management to function as leaders. The CQI philosophy creates an organization culture that is customer focused and process oriented.
5.2. Research findings
The findings related to the above objectives during the research time frame were generally not positive. This became understandable as we progressively recognized that CQI is a radical departure from the way things had been done requiring substantial new expectations for staff. Staff must move from a functionally divided structure that is rigid and emphasizes conformance to authority, to a process oriented structure built on multiple collaborative relationships. Many staff was skeptical about the goals, and experienced uncertainty and confusion as they learned new jobs and roles. Some management team members were frustrated by the slow speed of the transformation and issues encountered with employee morale.
We learned that change in culture is difficult, takes time, and demands a long-term commitment from management. The desired culture is one in which staff: (1) take pride, (2) see the meaning of the work each member does, (3) value and strive to please all customers (residents, families, other staff), and (4) understand that poor quality is usually the result of the system and not individual staff members. For this new culture to exist requires an environment of trust, which can only develop over time with: (1) consistent leadership behaviors, (2) meaningful empowerment of staff through participation in decision-making which impacts them, (3) mutual support and interaction among individuals in the work setting, and (4) decreased control by management accompanied by appropriate means of accountability.
Evergreen learned that the process for implementation of the culture must provide: (1) time for people to adjust to the change, (2) organizational support for the change, (3) substantive education of both management and other staff about CQI, (4) a pilot project where the staff can apply and see applied the principles and practices of CQI, (5) organization communication about the rationale behind and the change process, and (6) the revision of performance review and recognitions systems to emphasize teamwork. Evergreen leadership provided all of the above, which ultimately resulted in the full implementation of the CQI philosophy in 2004 with the expected positive results.
We also learned that the full impact of CQI can only be experienced in a physical setting that supports teamwork, as the Household/Neighborhood Model does. The traditional nursing home environment creates subtle barriers to full implementation of CQI even when all the other requirements are met.
6. Collaboration with state of Wisconsin
6.1. Involving state officials
Part of the planning process for the first household/neighborhood was a two-year collaborative effort with the State of Wisconsin to identify and address points of conflict with current state and federal regulations. We laid the ground-work for this collaboration beginning in 1987 when we began the process of informing elected, appointed and career State officials as to what we were doing and involving them in the process. We recognized that their involvement was essential since the environment we wanted to build was very different from anything the State had previously approved.
During the pilot household research project, the Wisconsin Governor and the Secretary of Health and Family Services accepted our invitation to visit. Following this experience, the Secretary had multiple persons from his staff come to see the household because it provided a tangible expression of what federal regulations implemented in 1990 required nursing homes to be. Up to this time, Wisconsin officials had little idea of what the desired skilled nursing facilities might look and feel like.
6.2. Changing regulations
One of the challenges Evergreen and the State jointly addressed was to change a regulation that limited the amount that could be spent per nursing home bed for new construction. This regulation was put in place to limit the amount the State would have to reimburse the nursing home for the care of residents who had insufficient funds. Both Evergreen and the State recognized that the cost per bed for the household/neighborhood would be greater than the limit, but that the value to the residents of living in the new environment was likely to be far greater than the cost. After two years of collaborative work, the State was able to add a provision to the regulation that permitted Evergreen to proceed with project planning.
We also worked closely with the State to identify all the building design regulations where a conflict might exist. Initially, Evergreen and the State jointly developed a list of about 140 potential regulatory conflicts. These were progressively eliminated by: (1) finding the conflict did not actually exist, (2) having the architect make non-substantive changes in the building design, and (3) changing the State׳s interpretation of the regulations. At the end of the process when the project was finally approved by the State, Evergreen had only 4 items of difference with the wording of the regulations, and in all of these situations the design actually exceeded State expectations. In 1996, this radically new building, named Creekview, was the first “demonstration project” approved by the State to evaluate an innovative nursing home design. It was also the first skilled nursing facility in the USA using the household/neighborhood design.
7. Organization structure
7.1. Household/neighborhood organization
Based on the experience with the pilot household, the Evergreen leadership recognized that the household/neighborhood design required a different organization. Since the staff from all disciplines would work together as a neighborhood team, a single manager for the neighborhood was required. After consideration of several disciplines from which the manager could come, the decision was made that the manager needed to be a Registered Nurse because all residents in a skilled nursing facility would have medical issues. However, this RN must have a high level of leadership skills and a strong appreciation for the importance of each of the disciplines involved on the neighborhood team.
In addition to nurses (both Registered and Licensed Practical), one of whom oversees and provides medical services in the neighborhood on each shift, the other disciplines and the number in the neighborhood are: (1) Certified Occupational Therapy Assistant (1 full-time equivalent [FTE] with flexible schedule), who is in charge of resident activities and overall resident functioning; (2) Unit Clerk (1 FTE on weekdays), who coordinates all of the neighborhood clerical responsibilities; (3) Social Worker (1 FTE on weekdays), who coordinates the relationship with families and other social needs; (4) Clinical Specialist (.4 FTE on weekdays), who coordinates all medical services for each resident; (5) Activities Aides (1.4 FTE, 7 days/week), who assist with the planning and execution of resident activities; (6) Exercise Aides (1.4 FTE, 7 days/week) who assist the residents maintain mobility and functioning; (7) Neighborhood Resident Assistant (each shift), who supports the Household RAs; (8) Household Resident Assistant (1 per household on day and evening shifts, and 1 per 2 households at night), who are responsible for all resident services provided in the household during one shift.
7.2. Evergreen organization
After moving into Creekview in mid 1997, it became clear that the change in the neighborhood organization called for a change in the total Evergreen organization structure to become team-based. The change eliminated all traditional departments except Dining Services and Environmental Services (both provide services from a central location to the entire facility). Thus, instead of having 11 functional department heads reporting to the CEO/President, the leadership team consisted of the President and 4 Vice-Presidents – Business Services, Community Services, Quality Services, and Operational Services. All Operational Services (except Dining and Environmental Services) were organized by neighborhoods under the leadership of a Neighborhood Manager. Thus, all traditional functional department directors except for Dining and Environmental Services were eliminated, thereby providing the funds required for more front-line staff in the neighborhood. Over time, staff from the different neighborhoods with the same functional roles developed on-going teams to coordinate their activities.
Because of the large scope of this organization change, it was done through evolution over 4 years, usually as positions became open through normal turnover. While the transition process was stressful because of the large changes in roles and responsibilities, the result proved to be very beneficial and worth all the difficulty encountered.
8. Research evaluation of Creekview
8.1. Research process
As part of the requirements of the State of Wisconsin for approval of Creekview as the first nursing home demonstration project, Evergreen needed to carry out a comprehensive research evaluation of the new environment by an independent research organization. Evergreen was able to obtain funding from foundations and the State of Wisconsin to retain a private research organization to undertake the research.7 All 36 residents who moved to Creekview agreed to be in the experimental research group; a control group was made up of 52 of the 72 residents in the other two traditional units of the Evergreen skilled nursing facility.
Data was collected prior to the move and at 6 months and 12 months following the move. Each collection involved a 4-day visit by a team which did resident, family and staff interviews plus a variety of evaluations of resident behavior, social interactions, and staff documentation. The two groups were examined in two ways: longitudinal (evaluating the same group over time), and cross-sectional (comparing differences between residents who moved to Creekview and those who did not). During the research, the organization structure and the management philosophy were the same for both groups of residents even though the physical settings were very different. Because of the differences in the settings, some differences in operations existed.
8.2. Research findings
Overall, Creekview residents consistently rated higher or better on cognitive, emotional and behavioral indices than residents who remained in the traditional units. One variation from this was that residents who moved to Creekview participated less in activities than the control group, perhaps because residents who wanted more privacy and less participation self-selected to move to Creekview. While the differences between the two groups were not big, the initial ratings for both groups were very high compared to other facilities in Wisconsin so there was not a lot of room for improvement.
8.3. Longer term impact of Creekview
Following are informal findings regarding the impact of Creekview on staff, residents and families during the next few years: (1) nurses preferred working in the household/neighborhood environment because of the team spirit even though the new setting required them to walk more and to be better organized; (2) some Resident Assistants did not like the new work setting, but those who did valued how the household clearly defined the area of responsibility for which they were held accountable, the variety of tasks they were expected to do, and the relationship with the rest of the neighborhood team; (3) residents and their families continued to be willing to pay a 10% premium for Creekview over what they would pay in the traditional units; and (4) Creekview continued to have high occupancy even when the regional demand for nursing home accommodations experienced a substantial drop.
9. Creekview II
9.1. Planning Creekview II
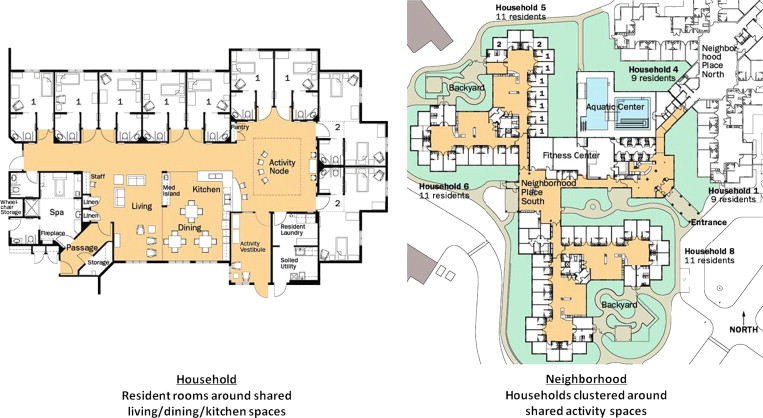
Because of the success of Creekview, the Evergreen governing board decided in 2001 to begin planning for a second Creekview. The planning team was a multi-disciplinary and multi-level group of staff drawn from those involved with the household pilot project and Creekview I. The basic household/neighborhood design was used again since in the 4 years following the opening of Creekview I, the design had proved to be very successful. Figure 2 illustrates the household plan and the neighborhood plan of Creekview II.
|
|
|
Figure 2. Design of Creekview II Household/Neighborhood Model (architect: Nelson-Tremain Partnership). |
One significant change was to increase the size of each household to 11 residents (with two Neighborhood RAs) to permit the conversion of 8 rooms in the original 1967 nursing home from semi-private to private rooms to make them more marketable. This change proved to be undesirable because: (1) 11 residents is too many for one Household Resident Assistant to be accountable for both tasks and relationship development, and (2) 22 residents is too few to keep a Neighborhood RA fully occupied. Therefore, more management of the neighborhood RA staff is required and the RA accountability for a single household is diminished.
Through the experience with Creekview I, many improvements in the design were identified by the front-line staff. Key items were: (1) the documentation and medication work areas, and supply storage do not need to be contiguous so can be dispersed around the household allowing more freedom and creativity in the design; (2) the kitchen and dining areas needed to be larger to provide more counter space and more room for tables; (3) the utility room with the washer/dryer and housekeeping equipment and supplies needed to be increased in size and rearranged; (4) the size of the bathing spa and beauty shop needed to be increased with greater separation between the two functions; and (5) more physical resources to support the provision of meaningful activities for individuals and groups were needed.
9.2. Construction of Creekview II and the influence of the model on others
Construction of Creekview II began in 2003 and was completed in mid 2004. State approval to build was received with ease because the code changes resulting from Creekview I had been institutionalized for other organizations to use. Several long-term care organizations in the state began to draw upon the experience of Evergreen and use variations of the Household/Neighborhood Model which supported the validity of this new approach in the provision of skilled nursing care.
Two examples of the broad influence of the model on other organizations occurred in 1992 during the household pilot project. Following a presentation Evergreen staff made about the household concept at a national conference late that year, representatives from long-term care organizations in Seattle, Washington and Rochester, New York visited the pilot project. Both organizations were rather far along in the design process for a replacement skilled nursing facility using the traditional model; after seeing the pilot project, both organizations made the decision to start over with the design process. This was a very strong affirmation that a new model for skilled nursing facilities was needed. It is fortunate that Evergreen had the opportunity and the will to develop such a model.
10. Utilization of Household/Neighborhood Model in China
10.1. Connecting with developer
In 2007 I did educational presentations about the Creekview model at two conferences which were attended by international participants. At both, a USA developer who wanted to build world-class skilled nursing facilities in China was present and looking for consultants to assist him. After learning about the Household/Neighborhood Model and what Evergreen had done to make it a reality through three iterations, he came to visit Creekview in 2008. In 2009 I was retained as the first USA consultant for China Senior Care, and named Director of Conceptual Planning and Development.
Conceptual designs were created in 2009 and 2010, a site for the first facility was acquired in 2012, and ground was broken in 2013 with the expectation of occupancy in the fall of 2014. This facility will have 8 households with 8 residents each (2 households per floor) in a 5 story building with the neighborhood center on the first floor and parking plus other support resources in the basement. All of the planning and operating processes are designed to be scalable since the objective is to build and operate many facilities based on the Household/Neighborhood Model.
10.2. Incorporation of CQI
Operations will be based on the Continuous Quality Improvement philosophy which was developed by the Toyota Corporation. Since Evergreen began the adoption of CQI in 1990, many more tools for implementation of the philosophy have been developed by Toyota that will be used by China Senior Care (CSC). Another significant difference between implementation of the model at Evergreen and at CSC is that one of the criteria for selection of CSC staff is the ability to work as an effective member of a team and develop personal relationships with residents. While CSC has the challenge of training the staff to work in an organization culture that is different from the culture of the typical Chinese employer, the staff will know in advance that this is a job expectation.
11. Conclusions
The Household/Neighborhood Model is a radical departure from the traditional medical model skilled nursing facility both in the design of the physical setting and in all aspects of operations. The physical setting for the model utilizes small residential living environments called households that are intended to provide residents the resources they associate with “home”. Operations call for a new management philosophy, organization structure, staff roles and training, and approach to activity programming, all based on the concepts of Continuous Quality Improvement.
For Evergreen to be the first long-term care organization in the USA to undertake the total transformation required to create and adopt the model was difficult, time consuming, and called for a long-term commitment by both the governing board and operational leadership. Over time the results strongly confirmed their worth. Being provided the opportunity to take the model to another level in China is very exciting, particularly since we now have a better understanding of how all the elements of the environment must fit together.
Every long-term care organization that desires to provide resident and relationship centered services and care and is still using a traditional medical model of design and operations would benefit from studying the Household/Neighborhood Model to determine when and how to begin the transformation process.
Notes
3. Alton J. DeLong, Philadelphia Geriatric Center (1967); A Preliminary Analysis of the Structural Points of Interpersonal and Environmental Transactions Among the Mentally Impaired Elderly; mimeo report.
4. Ralph Kalies, Ph.D., Oshkosh, WI (1993); Evaluation of the Household Research Project, Evergreen Retirement Community, Oshkosh, WI; unpublished research study.
5. Susan Colgrove, Ph.D. and other faculty of the College of Nursing, University of Wisconsin Oshkosh (1995); a study of the impact of Continuous Quality Improvement; unpublished research study.
6. Edwards Deming, MIT Center for Advanced Engineering Study, Cambridge, MA (1982); Quality, Productivity, and Competitive Position.
7. Margaret P. Calkins, Ph.D., President, I.D.E.A.S., Inc., Cleveland, OH (1999); Creekview: Its History and Evaluation; unpublished research study.
Document information
Published on 12/05/17
Submitted on 12/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?